
Here is the #PedsICU #BestOf2020 collection.
Jointly chosen by
@Dr_Hari_Krishna @sgdambrauskas and myself
Pubmed collection 40 articles: bit.ly/pedsicubestof2…
Infographic (clickable PDF) in English: bit.ly/bestof2020eng
Spanish: bit.ly/bestof2020esp
#PedsCICU #NeuroPICU

Jointly chosen by
@Dr_Hari_Krishna @sgdambrauskas and myself
Pubmed collection 40 articles: bit.ly/pedsicubestof2…
Infographic (clickable PDF) in English: bit.ly/bestof2020eng
Spanish: bit.ly/bestof2020esp
#PedsCICU #NeuroPICU

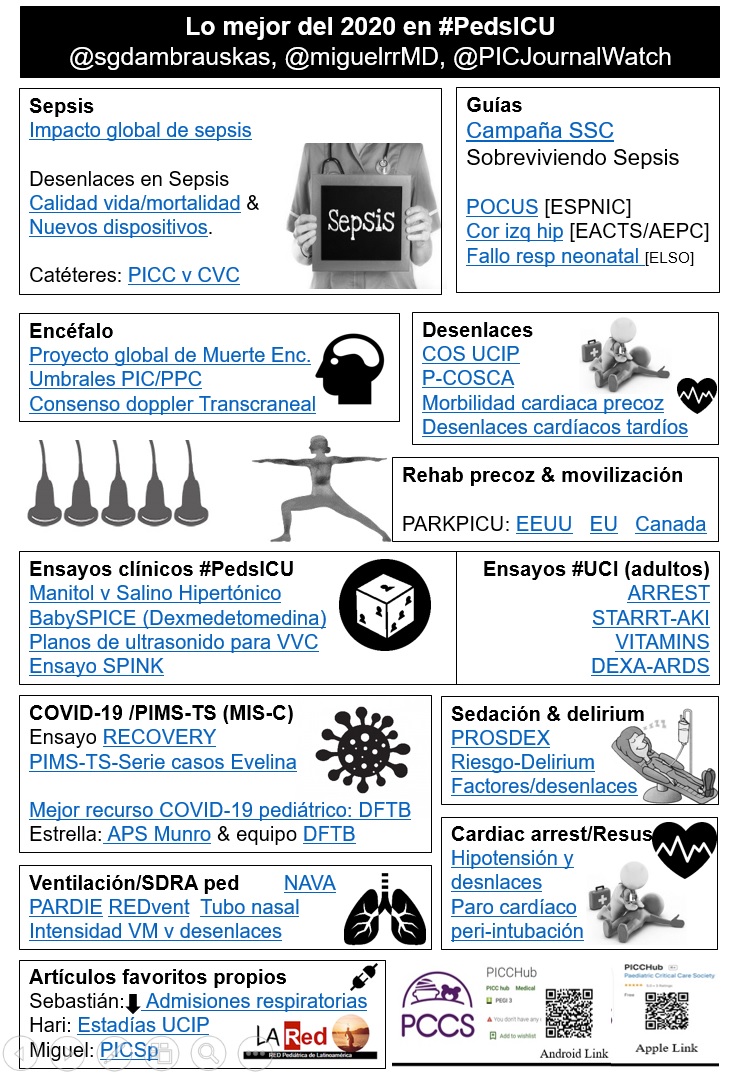
This will be a bilingual tweetorial in Spanish/English!
Infographics are available in both languages in Tweet #1
El hilo será en Español/Inglés. El resumen infográfico está disponible en los dos idiomas en el primer Tweet
Infographics are available in both languages in Tweet #1
El hilo será en Español/Inglés. El resumen infográfico está disponible en los dos idiomas en el primer Tweet
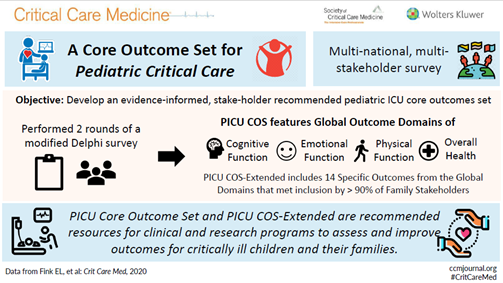
1/What are the outcomes that matter to children, to families and to #researchers/clinicians? @ericka_fink et al & @PostPICU_PALISI investigators identified COS using a delphi process. @CritCareMed bit.ly/381cfq8. Developmental and functional outcomes were important. 
2/ ¿Salino hipertónico o manitol en infecciones SNC? Gracias a este ensayo clínico sabemos que el salino hipertónico disminuye más la PIC que el manitol.
Rameshkumar R et al @drarunbansal 🇮🇳
@PedCritCareMed: bit.ly/3htjdYg
#neuroPICU #PedsICU
¿Cuál es tu práctica?
Rameshkumar R et al @drarunbansal 🇮🇳
@PedCritCareMed: bit.ly/3htjdYg
#neuroPICU #PedsICU
¿Cuál es tu práctica?
3/ @EsangbedoIvie et al: peri-intubation #CardiacArrest in #PedsCICU published in @PedCritCareMed: bit.ly/2KDxdCV
Systolic dysfunction of the systemic ventricle, hypotension, pre-intubation lactate ⬆️, lower pH, and oxygen desaturations appeared to be risk factors.
Systolic dysfunction of the systemic ventricle, hypotension, pre-intubation lactate ⬆️, lower pH, and oxygen desaturations appeared to be risk factors.
4/ Autorías relacionadas al género en ensayos clínicos controlados #PedsICU
La muestra indica que aún hay muchísimo por mejorar. Necesitamos màs
#heforshe #sheforshe #PedsICU
@GraceMXu @samara_samzav et al @M_Duffett 🇨🇦
@PedCritCareMed: bit.ly/3pBy6uA
La muestra indica que aún hay muchísimo por mejorar. Necesitamos màs
#heforshe #sheforshe #PedsICU
@GraceMXu @samara_samzav et al @M_Duffett 🇨🇦
@PedCritCareMed: bit.ly/3pBy6uA

5/ ¿Qué valores de PIC y PCC se asocian a mejores resultados en #PedsICU #NeuroPICU?
Trabajo Woods K et al @Pat_Kochanek 🇺🇸
@PedCritCareMed: bit.ly/2WYCJCB
Trabajo Woods K et al @Pat_Kochanek 🇺🇸
@PedCritCareMed: bit.ly/2WYCJCB
6/ The #ARREST trial showed that #ECPR saves lives in select adult patients. Incredibly difficult trial to pull off by @DYannopoulos and colleagues.
@TheLancet: bit.ly/2MgJ75X
#ECMO
@TheLancet: bit.ly/2MgJ75X
#ECMO
7/ @hotz_justin y @RobyKhemaniMD muestran en este estudio que un protocolo de ventilación mecánica basado en la valoración en tiempo real del esfuerzo del paciente es factible y puede acortar el tiempo de ventilación.
En @PedCritCareMed bit.ly/37ZMpmH
#PedsICU #SoMe4MV
En @PedCritCareMed bit.ly/37ZMpmH
#PedsICU #SoMe4MV
8/ Relevant study from Allison Shevell et al (@sickkids 🇨🇦) published in @PedCritCareMed: bit.ly/3n6Ub2w
Several post-op #PedsCICU factors may help identify children at risk of worse neurodevelopmental outcomes in the long run.
#PedsICU
Several post-op #PedsCICU factors may help identify children at risk of worse neurodevelopmental outcomes in the long run.
#PedsICU
9/ Eje largo, en plano. Esta parece ser la mejor manera de evitar perforar el vaso al colocar un catéter venoso central. Comparado con eje corto, fuera de plano, la tasa de éxito al primer intento fue similar.
Takeshita et al en @PedCritCareMed: bit.ly/2L4twWz
Takeshita et al en @PedCritCareMed: bit.ly/2L4twWz
10/ The PARK-PICU projects led by @SapnaKmd aimed to establish the prevalence of acute rehabilitation in the #PedsICU around the world. Results published in @PedCritCareMed @CritCareMed @Crit_Care
bit.ly/3pzYKUr bit.ly/2MmntNN bit.ly/2KFj4oR
#ICURehab
bit.ly/3pzYKUr bit.ly/2MmntNN bit.ly/2KFj4oR
#ICURehab

11/ Gran trabajo de @LA_Rednetwork liderado por @pvasquezcolpicu mostrando la disminución de ingresos en #PedsICU por infecciones respiratorias durante la pandemia #COVID19 en @ADC_BMJ: bit.ly/37Wmk7Y 

12/ @AlexisTopjian et al @BarneyUoB @ericka_fink #OpenAccess in @CircAHA: bit.ly/38L0WBH
Pediatric COS after #CardiacArrest. This article includes information related to actual tools such as PedsQL, GOSE-Ped, PCPC, FSS, VABS etc.and timing of assessments.
#PedsICU
Pediatric COS after #CardiacArrest. This article includes information related to actual tools such as PedsQL, GOSE-Ped, PCPC, FSS, VABS etc.and timing of assessments.
#PedsICU
13/ The World Brain Death Project, un proyecto global que busca homogeneizar la práctica en torno al diagnóstico de muerte por criterios neurológicos.
Greer et al @JAMA_current: bit.ly/2WXHigs
Interesante vídeo acompañante: edhub.ama-assn.org/jn-learning/vi…
#PedsICU #braindeath
Greer et al @JAMA_current: bit.ly/2WXHigs
Interesante vídeo acompañante: edhub.ama-assn.org/jn-learning/vi…
#PedsICU #braindeath
14/ NAVA seemed to shorten the length of mechanical ventilation in adult patients in the #NAVIATOR trial. I'd love to see results replicated in #PedsICU with #sedation and #delirium endpoints as well!
Kacmarek et al @yourICM: bit.ly/3n7i368
#SoMe4MV
Kacmarek et al @yourICM: bit.ly/3n7i368
#SoMe4MV
15/ Guías para el manejo de niños y neonatos con ventrículo izquierdo hipoplásico. #PedsICU #PedsCICU #PedsCards
Alphonso et al @EACTS_Journals: bit.ly/3o0VCAP
Alphonso et al @EACTS_Journals: bit.ly/3o0VCAP
16/ #BabySPICE, a pilot RCT exploring the usefulness and safety of dexmedetomidine as a primary sedative agent in #PedsICU patients requiring light #sedation. Results warrant a bigger RCT to answer this question!
Erickson, @deblong_picu @PedCritCareMed: bit.ly/3pCdkL6
Erickson, @deblong_picu @PedCritCareMed: bit.ly/3pCdkL6
17/ Los #PICCs no parecen reducir el riesgo de tromboembolismo o bacteriemia asociada a catéter comparados con los catéteres venosos centrales.
#CLABSI #DVT #PedsICU
Patel et al @CritCareMed: bit.ly/2L4mW2u
#CLABSI #DVT #PedsICU
Patel et al @CritCareMed: bit.ly/2L4mW2u
18/ Should we be looking at INTENSITY instead of length of mechanical ventilation? Interesting study in adults by @martin_urner et al @efan75 🇨🇦 @LancetRespirMed: bit.ly/2JyuZnD
#SoMe4MV
#SoMe4MV
19/ When everyone was throwing everything they had at patients with #COVID19, researchers in 🇬🇧 were randomizing patients. RECOVERY is the result. Not only did they find that dexamethasone was saving lives but also helped ditch several useless or harmful interventions! (Cont.)
19 bis/ Paper published by @PeterHorby @UniofOxford @MartinLandray in @NEJM: bit.ly/3rEg0d9
Great infographic by @VCCPharmD
Great infographic by @VCCPharmD

20/ (half way through!) Uno de los lemas del #zentensivist: antes no es necesariamente mejor, y esto se aplica también a las terapias de sustitución renal.
#STARRTAKI trial por Bagshaw et al @NEJM: bit.ly/3pC9HoI
Infográfico por @DTomacruzMD
#STARRTAKI trial por Bagshaw et al @NEJM: bit.ly/3pC9HoI
Infográfico por @DTomacruzMD

21/ Again morbidity instead of mortality. Higher risk of morbidity in neonates, complex congenital heart disease, increased preoperative severity of illness and with prolonged bypass.
@katebrown220 et al @NIHRresearch: bit.ly/3aWpo5S
#PedsICU #PedsCICU #PedsCards
@katebrown220 et al @NIHRresearch: bit.ly/3aWpo5S
#PedsICU #PedsCICU #PedsCards
22/ Estudio #PROSDEX de @FraSperotto explorando el uso prolongado de dexmedetomidina en #PedsICU. Nadie mejor que su autora para explicarlo:
@PedCritCareMed: bit.ly/380dvtS
https://twitter.com/FraSperotto/status/1289251088059846658?s=20
@PedCritCareMed: bit.ly/380dvtS
23/ FREE paper in @PedCritCareMed. How often do we use nasal intubation and how does it relate to outcomes? Does it reduce the risk of unplanned extubations? See for yourselves!
Christian et al: bit.ly/38U246l
#PedsICU #SoMe4MV
Christian et al: bit.ly/38U246l
#PedsICU #SoMe4MV
24/ GRATIS en @CritCareMed. Los investigadores de #PARDIE describen modelos predictivos de mortalidad en #pARDS implementables desde el momento del diagnóstico.
Yehya, @RBC_PICU, @DrHeidiFlori, @Martin_Kneyber, @RobyKhemaniMD and @NJThomas6: bit.ly/3rHPLlT
#SoMe4MV
Yehya, @RBC_PICU, @DrHeidiFlori, @Martin_Kneyber, @RobyKhemaniMD and @NJThomas6: bit.ly/3rHPLlT
#SoMe4MV
25/ Primera serie de casos describiendo el #PIMSTS #MISC publicada en @TheLancet por los compañeros de @STRS_Evelina. Esta publicación alertó de una nueva y grave presentación de la enfermedad que afortunadamente es infrecuente.
Riphagen et al: bit.ly/3pBVyrj
Riphagen et al: bit.ly/3pBVyrj
26/ Excellent work by @APSMunro & @DFTBubbles team. Outstanding resources for pediatric #COVID19:
1) dontforgetthebubbles.com/evidence-summa…
2) @apsmunro et al @ADC_BMJ: bit.ly/3839Bk4
1) dontforgetthebubbles.com/evidence-summa…
2) @apsmunro et al @ADC_BMJ: bit.ly/3839Bk4
27/ Guidelines for the management of neonatal respiratory failure by @ELSOOrg.
Wild et al @asaiojournal: bit.ly/2KJyMiK
#PedsICU #ECMO #ECLS
Wild et al @asaiojournal: bit.ly/2KJyMiK
#PedsICU #ECMO #ECLS
28/ 5% de los niños que sobreviven a la sepsis lo hacen con traqueostomía, gastrostomía, acceso vascular o amputaciones. Como muestra el siguiente estudio, sobrevivir a la #sepsis es solo el primer paso #PICSp
@ErinCarlton et al @CritCareMed: ow.ly/q5RB50zlpgX
@ErinCarlton et al @CritCareMed: ow.ly/q5RB50zlpgX

29/ Life after pediatric critical illness can be challenging and #sepsis is no different. Although mortality remains low, more than ⅓ of survivors suffer from an impaired quality of life even at 1 year post discharge.
@jerjohzimm et al in @CritCareMed: bit.ly/3rFzONg
@jerjohzimm et al in @CritCareMed: bit.ly/3rFzONg
30/ #POCUS has come to stay and is slowly growing into the hearts of the #PedsICU community. In February, an international panel of experts with the support of @ESPNIC_Society, issued a series of 39 recommendations.
Singh et al in @Crit_Care: bit.ly/2PWfFRF
Singh et al in @Crit_Care: bit.ly/2PWfFRF
31/ Antes que RECOVERY estuvo DEXA-ARDS. Ensayo clínico español publicado en marzo que mostró que la dexametasona puede disminuir hasta un 15% la mortalidad de los pacientes con #ARDS.
Trabajo publicado por Jesús Villar, @aon_jose et al @LancetRespirMed: bit.ly/2HnvBYN
Trabajo publicado por Jesús Villar, @aon_jose et al @LancetRespirMed: bit.ly/2HnvBYN

32/ Another landmark publication. In addition to 77 comprehensive recommendations related to sepsis management, the #SSC campaign published an algorithm that distinguished “suspected sepsis” v “septic shock”: Weiss, @pus27 et. al @PedCritCareMed: bit.ly/2Jy34UZ
32 bis/ 1) 40-60 mL/Kg iv bolus in 10-20mL/kg aliquots 2) advanced hemodynamic variables and lactate trends, 3) Epi > dopa, 4) Basic #pARDS management.
33/ After ROSC, the time a child spends hypotensive may be related with survival!
Laverriere, @VinayMNadkarni, @AlexisTopjian et al @PedCritCareMed: bit.ly/3hzhBwi
Laverriere, @VinayMNadkarni, @AlexisTopjian et al @PedCritCareMed: bit.ly/3hzhBwi

34/ En niños en #ECMO, el volumen de transfusión de plaquetas parece asociarse con un aumento de la mortalidad, el sangrado y la trombosis.
Cashen, @HeidiDalton26, et al. @PedCritCareMed: bit.ly/3o2C8f1
Cashen, @HeidiDalton26, et al. @PedCritCareMed: bit.ly/3o2C8f1

35/ In 2017 #sepsis hit over 48 million people causing 11 million deaths that were unequally distributed with a highest burden in #LMICs.
Rudd, @NiranjanKissoon, @FlaviaSepsis, et al. @TheLancet: bit.ly/3aWZCOX
Rudd, @NiranjanKissoon, @FlaviaSepsis, et al. @TheLancet: bit.ly/3aWZCOX

36/ The #SPINK trial compared Plasmalyte and 0.9% saline as initial fluid for children with #DKA and found no differences in: incidence of #AKI, time to resolution of #DKA, mortality, length of stay or need for #RRT.
@Vijaiwilliams et al. @Crit_Care: bit.ly/3huewgV
@Vijaiwilliams et al. @Crit_Care: bit.ly/3huewgV
37/ En este estudio se muestra que las benzodiacepinas, la ventilación mecánica o las sujeciones son factores de riesgo para #delirium en #PedsICU. Los días de delirium se asociaron con deterioro cognitivo tras el alta
@LeslieDervan et al. @PedCritCareMed: bit.ly/3pzYKDW
@LeslieDervan et al. @PedCritCareMed: bit.ly/3pzYKDW

38 (THE END!)/ Datos de los últimos años muestran que el número de niños que pasan > 28 días en UCIP en 🇬🇧 ha aumentado de manera importante. Esto puede tener importantes consecuencias logísticas. Trabajo de @Dr_Hari_Krishna @barneyUoB en @ADC_BMJ: bit.ly/3o625dz
@threadreaderapp please urnoll!
Most of the wonderful #VisualAbstracts in this thread are the work of the brilliant @traependergrast!
• • •
Missing some Tweet in this thread? You can try to
force a refresh


