1/
Let's kick off the new year with a #dermatology #tweetorial! I put together some tweets on
#MELANOMA
#MedEd #FOAMEd #medtwitter #dermtwitter #onctwitter
Let's start with a poll:
Among BOTH males and females in the US, how common is melanoma?
Let's kick off the new year with a #dermatology #tweetorial! I put together some tweets on
#MELANOMA
#MedEd #FOAMEd #medtwitter #dermtwitter #onctwitter
Let's start with a poll:
Among BOTH males and females in the US, how common is melanoma?
2/
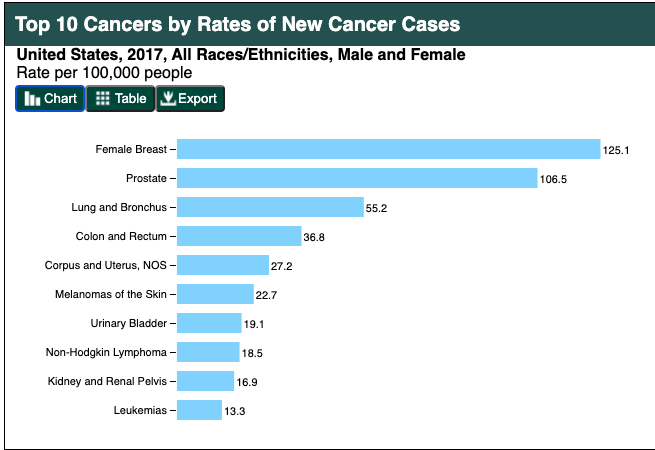
Melanoma is the 6th most common malignancy (that's tracked) for BOTH men & women. Basal cell carcinoma is actually the MOST common cancer in the US, but we don't track it.
While melanomas are 6th, in certain groups (eg: women age 25-30), it is the #1 cause of cancer death!
Melanoma is the 6th most common malignancy (that's tracked) for BOTH men & women. Basal cell carcinoma is actually the MOST common cancer in the US, but we don't track it.
While melanomas are 6th, in certain groups (eg: women age 25-30), it is the #1 cause of cancer death!
3/
So melanoma is deadly, especially in certain age groups. But something peculiar is happening too. @AdeAdamson recently spoke at @MassGeneralNews about this interesting finding 👉 melanoma diagnosis is increasing, but melanoma death is decreasing.
So melanoma is deadly, especially in certain age groups. But something peculiar is happening too. @AdeAdamson recently spoke at @MassGeneralNews about this interesting finding 👉 melanoma diagnosis is increasing, but melanoma death is decreasing.
https://twitter.com/AdeAdamson/status/1334155101351649280?s=20
4/
WHY that is happening is controversial. Some of it (as @AdeAdamson) pointed out, may be because of new therapies (eg: immunotherapy). But, it's not enough to account for it all. Better surveillance? overdiagnosis? 🧐
I'mma back away slowly & keep going with my tweetorial😅
WHY that is happening is controversial. Some of it (as @AdeAdamson) pointed out, may be because of new therapies (eg: immunotherapy). But, it's not enough to account for it all. Better surveillance? overdiagnosis? 🧐
I'mma back away slowly & keep going with my tweetorial😅
5/
Clinically speaking, we look for the moles that fit the ABCDEs:
Asymmetry
Border (irregular)
Color (atypical)
Diameter (>6mm)
Evolving
I also add an F for "Funny looking/Freaky." Basically, a mole that looks different than the rest (which we also call Ugly Duckling Sign)!
Clinically speaking, we look for the moles that fit the ABCDEs:
Asymmetry
Border (irregular)
Color (atypical)
Diameter (>6mm)
Evolving
I also add an F for "Funny looking/Freaky." Basically, a mole that looks different than the rest (which we also call Ugly Duckling Sign)!

6/
But what about in skin of color? While melanoma is less common overall, ACRAL melanomas in particular are a concern in your darker skinned patients.
So if you're a #primarycare doctor/NP, make sure you have your patients kick off their shoes and take a peek there too!
But what about in skin of color? While melanoma is less common overall, ACRAL melanomas in particular are a concern in your darker skinned patients.
So if you're a #primarycare doctor/NP, make sure you have your patients kick off their shoes and take a peek there too!

7/
Risk factors:
1 - Genetics (ex: CDKN2A)
2 - UV exposure (for some populations)
3 - Immunosuppression (post transplant)
4 - Skin type (especially in lighter skinned patients)
5 - Lots of moles (especially atypical ones)
So primary prevention includes sun protection!
Risk factors:
1 - Genetics (ex: CDKN2A)
2 - UV exposure (for some populations)
3 - Immunosuppression (post transplant)
4 - Skin type (especially in lighter skinned patients)
5 - Lots of moles (especially atypical ones)
So primary prevention includes sun protection!
8/
Melanomas tend to arise de novo. 2/3 of melanomas come from normal skin. 1/3 from existing nevi.
Pet peeve of mine: A biopsied mole with "atypical cells" is NOT pre-melanoma. It's a marker that you might be higher risk, but not that it would've become melanoma!
Melanomas tend to arise de novo. 2/3 of melanomas come from normal skin. 1/3 from existing nevi.
Pet peeve of mine: A biopsied mole with "atypical cells" is NOT pre-melanoma. It's a marker that you might be higher risk, but not that it would've become melanoma!
9/
So why do we excise atypical nevi?
We're not necessarily worried it's going to become melanoma. The pathologic dx can be difficult & the severely atypical➡️melanoma spectrum is a gray area.
We're actually starting to excise fewer atypical nevi now!
jamanetwork.com/journals/jamad…
So why do we excise atypical nevi?
We're not necessarily worried it's going to become melanoma. The pathologic dx can be difficult & the severely atypical➡️melanoma spectrum is a gray area.
We're actually starting to excise fewer atypical nevi now!
jamanetwork.com/journals/jamad…
10/
OK, so what happens if you get a melanoma #dermpath report? It can be overwhelming! You might see this:
Diagnosis: Melanoma (see note).
Note:
Type: superficial spreading
Breslow depth: 1.2 mm
Clark level: IV
Ulceration: -
Mitoses: 1/hpf
Q: What matters most for prognosis?
OK, so what happens if you get a melanoma #dermpath report? It can be overwhelming! You might see this:
Diagnosis: Melanoma (see note).
Note:
Type: superficial spreading
Breslow depth: 1.2 mm
Clark level: IV
Ulceration: -
Mitoses: 1/hpf
Q: What matters most for prognosis?
11/
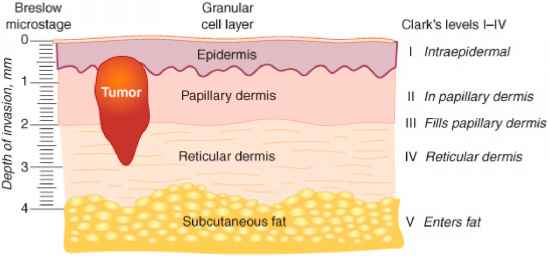
BRESLOW DEPTH holds the most prognostic information.
It doesn't matter what level of skin you've invaded (right side of pic 1), the physical depth (left side of pic 1) to the deepest melanoma cell is most important.
The #dermpath photo is to show you how HARD this is!

BRESLOW DEPTH holds the most prognostic information.
It doesn't matter what level of skin you've invaded (right side of pic 1), the physical depth (left side of pic 1) to the deepest melanoma cell is most important.
The #dermpath photo is to show you how HARD this is!

12/
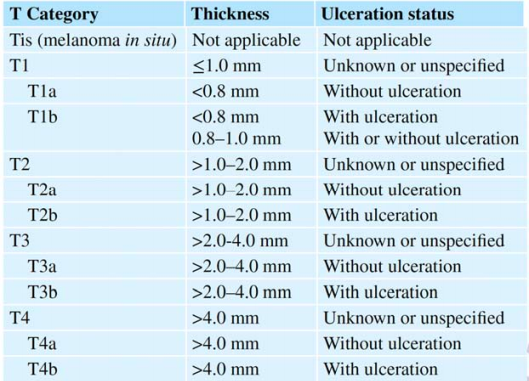
If you look at the KM curve based on breslow, you can see why we care so much about it!
The next pic is how we start the TNM staging with the primary tumor, mainly by breslow and +/- ulceration.
If you want to see how we stage overall, check out: cancerstaging.org/references-too…

If you look at the KM curve based on breslow, you can see why we care so much about it!
The next pic is how we start the TNM staging with the primary tumor, mainly by breslow and +/- ulceration.
If you want to see how we stage overall, check out: cancerstaging.org/references-too…

13/
But realistically, what do we do when we get a melanoma report?
If the patient has a melanoma that is stage T1a or less (< 0.75 mm, without ulceration), we may do a wide local excision ourselves. Once we are T1b or higher, we refer to surg/med onc!
But realistically, what do we do when we get a melanoma report?
If the patient has a melanoma that is stage T1a or less (< 0.75 mm, without ulceration), we may do a wide local excision ourselves. Once we are T1b or higher, we refer to surg/med onc!
14/
But if sentinal node biopsies don't change prognosis, why do we refer?
1 - If we do the WLE and the patient wants a SLNBx later, we don't want to have disrupted the lymphatics.
2 - SLNBx might not change prognosis, but + nodes might open new treatment options for the pt.
But if sentinal node biopsies don't change prognosis, why do we refer?
1 - If we do the WLE and the patient wants a SLNBx later, we don't want to have disrupted the lymphatics.
2 - SLNBx might not change prognosis, but + nodes might open new treatment options for the pt.
15/
What do we do for our melanoma pts after dx? If it's local disease and they've had WLE, we start more frequent skin checks for the first 5 years (and become bffs given the frequent visits).
Let's not forget about the psychological toll having a diagnosis of melanoma has too!
What do we do for our melanoma pts after dx? If it's local disease and they've had WLE, we start more frequent skin checks for the first 5 years (and become bffs given the frequent visits).
Let's not forget about the psychological toll having a diagnosis of melanoma has too!
16/
A note to say: when I started residency in 2010, metastatic melanoma was a TERRIBLE diagnosis. 5 year survival was <5%.
But the field has changed immensely, first with BRAF then MEK inhibitors, & now checkpoint inhibitors. Survival for metastatic melanoma has skyrocketed!
A note to say: when I started residency in 2010, metastatic melanoma was a TERRIBLE diagnosis. 5 year survival was <5%.
But the field has changed immensely, first with BRAF then MEK inhibitors, & now checkpoint inhibitors. Survival for metastatic melanoma has skyrocketed!
17/
RECAP
✅ Melanoma is common, and can be fatal, especially in young women.
✅ ABCDE(F)s are critical for diagnosis
✅ Sunprotection is important for some
✅ Breslow depth matters most
✅ Treatments for metastatic melanoma are much better now than just 10 years ago!
RECAP
✅ Melanoma is common, and can be fatal, especially in young women.
✅ ABCDE(F)s are critical for diagnosis
✅ Sunprotection is important for some
✅ Breslow depth matters most
✅ Treatments for metastatic melanoma are much better now than just 10 years ago!
18/
Obviously, the entire field of melanoma is way too big to be covered comprehensively in a #tweetorial, but I hope this helps cover some basics for you!
Please feel free to drop a comment with your pearls/additions below!
Until next time!
Obviously, the entire field of melanoma is way too big to be covered comprehensively in a #tweetorial, but I hope this helps cover some basics for you!
Please feel free to drop a comment with your pearls/additions below!
Until next time!
• • •
Missing some Tweet in this thread? You can try to
force a refresh