1/#tweetorial coagulopathy in liver disease and the role of vit K
Thanks to all who responded to the poll.
Thanks to all who responded to the poll.
https://twitter.com/AnnKumfer/status/1338939315586523139?s=20
2/ Pts with cirrhosis are at higher risk of bleeding d/t ⬇️ factors, right? Not necessarily. In cirrhosis, there are ⬇️ in both anticoagulant and procoagulant factors in the liver. Additionally, factor VIII and VWF are usually increased. 

3/ INR is only measuring a small part of the coagulation cascade, the extrinsic pathway (Factor VII). Additionally, variceal bleed is driven by ⬆️ portal pressure primarily.
4/ Study of patients with cirrhosis showed that there was no significant difference of VTE risk between INR quarterlies. ⬆️ INR was not protective against VTE.
pubmed.ncbi.nlm.nih.gov/20040609/
pubmed.ncbi.nlm.nih.gov/20040609/
5/ TWDFNR suggested against checking/correcting INR prior to routine paracentesis.
journalofhospitalmedicine.com/jhospmed/artic…
journalofhospitalmedicine.com/jhospmed/artic…
6/ Things like thromboelastography (TEG) have been shown to ⬇️ blood product usage in variceal bleed (pubmed.ncbi.nlm.nih.gov/31148204/) but has not been shown to predict long-term mortality (pubmed.ncbi.nlm.nih.gov/32722691/) . TEG may be used more in future in defining bleeding vs vte risk.
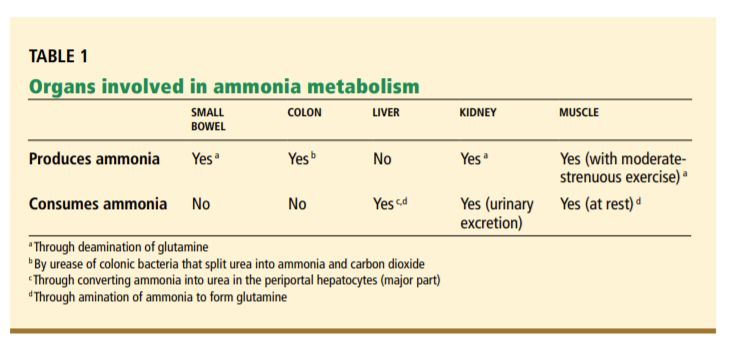
7/ A brief review table from the below article posted by @k_vaishnani.
Summary: Pts with cirrhosis can have increased bleeding or clotting risk that is difficult to assess with standard coagulation factors.
journals.lww.com/ajg/Abstract/2…
Summary: Pts with cirrhosis can have increased bleeding or clotting risk that is difficult to assess with standard coagulation factors.
journals.lww.com/ajg/Abstract/2…

• • •
Missing some Tweet in this thread? You can try to
force a refresh