A tweetorial on optimal machine settings for B line image acquisition, with a focus on: focal position at pleura, harmonics off, and increased far gain.
Inspired/based on the recent article - onlinelibrary.wiley.com/doi/full/10.10…
@cameron_baston @IsaacMatthiasM1
#POCUS #IMPOCUS
1/18
Inspired/based on the recent article - onlinelibrary.wiley.com/doi/full/10.10…
@cameron_baston @IsaacMatthiasM1
#POCUS #IMPOCUS
1/18
Let's start with some polls
We will stick to low frequency probes here (i.e. curvilinear and phased array - linear has its own purpose for detailed pleural assessment)
Which preset do you prefer for B line assessment?
2/
We will stick to low frequency probes here (i.e. curvilinear and phased array - linear has its own purpose for detailed pleural assessment)
Which preset do you prefer for B line assessment?
2/
What depth do you typically set?
3/
3/
After selecting preset and selecting depth, do you ever adjust any other machine settings to optimize B line assessment?
4/
4/
Importantly, there is no right answer to the above questions!
We won't discuss much about preset or probe type. But we will discuss machine settings to optimize B line quality, based on
1) Theory based on physical basis of B lines
2) In vitro study
3) Study in patients
5/
We won't discuss much about preset or probe type. But we will discuss machine settings to optimize B line quality, based on
1) Theory based on physical basis of B lines
2) In vitro study
3) Study in patients
5/
To start with the theoretical basis:
B lines are
1) reverberation artifacts
2) formed from the pleural interface when the interstitium is thickened
3) span the full depth of the field
See explanation in tweetorial on ABCs of lung ultrasound here
6/
B lines are
1) reverberation artifacts
2) formed from the pleural interface when the interstitium is thickened
3) span the full depth of the field
See explanation in tweetorial on ABCs of lung ultrasound here
https://twitter.com/IMPOCUSFocus/status/1177700689365147649?s=20
6/
1) Artifact
Tissue harmonic imaging is a technology designed to minimize artifact. In theory, harmonics being "on" may reduce B line quantity. The same idea applies for cardiac presets, which tend to minimize artifact.
(Notably, there is conflicting literature here)
7/
Tissue harmonic imaging is a technology designed to minimize artifact. In theory, harmonics being "on" may reduce B line quantity. The same idea applies for cardiac presets, which tend to minimize artifact.
(Notably, there is conflicting literature here)
7/
2) Formed at the pleural interface
Thus it would make sense to put the focus at the pleural line. The focal position is the depth at which lateral resolution is highest, so interstitial thickening is more likely to be detected w pleural at focal position.
Here, focus at 10 cm
8/
Thus it would make sense to put the focus at the pleural line. The focal position is the depth at which lateral resolution is highest, so interstitial thickening is more likely to be detected w pleural at focal position.
Here, focus at 10 cm
8/
Same site, but focus moved to pleura. Improved lateral resolution at the pleural line brings out more B lines.
9/
9/
3) B lines Span the full depth of the field
Often the brightness of B lines fades deeper into the image due to loss of energy with subsequent reverberations. Increasing the far gain can theoretically improve ease of visualizing B lines in the far field (as shown here).
10/
Often the brightness of B lines fades deeper into the image due to loss of energy with subsequent reverberations. Increasing the far gain can theoretically improve ease of visualizing B lines in the far field (as shown here).
10/
Study using in-vitro B line model (tetrahedral air bubbles) found better quality w
-focus at pleura
-more far-gain
-lung preset (vs abd)
Did not acheive significance for "harmonics off"
Limitations: one machine (Sparq), needs further study in pts.
pubmed.ncbi.nlm.nih.gov/31089845/
11/

-focus at pleura
-more far-gain
-lung preset (vs abd)
Did not acheive significance for "harmonics off"
Limitations: one machine (Sparq), needs further study in pts.
pubmed.ncbi.nlm.nih.gov/31089845/
11/


Back to the article that inspired the thread. onlinelibrary.wiley.com/doi/full/10.10…
This study sought to test if adjusted settings (developed based on in-vitro experiments) were associated change in perceived quality (and quantity) of B lines.
12/
This study sought to test if adjusted settings (developed based on in-vitro experiments) were associated change in perceived quality (and quantity) of B lines.
12/
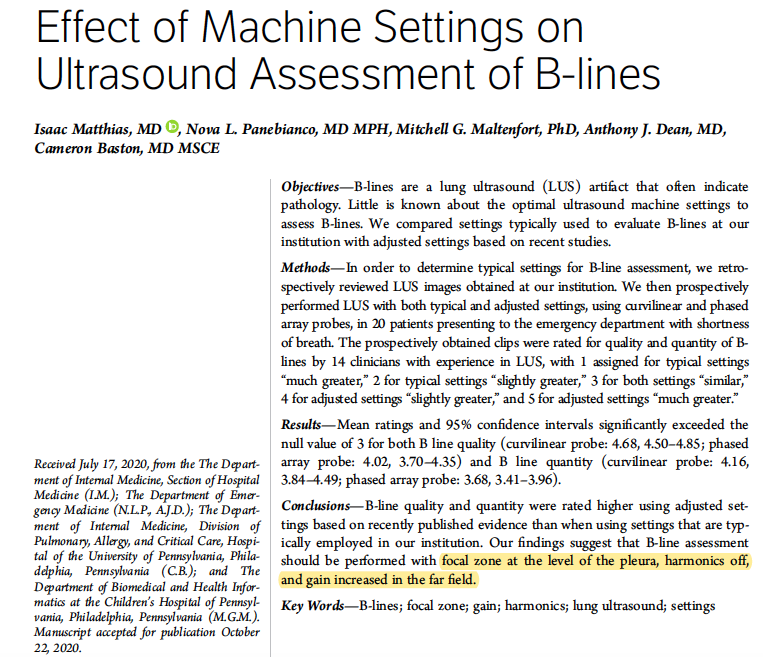
Adjusted settings were defined as focus at pleural line, harmonics off, and time gain compensation increased linearly in the far field.
In a retrospective study, most exams resembled the typical settings (and cardiac was most common preset).
13/
In a retrospective study, most exams resembled the typical settings (and cardiac was most common preset).
13/

In the prospective study, reviewers (>100 prior lung ultrasound exams) were shown side by side clips of typical v adjusted settings (side randomized) and were asked to grade the quality and quantity of each.
Adj settings were reported to have better quality in ~97% of cases
14/

Adj settings were reported to have better quality in ~97% of cases
14/


Conclusions
Though more data is needed, it seems reasonable that for B line assessment:
1) focus set at pleural line
2) harmonics off
3) increased fair gain
Limitations: these were studied as a bundle (not individual). Study not designed to compare probes or presets.
15/
Though more data is needed, it seems reasonable that for B line assessment:
1) focus set at pleural line
2) harmonics off
3) increased fair gain
Limitations: these were studied as a bundle (not individual). Study not designed to compare probes or presets.
15/
Why does this matter?
1) Consistency is important, in both clinical practice and in research.
2) The utility of B lines lies in their high sensitivity for interstitial edema. If settings are suboptimum and limit sensitivity, that reduces the power of the B line assessment.
16/
1) Consistency is important, in both clinical practice and in research.
2) The utility of B lines lies in their high sensitivity for interstitial edema. If settings are suboptimum and limit sensitivity, that reduces the power of the B line assessment.
16/
Other points on B line acquisition
-remember to find the most perpendicular angle to the pleural line. Otherwise you may end up with a non-A non-B pattern, which is non-diagnostic.
-if ribs are obscuring view, can turn probe to remove ribs from view.
17/
-remember to find the most perpendicular angle to the pleural line. Otherwise you may end up with a non-A non-B pattern, which is non-diagnostic.
-if ribs are obscuring view, can turn probe to remove ribs from view.
17/
After considering the above data and discussion, will you adjust machine settings for B line assessment?
18/
18/
Thanks for reading, interested to hear all thoughts on experiences w B line assessment!
Tagging a few #POCUS friends @kyliebaker888 @iceman_ex @msenussiMD @cameron_baston @Manoj_Wickram @DRsonosRD @NephroP @ArgaizR @ria_dancel @hraza222 @ThinkingCC @Wilkinsonjonny @katiewiskar
Tagging a few #POCUS friends @kyliebaker888 @iceman_ex @msenussiMD @cameron_baston @Manoj_Wickram @DRsonosRD @NephroP @ArgaizR @ria_dancel @hraza222 @ThinkingCC @Wilkinsonjonny @katiewiskar
• • •
Missing some Tweet in this thread? You can try to
force a refresh