Tweeting the WHO's conference on #LongCOVID (called "Post COVID-19 Condition" here) as possible.
It starts off with the amazing @LongCovidSOS video from earlier this year: 1/
It starts off with the amazing @LongCovidSOS video from earlier this year: 1/
Dr. Pardo-Villamizar giving us a history of the (mostly neurological) symptoms from pandemics in the past. 2/
Dr. Dale Needham on post-ICU syndrome. Symptoms are similar to non-hospitalized #LongCOVID. Mentions the 6 minute walk test - would be helpful to do on non-hospitalized patients too.
Cognitive test scores look like TBIs or mild alzheimer's, no difference in severity. 3/
Cognitive test scores look like TBIs or mild alzheimer's, no difference in severity. 3/
Familiar face Andrea Lerner recaps the NIH workshop:
107 million cases. Even if a small % of cases have prolonged recovered (estimates range from 10-21%), that is an enormous public health issue.
"What we learn from this can be applied to other post-viral conditions."
4/
107 million cases. Even if a small % of cases have prolonged recovered (estimates range from 10-21%), that is an enormous public health issue.
"What we learn from this can be applied to other post-viral conditions."
4/
Common issues:
-cognitive impairment
-inequities around race
-lack of healthcare coverage (US)
Post-ICU is one phenotype, but #LongCOVID manifests after both severe and not-severe illness 5/
-cognitive impairment
-inequities around race
-lack of healthcare coverage (US)
Post-ICU is one phenotype, but #LongCOVID manifests after both severe and not-severe illness 5/
Dr. Gail Carson summarizes the ISRARIC #LongCOVID conference from December.
Important: "Nothing about us without us", meaning patient involvement is crucial.
#LongCOVID lacked recognition for months 6/
Important: "Nothing about us without us", meaning patient involvement is crucial.
#LongCOVID lacked recognition for months 6/
#LongCOVID in children is less well recognized.
Mental health impact is possibly the direct impact of the virus (completely agree with this!! check out Jarred Younger's research here) 7/
Mental health impact is possibly the direct impact of the virus (completely agree with this!! check out Jarred Younger's research here) 7/
Next up @Daltmann10!
Talking about #LongCOVID clinics: these need to include neurological, cardiovascular, respiratory, endocrinological care - no shuffling from doctor to doctor.
How can we refer patients when most around the world don't have a PCR or antibody test? 8/
Talking about #LongCOVID clinics: these need to include neurological, cardiovascular, respiratory, endocrinological care - no shuffling from doctor to doctor.
How can we refer patients when most around the world don't have a PCR or antibody test? 8/
We need immunity data! Is this an over or under reaction to the virus?
We are facing 10-20 *million* #LongCOVID cases around the world to manage! This has massive ramifications!
We need to move from the observational to the interventional! 9/
We are facing 10-20 *million* #LongCOVID cases around the world to manage! This has massive ramifications!
We need to move from the observational to the interventional! 9/
Post-Ebola and persistent mono infections have similar long-term symptoms
Patient groups are highly motivated, active, and ready to team up with researchers :)
10/
Patient groups are highly motivated, active, and ready to team up with researchers :)
10/
@DrTedros is up:
This has to be people-centered....we *have* to be listening.
We need recognition, research, & rehabiliitation (a reference to @LongCOVIDSOS's campaign).
#LongCOVID has economic & societal impacts as well! Need research here. 11/
This has to be people-centered....we *have* to be listening.
We need recognition, research, & rehabiliitation (a reference to @LongCOVIDSOS's campaign).
#LongCOVID has economic & societal impacts as well! Need research here. 11/
The 110 million cases is underreported. Morbidity is high.
We still don't have enough research.
We need rehabilitation & we need countries to prioritize this.
We understand that we're just starting. #LongCOVID is at its early stage. Sustaining the fight will be key. 12/
We still don't have enough research.
We need rehabilitation & we need countries to prioritize this.
We understand that we're just starting. #LongCOVID is at its early stage. Sustaining the fight will be key. 12/
Dr. Janet Diaz is up, talking about recommendations, standardizing data. (More info here but missed a bit of it)
Recommends the WHO Global Forum on Neurology and COVID-19. 13/
Recommends the WHO Global Forum on Neurology and COVID-19. 13/
5 minute break then I'm up 😬 14/
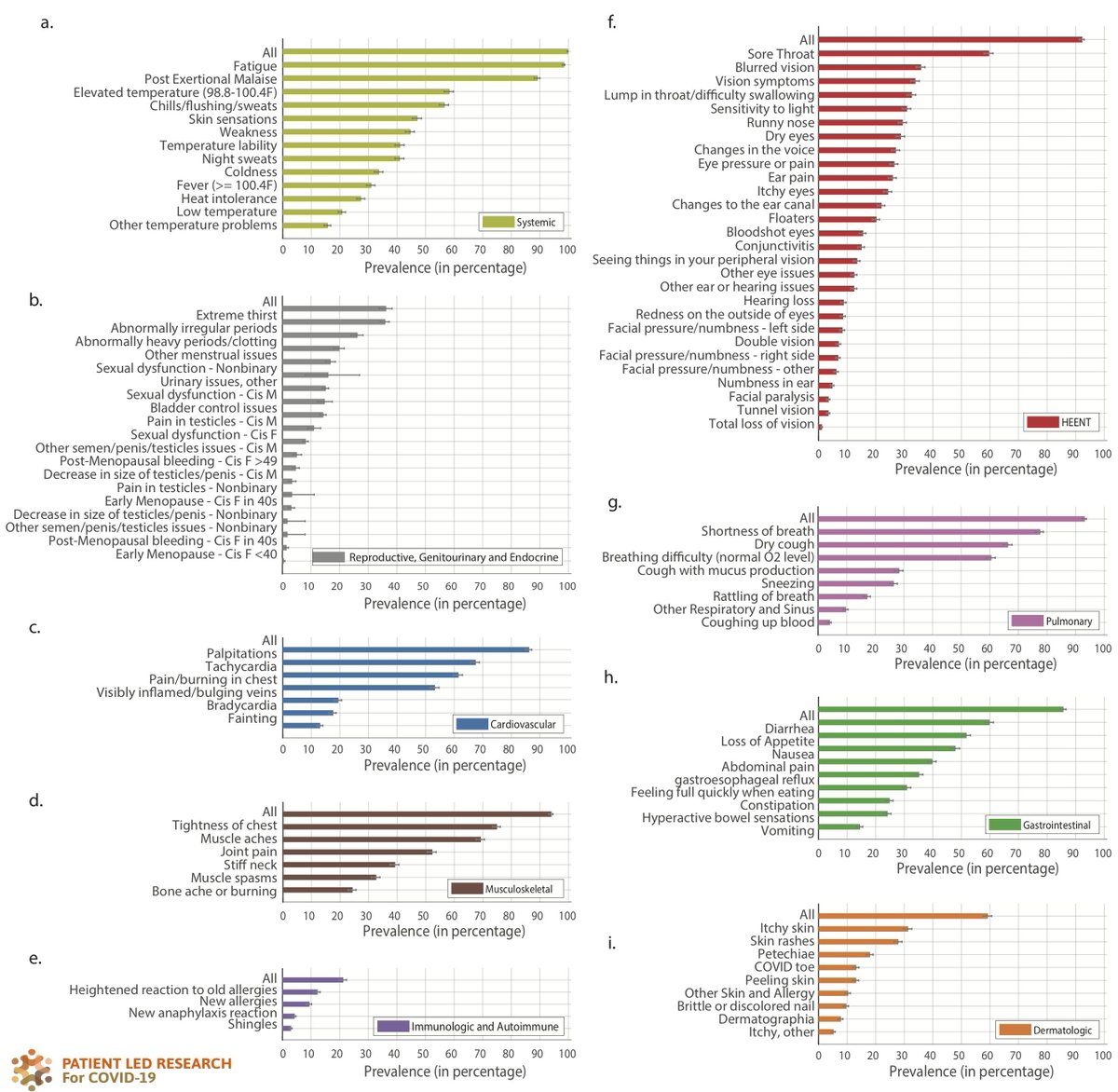
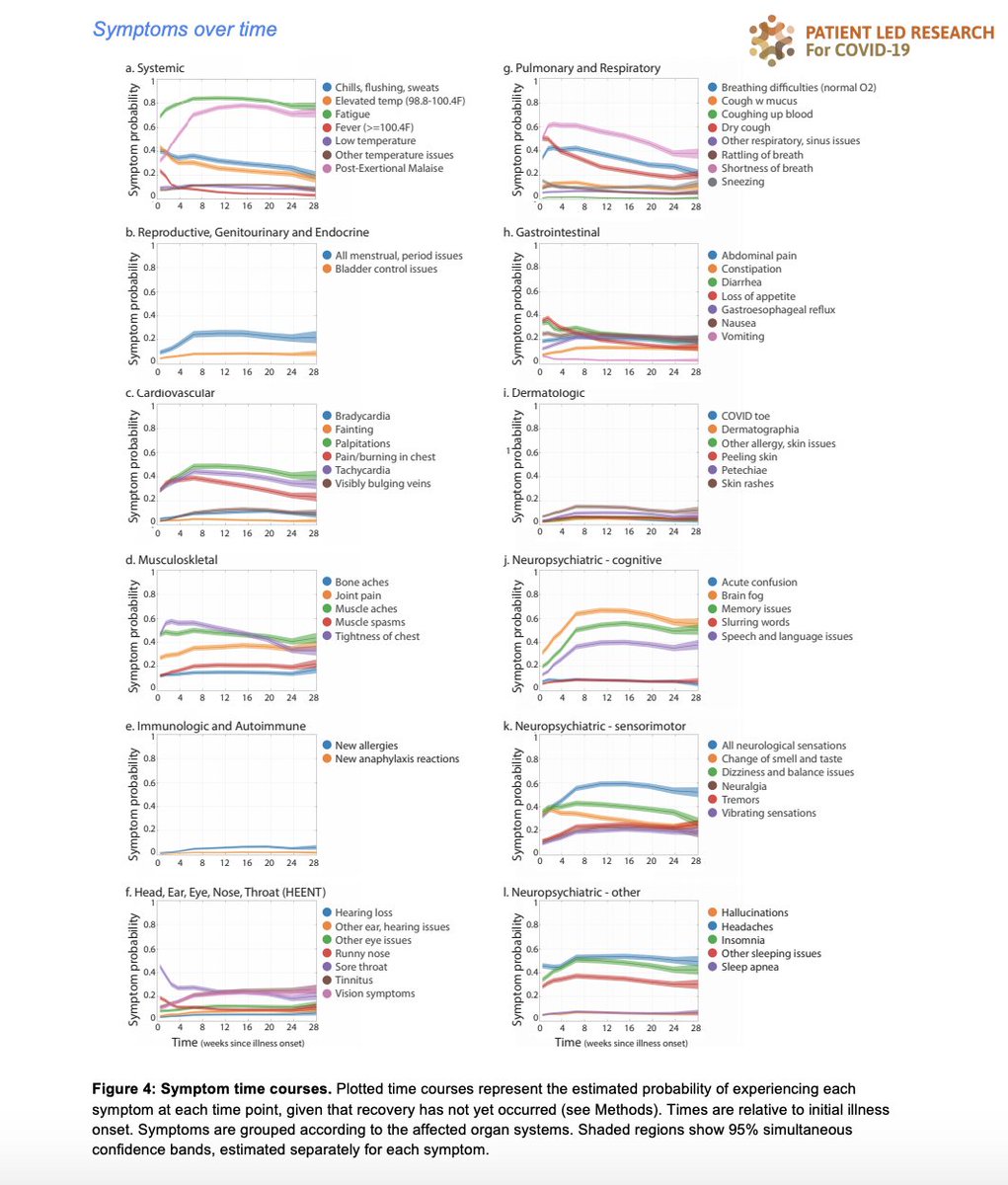
Phew. My slides are here, I'll add speaker notes at some point! Please see more at @patientled!
docs.google.com/presentation/d… 15/
docs.google.com/presentation/d… 15/
Dr. Bin Cao up with experiences from China, mostly hospitalized patients.
There is a decline in antibodies, particularly neutralizing antibodies.
58 patients diagnosed with diabetes at followup.
At 6 months, most patients had 1+ symptom. Fatigue, muscle weakness common 16/
There is a decline in antibodies, particularly neutralizing antibodies.
58 patients diagnosed with diabetes at followup.
At 6 months, most patients had 1+ symptom. Fatigue, muscle weakness common 16/
Dr. Marco Rizzi with experiences from Italy:
Fatigue, shortness of breath common.
Anosmia was more common in women (curious!) but only in a small (3-5%) of patients at followup. 17/
Fatigue, shortness of breath common.
Anosmia was more common in women (curious!) but only in a small (3-5%) of patients at followup. 17/
Dr. Simone Piva from Italy:
Cognitive dysfunction was in 20%
Anxiety and depression were generally normal.
Just 3% had PTSD.
Their ICU patients' data is different from what they're finding outside the ICU and in other ICU patients.
18/
Cognitive dysfunction was in 20%
Anxiety and depression were generally normal.
Just 3% had PTSD.
Their ICU patients' data is different from what they're finding outside the ICU and in other ICU patients.
18/
Lots of post-ICU people. Next up is Dr. Regis Rosa from Brazil on post-ICU outcomes:
61.3% were male, average age 52, all hospitalized, in hospital for an average of 9 days.
16% of patients who didn't need oxygen & 40% who did required rehospitalization before 6 months! 19/
61.3% were male, average age 52, all hospitalized, in hospital for an average of 9 days.
16% of patients who didn't need oxygen & 40% who did required rehospitalization before 6 months! 19/
Possibly worse physical functioning status for women in the ICU, both with and without oxygen, compared to men. Didn't mention if it was statistically significant 20/
We took a break to participate in working groups, there were 3:
1. Clinical case definition
2. Clinical case definition through the lens of diagnostics
3. Prevention, management, and treatment
21/
1. Clinical case definition
2. Clinical case definition through the lens of diagnostics
3. Prevention, management, and treatment
21/
Working Group 2 is presenting first (Dr. John Marshall):
-potentially 2-3 conditions going on:
1) very sick ICU patient, post-ICU syndrome, psychiatric & PTSD
2) patients with disproportionately mild disease but long term debilitating symptoms: fatigue, PEM, cog dysfunction
22/
-potentially 2-3 conditions going on:
1) very sick ICU patient, post-ICU syndrome, psychiatric & PTSD
2) patients with disproportionately mild disease but long term debilitating symptoms: fatigue, PEM, cog dysfunction
22/
Group #1 is almost the minority, implying #2 is a delayed immune response that may have prevented early immune response earlier on!
23/
23/
We need to know, is this:
1. Viral persistence (GI tract?)
2. Driven by host response? either chronic perturbation or activation of autoimmune response
3. Residual damage to ACE-2 pos tissue
These are not mutually exclusive!
24/
1. Viral persistence (GI tract?)
2. Driven by host response? either chronic perturbation or activation of autoimmune response
3. Residual damage to ACE-2 pos tissue
These are not mutually exclusive!
24/
Tests to look at host response:
Immunologic
Metabolic
Inflammation
Coagulation testing
Endocrine
25/
Immunologic
Metabolic
Inflammation
Coagulation testing
Endocrine
25/

The role of imaging: conventional imaging may not show even severe impacts 26/
Instead, should be using functional MRIs and others, brain MRI but also spine MRI (good job whoever suggested this!!)
27/
27/

Working group 3 is next (Prevention, Management, Research):
-recognition that too many studies are in hospitalized patients
-nonhospitalized have difficulty with testing
-outpatient services aren't aligned with the needs
-symptoms don't necessarily correlate with severity
28/
-recognition that too many studies are in hospitalized patients
-nonhospitalized have difficulty with testing
-outpatient services aren't aligned with the needs
-symptoms don't necessarily correlate with severity
28/
Pharmacological interventions and potential targets
Shout out to @sarahgeline request to include nonhospitalized patients in trials!
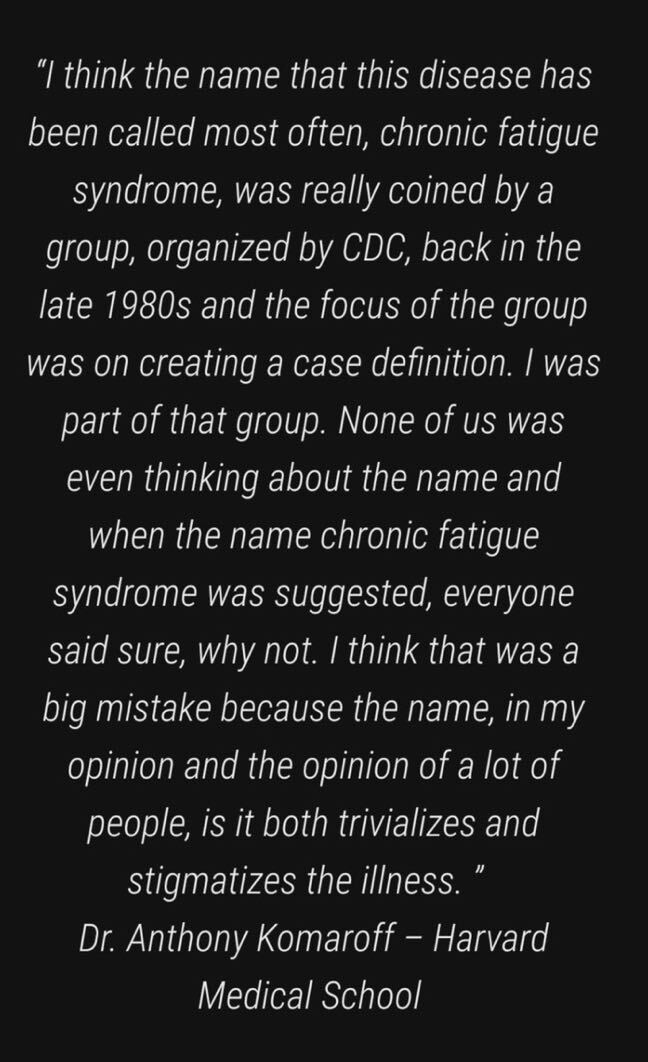
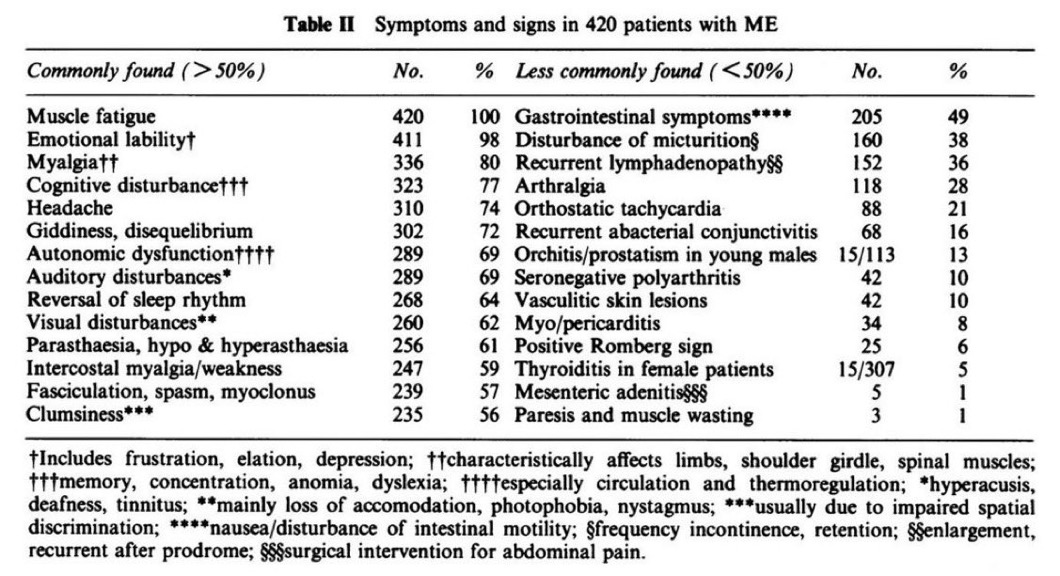
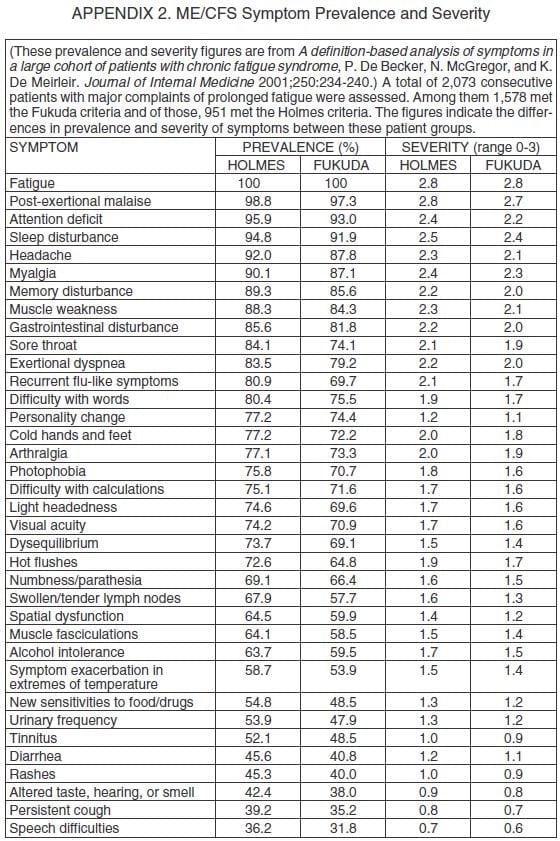
@PlzSolveCFS and @patientled request to learn from research being doing by those working in the ME biomedical field(s)
29/

Shout out to @sarahgeline request to include nonhospitalized patients in trials!
@PlzSolveCFS and @patientled request to learn from research being doing by those working in the ME biomedical field(s)
29/


Non-pharmacological needs:
-Hospital staff have PTSD and need psychological help
-cognitive assessments need to happen at initial phase
-education and information to the public are key!
-very strong emphasis on comprehensive and universal healthcare coverage
30/
-Hospital staff have PTSD and need psychological help
-cognitive assessments need to happen at initial phase
-education and information to the public are key!
-very strong emphasis on comprehensive and universal healthcare coverage
30/
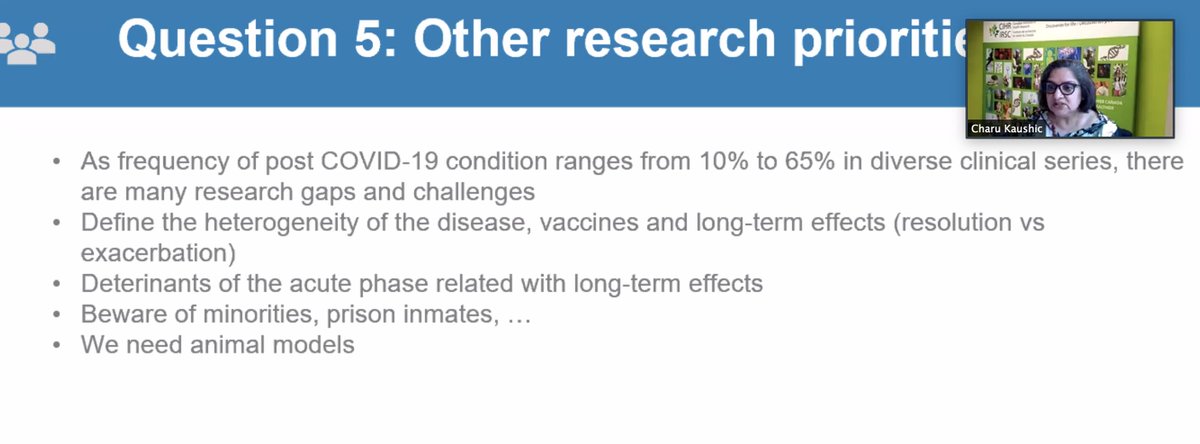
Other research priorities ("minorities and prison inmates" is poorly worded here but means they need priority!)
31/
31/
Working Group 1 (I was in this one):
-case definition is necessary not only for epidemiological research but for management/meeting patient needs
-heterogeneity across post COVID patients
-want to ground the discussion is recognition of patients
32/
-case definition is necessary not only for epidemiological research but for management/meeting patient needs
-heterogeneity across post COVID patients
-want to ground the discussion is recognition of patients
32/
-Need to move beyond case counting to characterization and then actionable items and management
-different symptom clusters, neurological, pulmonary, GI, endocrine
-but that many are not individual organs systems at all
but are systemic!!
33/
-different symptom clusters, neurological, pulmonary, GI, endocrine
-but that many are not individual organs systems at all
but are systemic!!
33/

A lot of the same theories as working group 1:
-inflammation
-immune dysregulation
-viral persistance (GI tract)
-coagulation/vascular issues
-endocrine & metabolic derangements
34/
-inflammation
-immune dysregulation
-viral persistance (GI tract)
-coagulation/vascular issues
-endocrine & metabolic derangements
34/
These are good pathways of investigation (though obviously would add brain inflammation to this, especially based on the brainstem hypometabolism in #LongCOVID paper that came out last month) 35/ 

Research gaps:
-important to have inclusivity across different patient populations
-BIPOC
-socially disadvantaged
-pediatrics
-pregnant/maternal
36/
-important to have inclusivity across different patient populations
-BIPOC
-socially disadvantaged
-pediatrics
-pregnant/maternal
36/
Dr. Diaz sums up:
1. No one can be left behind
2. Heterogeneity happening
3. Fatigue, PEM, & cognitive dysfunction common
4. System-based sequelae (neurological, mental health, respiratory, cardiac, renal)
A lot of needs: prevalence, animal studies, vaccine responses in LC
37/
1. No one can be left behind
2. Heterogeneity happening
3. Fatigue, PEM, & cognitive dysfunction common
4. System-based sequelae (neurological, mental health, respiratory, cardiac, renal)
A lot of needs: prevalence, animal studies, vaccine responses in LC
37/
Dr. Ryan: Sometimes the greatest fear is that people will be left behind, that society won't think this is real -we are potentially at risk of doing that unless we stand up now. They are all valid, and they are all real, the pathophysiology will be tough but we need to do it. 38/
Dr. Ryan's brother is a #LongCOVID patient 39/
• • •
Missing some Tweet in this thread? You can try to
force a refresh