1/
Thread: Ultrasound for CVC placement - more than just follow the needle tip and confirm the wire.
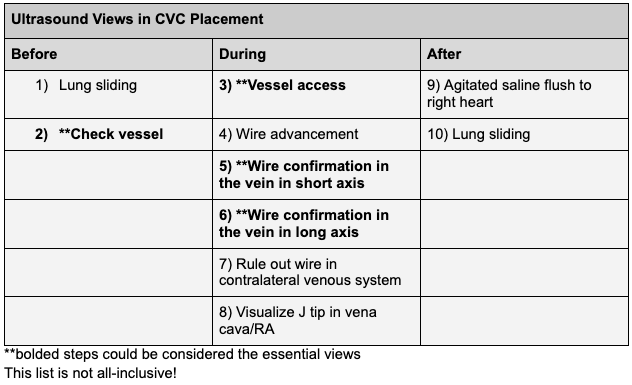
There are many potential uses of ultrasound during CVC placement, shown here. Not all are essential.
#POCUS #IMPOCUS #FOAMED #FOAMUS
Thread: Ultrasound for CVC placement - more than just follow the needle tip and confirm the wire.
There are many potential uses of ultrasound during CVC placement, shown here. Not all are essential.
#POCUS #IMPOCUS #FOAMED #FOAMUS
2/
Pre-procedure
Lung sliding on ipsilateral side - for a comparison to post-procedure
-use linear probe
-apical and lateral/anterior
Pre-procedure
Lung sliding on ipsilateral side - for a comparison to post-procedure
-use linear probe
-apical and lateral/anterior
3/
Check vessel
-confirm compressibility
-understand axis of vessel
-check prox and distal for stenoses
-optimize depth and gain (this image may be undergained)
Check vessel
-confirm compressibility
-understand axis of vessel
-check prox and distal for stenoses
-optimize depth and gain (this image may be undergained)
4/ Vessel access
-Most often done in short axis. Long axis is fine too
-This is the part that requires the most practice
-If not seeing the needle tip, slide probe back/forth while pushing needle back/forth slightly (not advancing needle).
Example of long axis:
-Most often done in short axis. Long axis is fine too
-This is the part that requires the most practice
-If not seeing the needle tip, slide probe back/forth while pushing needle back/forth slightly (not advancing needle).
Example of long axis:
5/
In this case, a nerve bundle is seen! This reminds us of the importance of identifying and avoiding neighboring key structures, such as nerves. Nerve injury has been reported following central venous cannulation.
pubmed.ncbi.nlm.nih.gov/3047455/
In this case, a nerve bundle is seen! This reminds us of the importance of identifying and avoiding neighboring key structures, such as nerves. Nerve injury has been reported following central venous cannulation.
pubmed.ncbi.nlm.nih.gov/3047455/
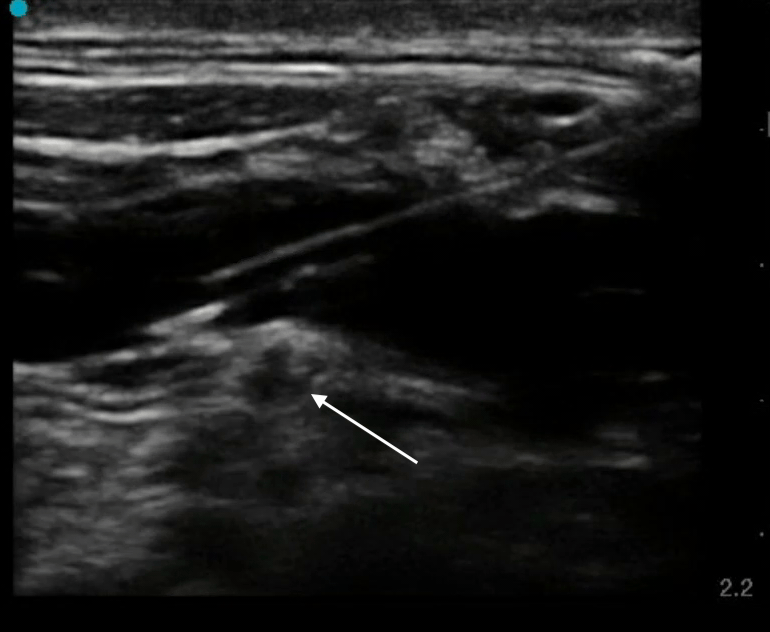
6/
Vessel Access (continued)
When the nerve was noticed to be in a precarious position, the needle was repositioned to avoid accidental nerve injury. Imagine trying to avoid this nerve without ultrasound!
Vessel Access (continued)
When the nerve was noticed to be in a precarious position, the needle was repositioned to avoid accidental nerve injury. Imagine trying to avoid this nerve without ultrasound!
7/ Wire advancement
A common point of attempt failure occurs when probe is dropped and wire is threaded. Slight movement of needle may lead wire to be advanced into tissue rather than vessel. This problem can be avoided by real-time visualization of wire advancement into vessel.
A common point of attempt failure occurs when probe is dropped and wire is threaded. Slight movement of needle may lead wire to be advanced into tissue rather than vessel. This problem can be avoided by real-time visualization of wire advancement into vessel.
8/
Wire advancement (continued)
The wire is seen to pass into the vein smoothly. In this case, the Wire-in-Needle Technique was used. pubmed.ncbi.nlm.nih.gov/26281803/
@HeyDrNik
Wire advancement (continued)
The wire is seen to pass into the vein smoothly. In this case, the Wire-in-Needle Technique was used. pubmed.ncbi.nlm.nih.gov/26281803/
@HeyDrNik
9/
**Wire confirmation in the vein in short axis
-identify vein and artery. Ensure wire in vein.
-scan proximal (closer to heart) and ensure wire is within vessel as far as can be seen
**Wire confirmation in the vein in short axis
-identify vein and artery. Ensure wire in vein.
-scan proximal (closer to heart) and ensure wire is within vessel as far as can be seen
10/
**Wire confirmation in the vein in long axis
-identify vein and artery. Ensure wire in vein.
-scan proximal (closer to heart) and ensure wire is within vessel as far as can be seen
**Wire confirmation in the vein in long axis
-identify vein and artery. Ensure wire in vein.
-scan proximal (closer to heart) and ensure wire is within vessel as far as can be seen
11/
Rule out wire in contralateral venous system (optional, often impractical due to need for use linear probe over non-sterile area). If you do see the wire in contralateral subclavian or IJ (as shown here), withdraw wire to 10 cm and readvance.
Rule out wire in contralateral venous system (optional, often impractical due to need for use linear probe over non-sterile area). If you do see the wire in contralateral subclavian or IJ (as shown here), withdraw wire to 10 cm and readvance.
12/
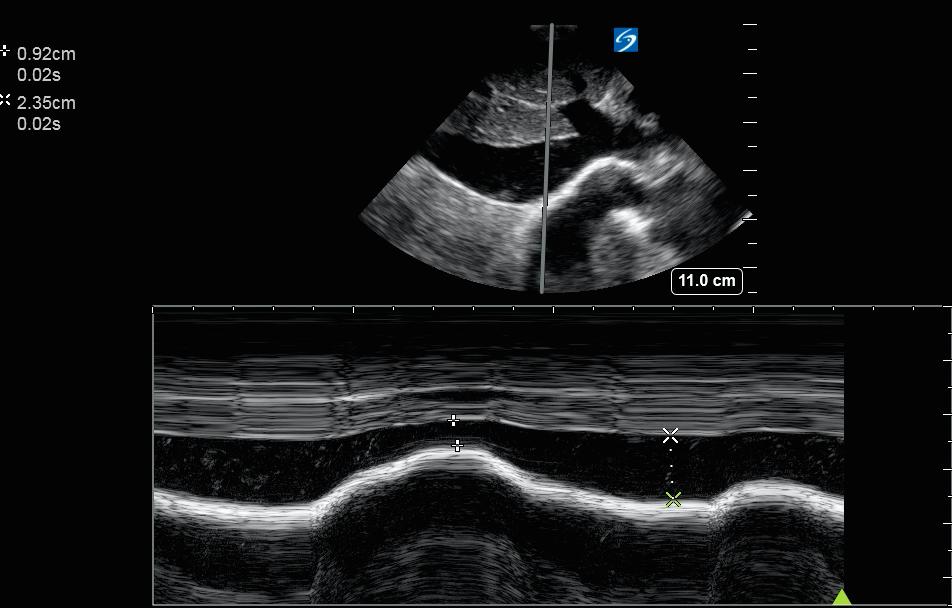
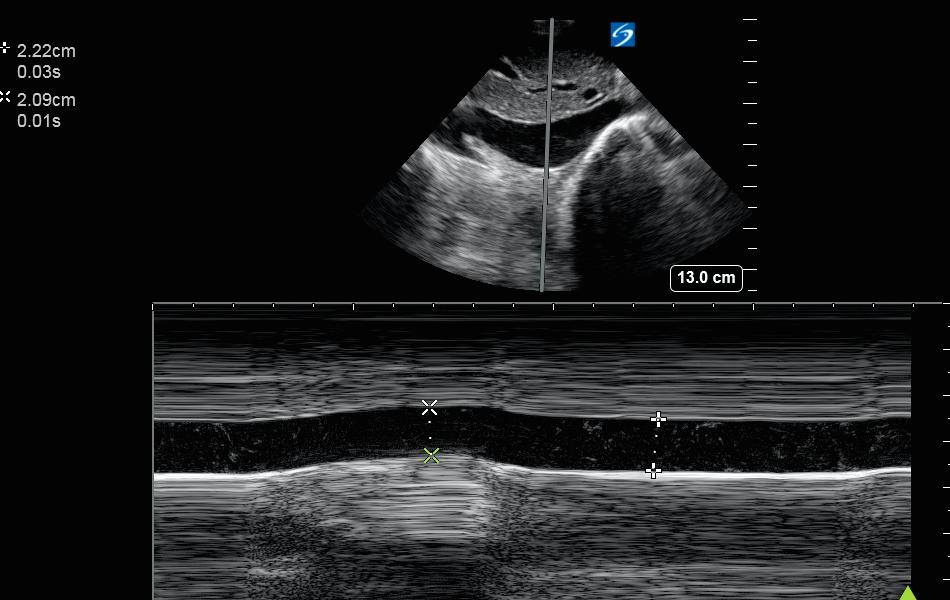
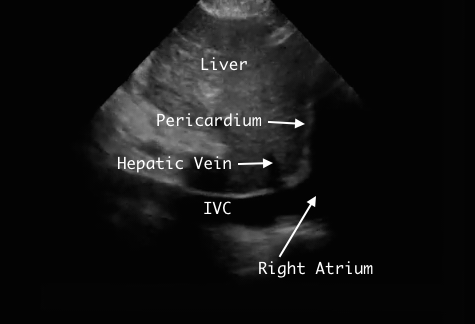
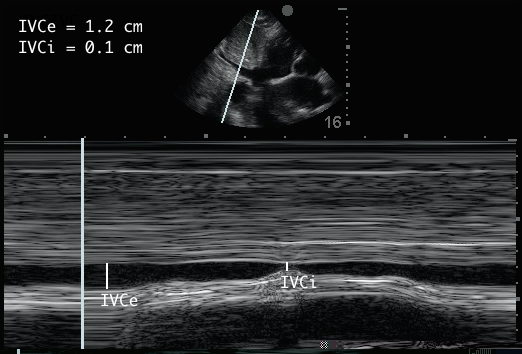
Visualize J tip in cava/RA
This step may prevent venous malpositioning. If wire in SVC/RA, the catheter will go in the right direction. Requires 2nd operator w phased array probe. Can be practical in some settings.
See clip here of J tip at cavoatrial junction
Visualize J tip in cava/RA
This step may prevent venous malpositioning. If wire in SVC/RA, the catheter will go in the right direction. Requires 2nd operator w phased array probe. Can be practical in some settings.
See clip here of J tip at cavoatrial junction
13/
How common is venous malpositioning? and how often can wire be seen well?
Rates ~5-7% of CVC venous malpositioning (most often in contralateral IJ, SC, or innominate). Probably lower for RIJ and higher for SC and LIJ. Preventing this would be useful.
pubmed.ncbi.nlm.nih.gov/17342519/
How common is venous malpositioning? and how often can wire be seen well?
Rates ~5-7% of CVC venous malpositioning (most often in contralateral IJ, SC, or innominate). Probably lower for RIJ and higher for SC and LIJ. Preventing this would be useful.
pubmed.ncbi.nlm.nih.gov/17342519/
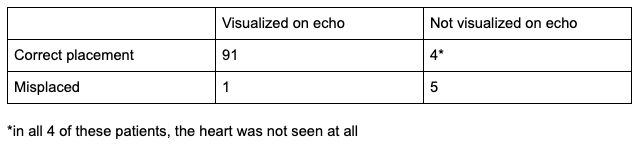
14/
This study pubmed.ncbi.nlm.nih.gov/24052186/
quantified the ability of this technique to detect the wire in the right heart chambers.
When wire not seen, 5/6 were incorrectly placed.
When wire seen, 91/92 correctly placed.
Overall incidence of malpositioning ~6%.

This study pubmed.ncbi.nlm.nih.gov/24052186/
quantified the ability of this technique to detect the wire in the right heart chambers.
When wire not seen, 5/6 were incorrectly placed.
When wire seen, 91/92 correctly placed.
Overall incidence of malpositioning ~6%.

15/
Is it practical? Here is a study that used this strategy and found similar success rates, similar duration of procedure, and reduced time to central line use. journals.sagepub.com/doi/full/10.11…
Not aware of any data showing reduces incidence of venous malpositioning with this method.
Is it practical? Here is a study that used this strategy and found similar success rates, similar duration of procedure, and reduced time to central line use. journals.sagepub.com/doi/full/10.11…
Not aware of any data showing reduces incidence of venous malpositioning with this method.
16/ Back to the CVC images...
Agitated saline flush to right heart. Can be done with a single 10 cc sterile flush after shaking/flicking to induce microbubbles. Note: still be sure to remove MACRObubbles from the syringe (i.e. visible air).
Is CVC ok to use?
No we need a CXR?
Agitated saline flush to right heart. Can be done with a single 10 cc sterile flush after shaking/flicking to induce microbubbles. Note: still be sure to remove MACRObubbles from the syringe (i.e. visible air).
Is CVC ok to use?
No we need a CXR?
17/
This study found an excellent concordance between ultrasound (wire confirmation in vein plus agitated saline) and CXR and suggested CXR may not be needed. journals.lww.com/ccmjournal/Abs…
If you verify +saline flush in RA, what is your approach to CXR and OKing the line?
This study found an excellent concordance between ultrasound (wire confirmation in vein plus agitated saline) and CXR and suggested CXR may not be needed. journals.lww.com/ccmjournal/Abs…
If you verify +saline flush in RA, what is your approach to CXR and OKing the line?
18/
A practice style: ok line based on flush, but still obtain CXR. Flush verifies catheter in venous system, but not necessarily correct position. Others caring for pt may rely on CXR and may not be ok w/o CXR.
Many opinions on this. See emcrit.org/pulmcrit/does-… @PulmCrit
A practice style: ok line based on flush, but still obtain CXR. Flush verifies catheter in venous system, but not necessarily correct position. Others caring for pt may rely on CXR and may not be ok w/o CXR.
Many opinions on this. See emcrit.org/pulmcrit/does-… @PulmCrit
19/
Post-procedure lung sliding (ipsilateral). Again, remember to check multiple points (apex and lateral/anterior)
Post-procedure lung sliding (ipsilateral). Again, remember to check multiple points (apex and lateral/anterior)
20/ An additional method worth knowing for subclavian CVCs is the PART (Pleural avoidance with rib trajectory) method.
Be sure to check it out
ultrasoundpodcast.com/2017/11/part-m…
pubmed.ncbi.nlm.nih.gov/28359216/
@msenussiMD
Be sure to check it out
ultrasoundpodcast.com/2017/11/part-m…
pubmed.ncbi.nlm.nih.gov/28359216/
@msenussiMD
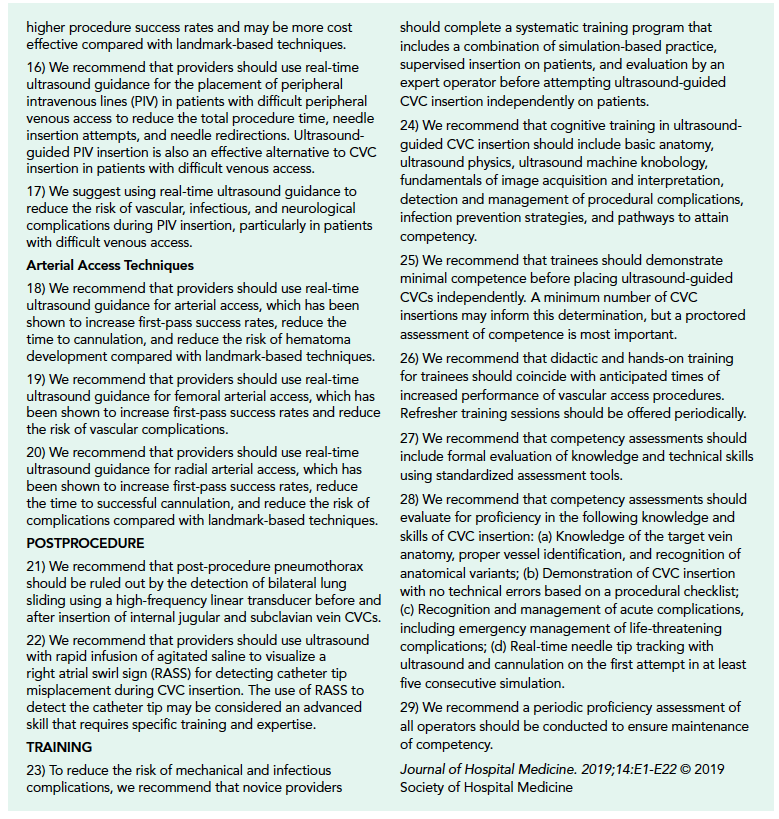
21/
SHM guidelines recommend many of the views shown above
(real time ultrasound for vessel access, wire confirmation, saline flush, and post-procedure lung sliding) journalofhospitalmedicine.com/jhospmed/artic…

SHM guidelines recommend many of the views shown above
(real time ultrasound for vessel access, wire confirmation, saline flush, and post-procedure lung sliding) journalofhospitalmedicine.com/jhospmed/artic…
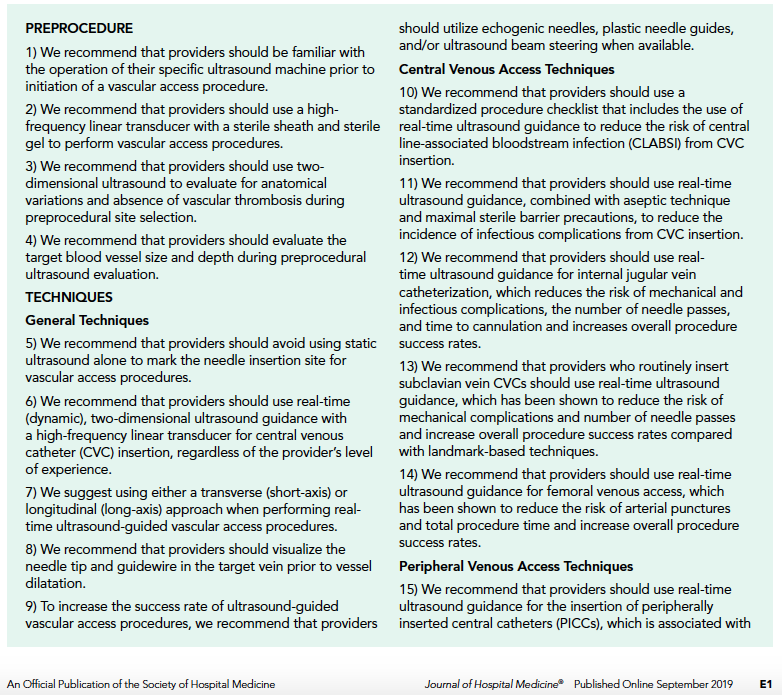
21/
Summary: ultrasound for CVC placement may help
-Reduce # of attempts
-Reduce injury to nearby structures
-Reduce likelihood of arterial placement
-Reduce likelihood of venous malposition
-Verify for earlier “OK to use”
Summary: ultrasound for CVC placement may help
-Reduce # of attempts
-Reduce injury to nearby structures
-Reduce likelihood of arterial placement
-Reduce likelihood of venous malposition
-Verify for earlier “OK to use”
22/ Interested to hear thoughts of others, any more tips/tricks on ultrasound and CVCs?
@msenussiMD @iceman_ex @kyliebaker888 @collinflan @katiewiskar @Wilkinsonjonny @siddharth_dugar @ria_dancel @MDbenji @ArgaizR @RogerAlvarezDO @laxswamy @emily_fri @cameron_baston @hraza222
@msenussiMD @iceman_ex @kyliebaker888 @collinflan @katiewiskar @Wilkinsonjonny @siddharth_dugar @ria_dancel @MDbenji @ArgaizR @RogerAlvarezDO @laxswamy @emily_fri @cameron_baston @hraza222
@bryanboling @virenkaul @pedrodammert @criticalcareuk
@redneeraj @ccpractitioner @ThinkingCC @cianmcdermott @jtanguay11 @TimRowesays @jelevenson @khldtaha @DRsonosRD @NephroP @DrGalenMD @buckeye_sanjay @Cometin007 @ScottTiltonCRNP @jminardi21 @drshahrul80 @JCHCheung
@redneeraj @ccpractitioner @ThinkingCC @cianmcdermott @jtanguay11 @TimRowesays @jelevenson @khldtaha @DRsonosRD @NephroP @DrGalenMD @buckeye_sanjay @Cometin007 @ScottTiltonCRNP @jminardi21 @drshahrul80 @JCHCheung
This was supposed to say "Do we need a CXR?"
• • •
Missing some Tweet in this thread? You can try to
force a refresh