Neuroanatomy TOTD #15🧵
The inner ear #tweetorial--it packs a large functional punch for its small size-strap in!
#meded #FOAMed #FOAMrad #medtwitter #medstudents #radiology #neurorad #HNrad #radres #neurology #ENT #temporalbone #neurosurgery #neuroanatomy #neuroanatomyTOTD
1/24
The inner ear #tweetorial--it packs a large functional punch for its small size-strap in!
#meded #FOAMed #FOAMrad #medtwitter #medstudents #radiology #neurorad #HNrad #radres #neurology #ENT #temporalbone #neurosurgery #neuroanatomy #neuroanatomyTOTD
1/24
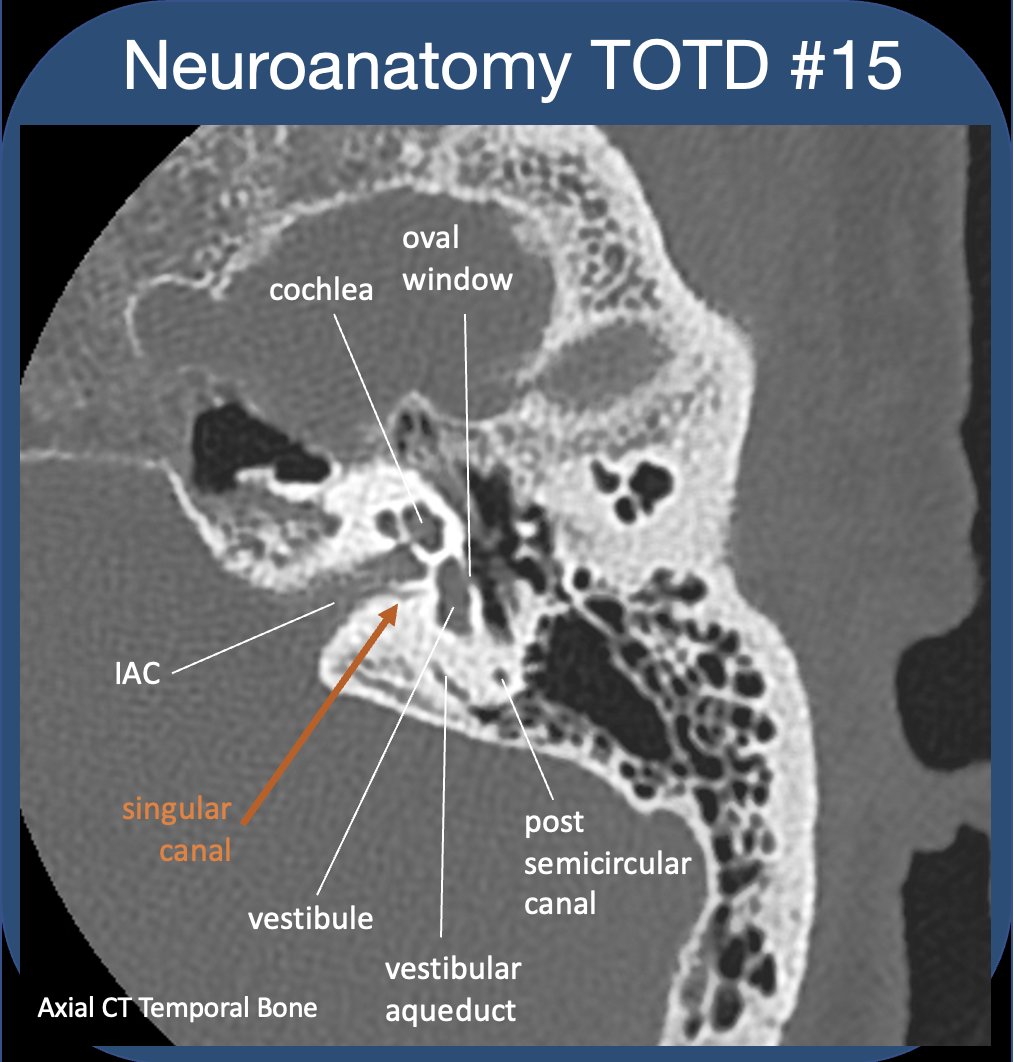
To evaluate the t-bone, best to compartmentalize--external/middle/inner ear (IE). See previous #tweetorial of the ME. The IE is difficult as most structures are obliquely oriented (at different obliquities!)-and can be hard to see on standard views. 2/24

https://twitter.com/aaronrutman/status/1348530356002045954

IE communicates with ME via oval&round windows (which allow for transmission&dissipation of sonic vibrations). IE houses sensory organs for hearing/balance/sensing motion. The cochlear&vestibular nerves (CNVIII) transmit signals to the brain via the int auditory canal (IAC). 3/24 

Let’s do some more compartmentalizing-divide the IE into MEMBRANOUS and OSSEOUS labyrinth, separated by a layer of perilymph shock absorption. What structures make up the different parts of the labyrinth, and what are the functions?
4/24
4/24

Consider how the labyrinth communicates with the ME (oval and round windows), as well as with the CSF space (vestibular and cochlear aqueducts), and how signals are sent back to the brain (CN VIII via IAC).
5/24

5/24


The MEMBRANOUS labyrinth (ML) contains endolymph & sensory epithelium. The BONY labyrinth (BL, or otic capsule) surrounds and houses the ML, separated by a layer of perilymph (which has no sensory epithelium, and mostly acts to absorb the energy of fluid motion).
6/24

6/24
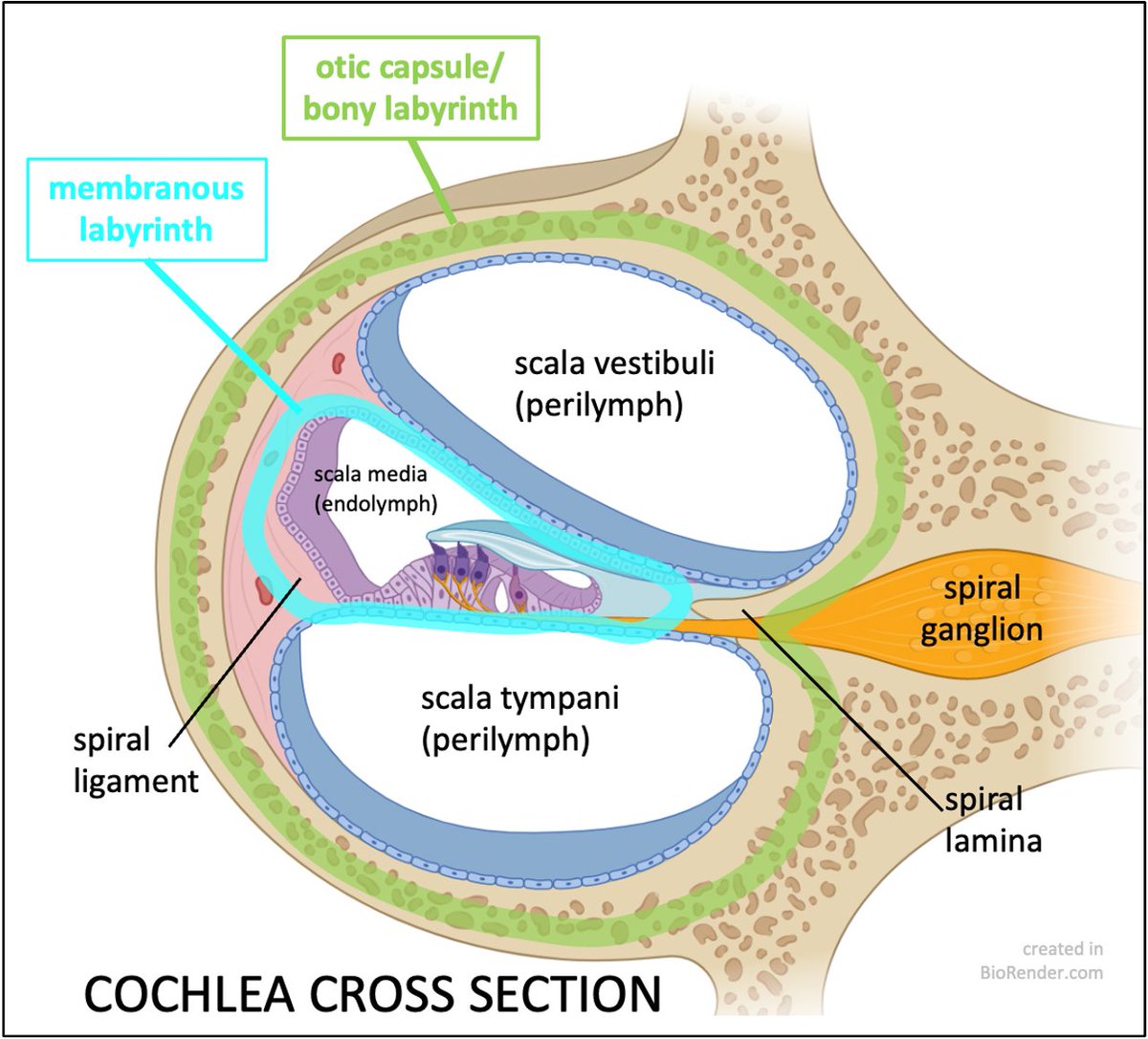

The ML consists of the endolymph-containing cochlear duct (scala media), utricle, saccule, semicircular ducts, and endolymphatic duct and sac. (Note endolymph K+>Na+; perilymph K+<Na+).
7/24
7/24

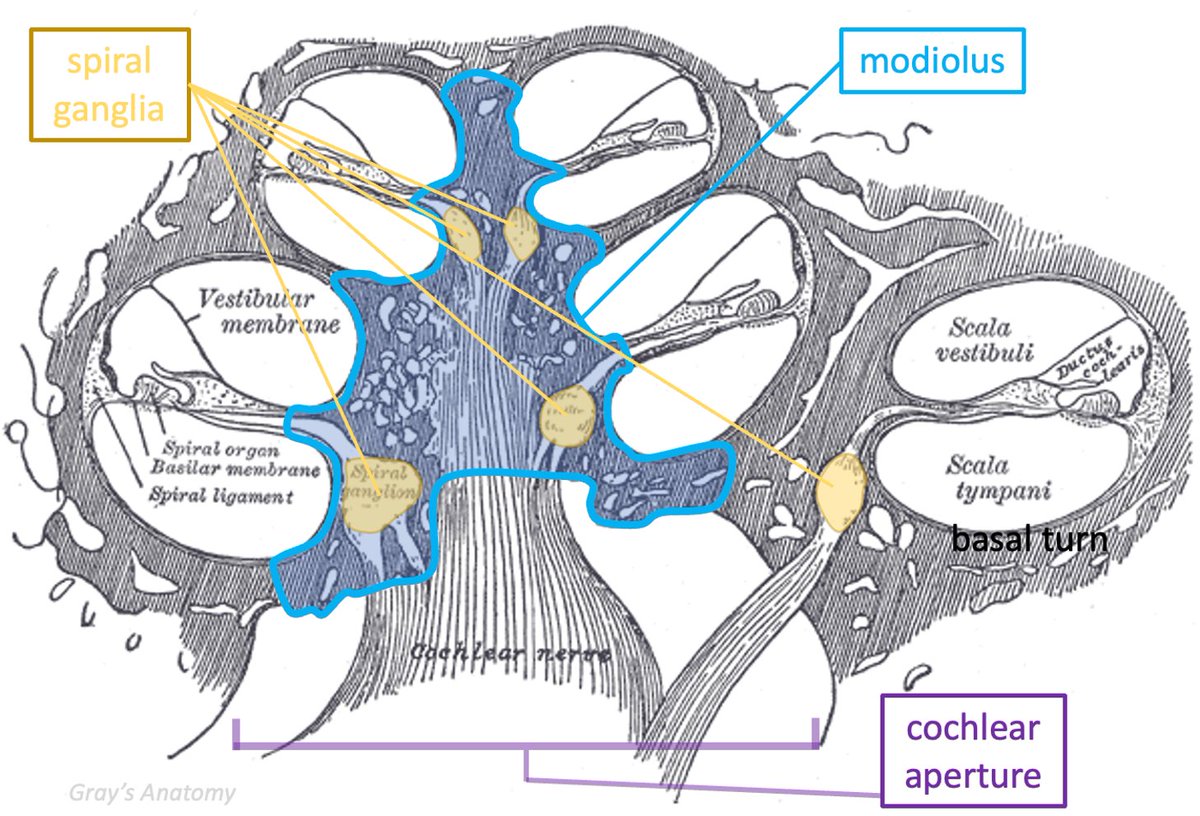
The ML and sensory organs within the ML are not well seen on imaging, but we know where they reside. For example, the membranous scala media (cochlea) is a/w the spiral lamina/ligament which projects from the cochlear modiolus and can be seen in the basal turn on imaging.
8/24

8/24


The COCHLEAR DUCT is synonymous w/ the scala media, separated from the perilymph of scala tympani by basilar membrane, and from scala vestibuli by Reissner’s membrane; hair cells of organ of Corti convert mechanical vibration into electrical potential; CNVIII➡️brainstem.
9/24
9/24
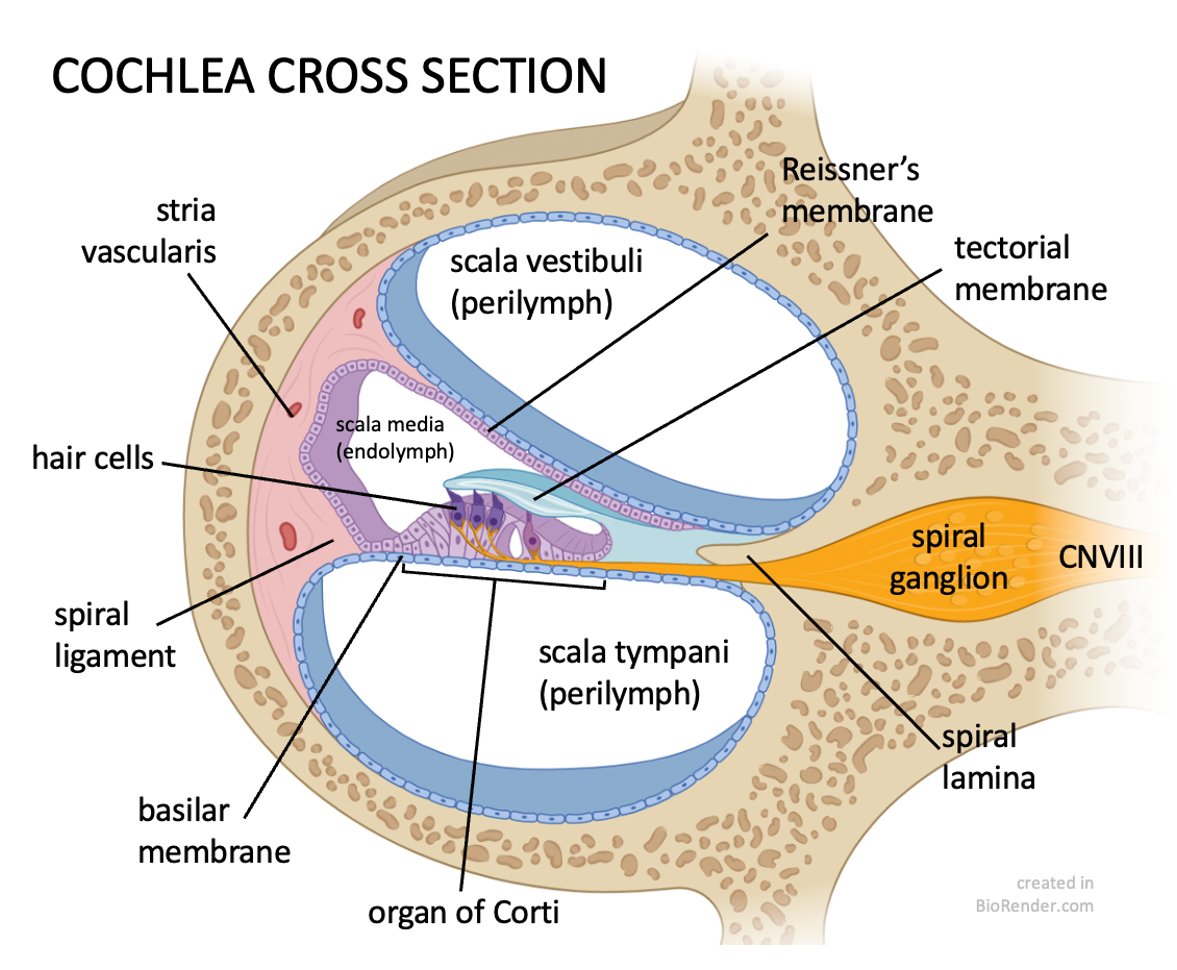
Note the bipolar cell bodies of the cochlear nerve are in the spiral ganglia, within the bony MODIOLUS, the osseous central axis around which the cochlea turns 2.5x. The modiolus is well seen on axial images.
10/24

10/24

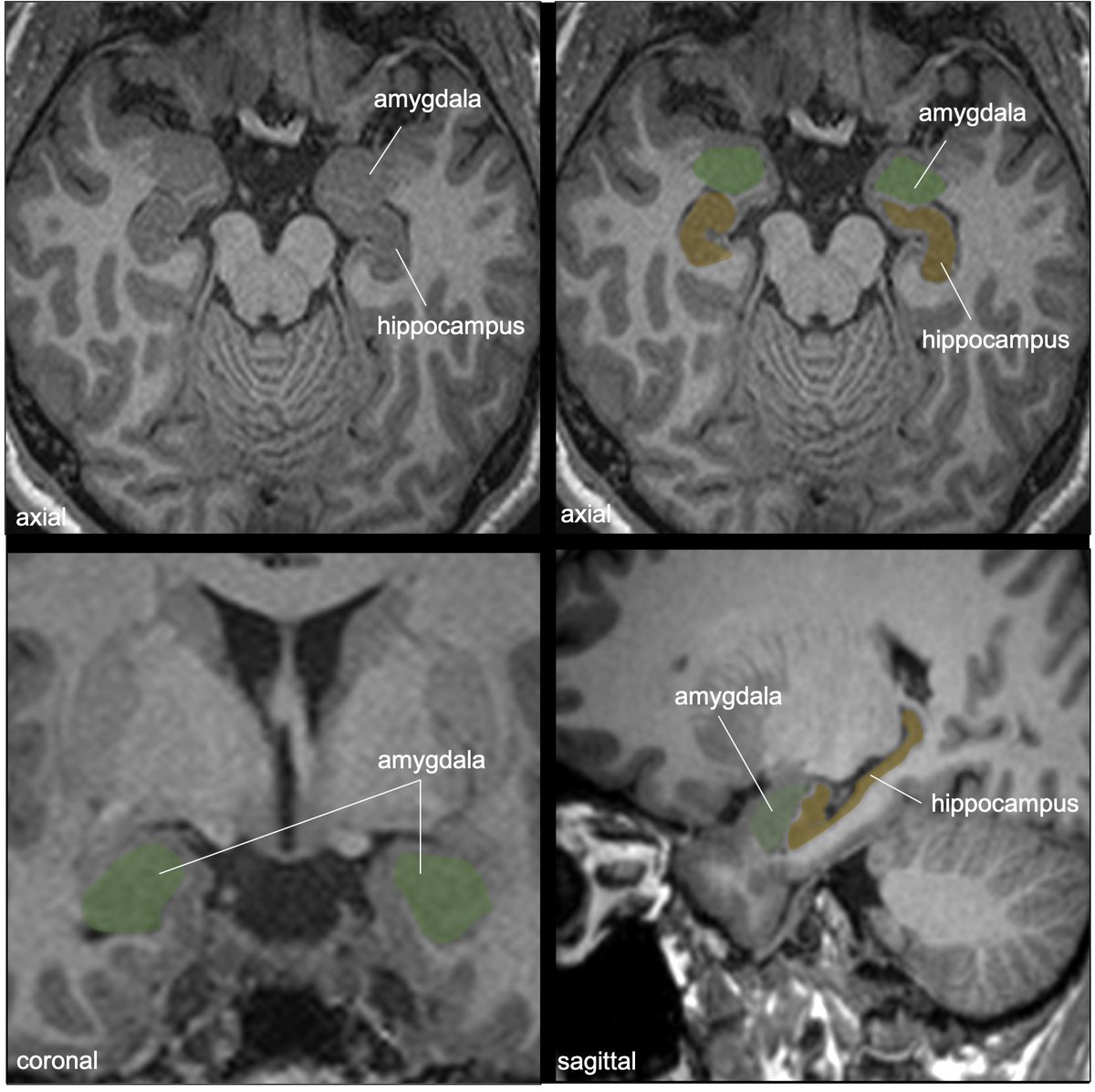
The VESTIBULE (of the BL) is continuous with the basal turn of the cochlea (well delineated on imaging). The vestibule houses the utricle & saccule of the membranous labyrinth (which are not seen on imaging).
11/24


11/24



The SACCULE/UTRICLE each have a MACULA which detect head position/linear acceleration (saccule-vertical; utricle-horizontal). Gravity on the otolithic membrane/otoliths promotes depolarization of the hair cells embedded in the gelatinous membrane.
12/24
12/24

The SEMICIRCULAR DUCTS (ML) are housed within the SEMICIRCULAR CANALS (BL). There are 3 – superior (SSC), lateral (LSC), & posterior (PSC). The limbs are continuous w/ the vestibule. Of note, a limb of the PSC & a limb of the SSC converge near the vestibule (common crus).
13/24
13/24

At the base if each duct➡️ampulla, in which there is a CRISTA AMPULLARES, which detects rotational acceleration (2/2 deflection of the gelatinous cupula by inertial flow of endolymph during head motion. Each crista ampullares responds to a different rotational axis.
14/24
14/24

Nerves from utricle/SSC/LSC travel in the sup division of the vestibular nerve, while those from saccule and PSC in the inf division. Of note, the nerve fibers of the PSC ampulla travel independently as the singular nerve, through its own SINGULAR CANAL to meet the IAC.
15/24

15/24


The VESTIBULAR AQUEDUCT is a bony channel (housing the membranous endolymphatic duct). It courses posterolaterally from the vestibule to the post. petrous surface, widening as it approaches the external aperture. Can be difficult to follow on CT due to its oblique course.
16/24
16/24

The ENDOLYMPHATIC SAC is the terminal end of the duct, situated at the aperture along the petrous margin, covered by dura. It's not clearly distinguished but we know where it lives. It functions in resorption of endolymph and pressure equalization with the CSF.
17/24
17/24
The COCHLEAR AQUEDUCT does not house any of the ML; it contains perilymph and courses obliquely, parallel and inferior to the IAC from the basilar turn of cochlea to just above the jugular foramen.
18/24
18/24

It has a funnel shaped opening above the jugular foramen, contiguous with the subarachnoid space, and variable in size (0-11mm). Its lateral end in the otic capsule is usually not well seen as it narrows towards the cochlea basal turn/vestibule.
19/24
19/24

Intrinsic channels can mimic otic capsule fractures--Note the petromastoid (or subarcuate) canal (which contains the subarcuate artery&vein), joins the mastoid antrum to the posterior fossa, threading the needle through under the arch of the sup semicircular canal.
20/24
20/24

Understanding normal IE #anatomy is critical for the #pedineurorad to understand complex congenital malformations that occur with abnormal IE development. Classic Mondini malformation p/w SNHL: only 1.5 turns in sac-like cochlea, enlarged vestibule/vestibular aqueduct/ELS.
21/24
21/24

Another classic IE dx-otosclerosis/otospongiosis: a leading cause of deafness in adults (osteodystrophy of the otic capsule). Case demonstrates typical lucency of the BL about the cochlea and oval window (retrofenestral otospongiosis). Stapedectomy/stapes prosthesis is tx.
22/24
22/24

Inner Ear!
...23/24
...23/24
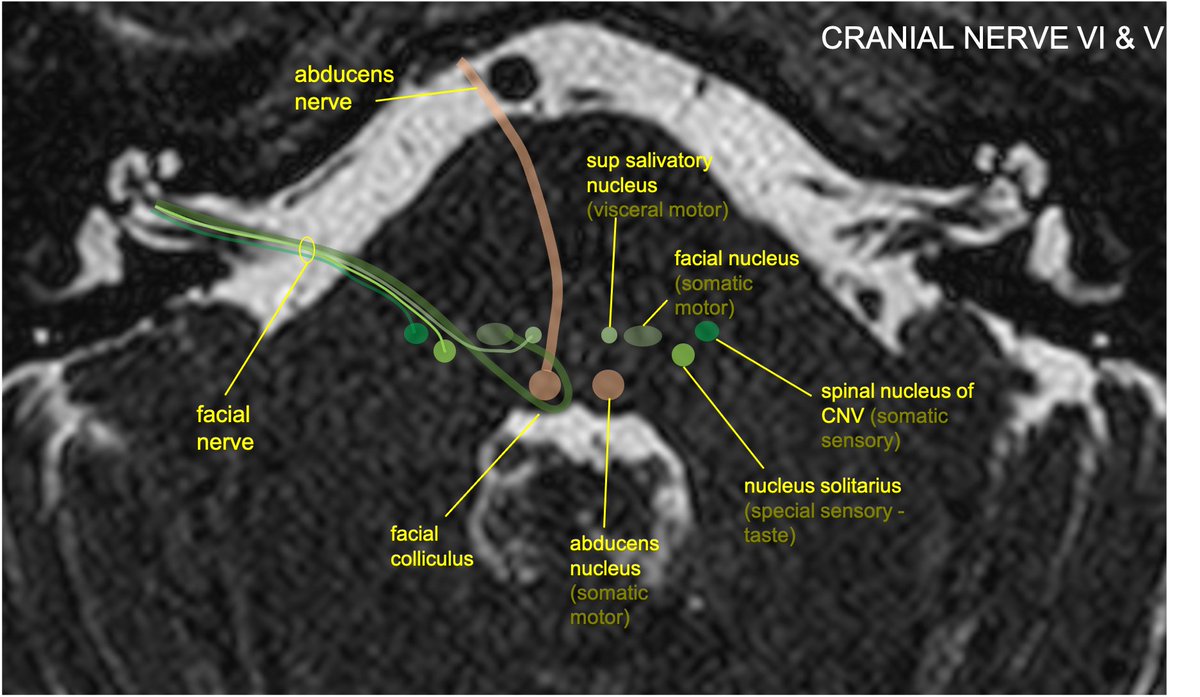
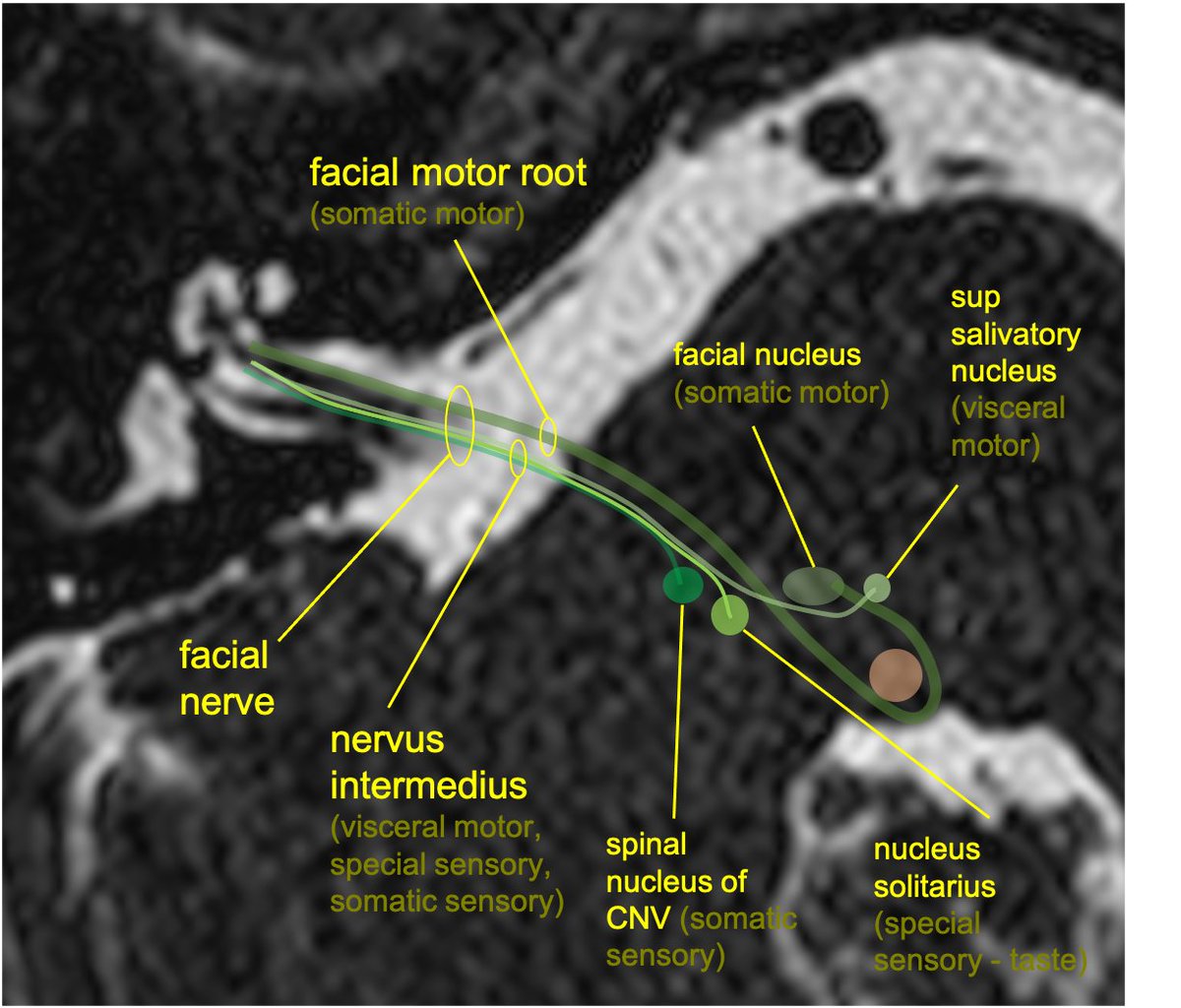
IAC nerves!
...24/24 (the end)
...24/24 (the end)
• • •
Missing some Tweet in this thread? You can try to
force a refresh