A #tweetorial on non-variceal upper gastrointestinal bleeding #NVUGIB
And an overview of why we do what we do
To warm up, which of the following is the most common cause of NVUGIB?
#gitwitter #livertwitter #medtwitter #MedEd
1/
And an overview of why we do what we do
To warm up, which of the following is the most common cause of NVUGIB?
#gitwitter #livertwitter #medtwitter #MedEd
1/
2/
PUD it is...
Btw wt do we mean by "upper"?
This is defined as a bleeding source proximal to the Ligament of Treitz, also known as the suspensory muscle of duodenum, the landmark that separates the duodenum & jejunum
PUD it is...
Btw wt do we mean by "upper"?
This is defined as a bleeding source proximal to the Ligament of Treitz, also known as the suspensory muscle of duodenum, the landmark that separates the duodenum & jejunum

3/
Back to PUD, there are actually many well established causes and some associated factors related to its development, the most important being:
💊 Drugs - NSAIDs/aspirin, direct chemical/erosive agents etc
🦠 Bugs - H. pylori
♋ Thugs (if I may) - Neoplasm
Back to PUD, there are actually many well established causes and some associated factors related to its development, the most important being:
💊 Drugs - NSAIDs/aspirin, direct chemical/erosive agents etc
🦠 Bugs - H. pylori
♋ Thugs (if I may) - Neoplasm

4/
So what does a patient with UGIB present with?
Listed are some of the commonest presenting symptoms and signs
☕ Isolated coffee ground vomiting is seldom due to UGIB... It could anything... Be wary of IO, sepsis, inferior MIs etc
⚠️ Syncope could be very serious bleeding
So what does a patient with UGIB present with?
Listed are some of the commonest presenting symptoms and signs
☕ Isolated coffee ground vomiting is seldom due to UGIB... It could anything... Be wary of IO, sepsis, inferior MIs etc
⚠️ Syncope could be very serious bleeding

5/
Syncope or fainting, is such a bad presenting symptom it's included in one of the risk stratification scores known as the Glasgow-Blatchford score (GBS)
Scoring 0⃣ means a low risk of complications and these patients may not need to be admitted
thelancet.com/article/S0140-…
Syncope or fainting, is such a bad presenting symptom it's included in one of the risk stratification scores known as the Glasgow-Blatchford score (GBS)
Scoring 0⃣ means a low risk of complications and these patients may not need to be admitted
thelancet.com/article/S0140-…

6/
A thorough history taking and physical examination is essential:
🧠 mental status
🚫 acute abdomen (ie shouldn't scope and need imaging/surgeon input)
💊 antiplatelets, anticoagulant use
A thorough history taking and physical examination is essential:
🧠 mental status
🚫 acute abdomen (ie shouldn't scope and need imaging/surgeon input)
💊 antiplatelets, anticoagulant use
7/
Many things to do before putting a scope in!
⚠️🔤 of resuscitation! Very important
+
DAVID
Diet
Activities
Vitals
Investigations
Drugs: ✅ stuff we give; ❌ stuff we stop
Scoping/Surgery (last but not least!)
⛔ contraindicated in perforation, intestinal obstruction

Many things to do before putting a scope in!
⚠️🔤 of resuscitation! Very important
+
DAVID
Diet
Activities
Vitals
Investigations
Drugs: ✅ stuff we give; ❌ stuff we stop
Scoping/Surgery (last but not least!)
⛔ contraindicated in perforation, intestinal obstruction


8/
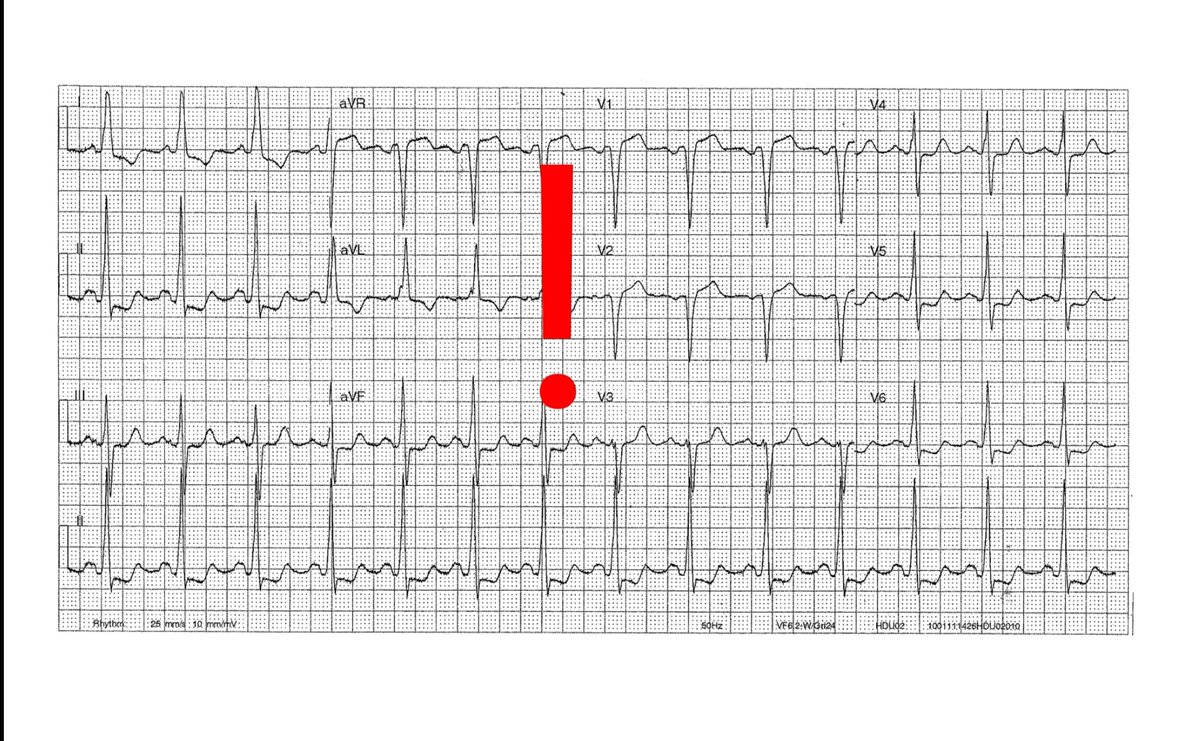
Besides blood taking, 🔬 Ix we routinely request include:
- erect CXR (any free gas, weird funny mediastinal gas)
- ECG (acute coronary syndrome)
&
- #covid19 in this day and age

Besides blood taking, 🔬 Ix we routinely request include:
- erect CXR (any free gas, weird funny mediastinal gas)
- ECG (acute coronary syndrome)
&
- #covid19 in this day and age

9/
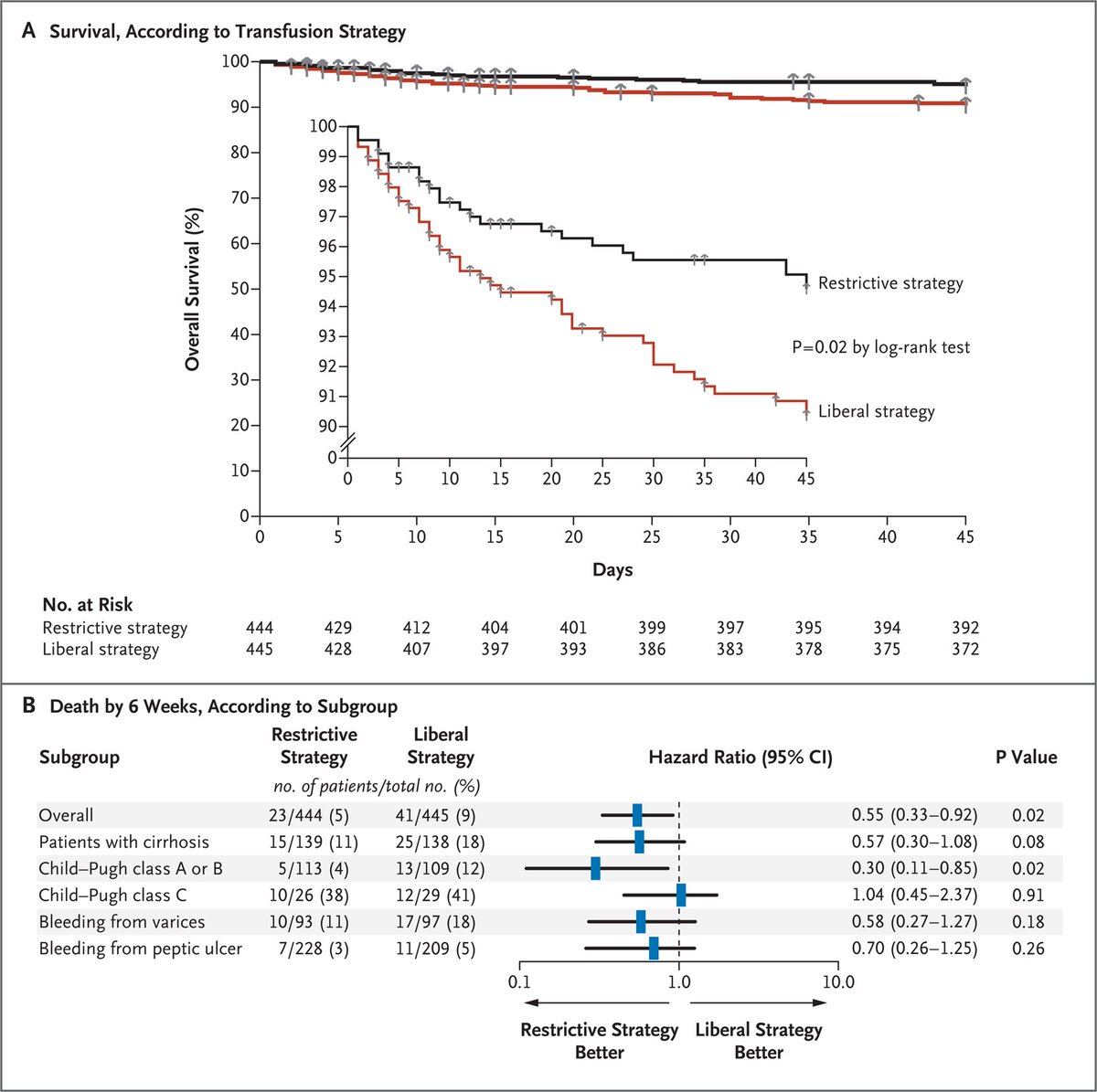
Restrictive transfusion with a Hb >= 7 g/dL is likely sufficient for most hemodynamically stable patients
Subgroup showed that this was better for Child's A/B (postulated that ⬆️splanchnic pressure ➡️ rebleeding, fluid overload, other transfusion Cx)
nejm.org/doi/full/10.10…

Restrictive transfusion with a Hb >= 7 g/dL is likely sufficient for most hemodynamically stable patients
Subgroup showed that this was better for Child's A/B (postulated that ⬆️splanchnic pressure ➡️ rebleeding, fluid overload, other transfusion Cx)
nejm.org/doi/full/10.10…

10/
A meta-analysis (MA) also favoured a restrictive transfusion strategy:
⬇️ Mortality & re-bleeding
↔️ No difference in ischemic events
✅ Transfuse to maintain circulation
❌ Aggressive over-transfusion

A meta-analysis (MA) also favoured a restrictive transfusion strategy:
⬇️ Mortality & re-bleeding
↔️ No difference in ischemic events
✅ Transfuse to maintain circulation
❌ Aggressive over-transfusion


11/
In REALITY, more evidence is emerging that a restrictive strategy may also be non-inferior for pts at risk for ischemic events, in this case acute myocardial infarction + anemia and 30 day MACE (though the CIs may have included what may be a clinically important harm)
In REALITY, more evidence is emerging that a restrictive strategy may also be non-inferior for pts at risk for ischemic events, in this case acute myocardial infarction + anemia and 30 day MACE (though the CIs may have included what may be a clinically important harm)

12/
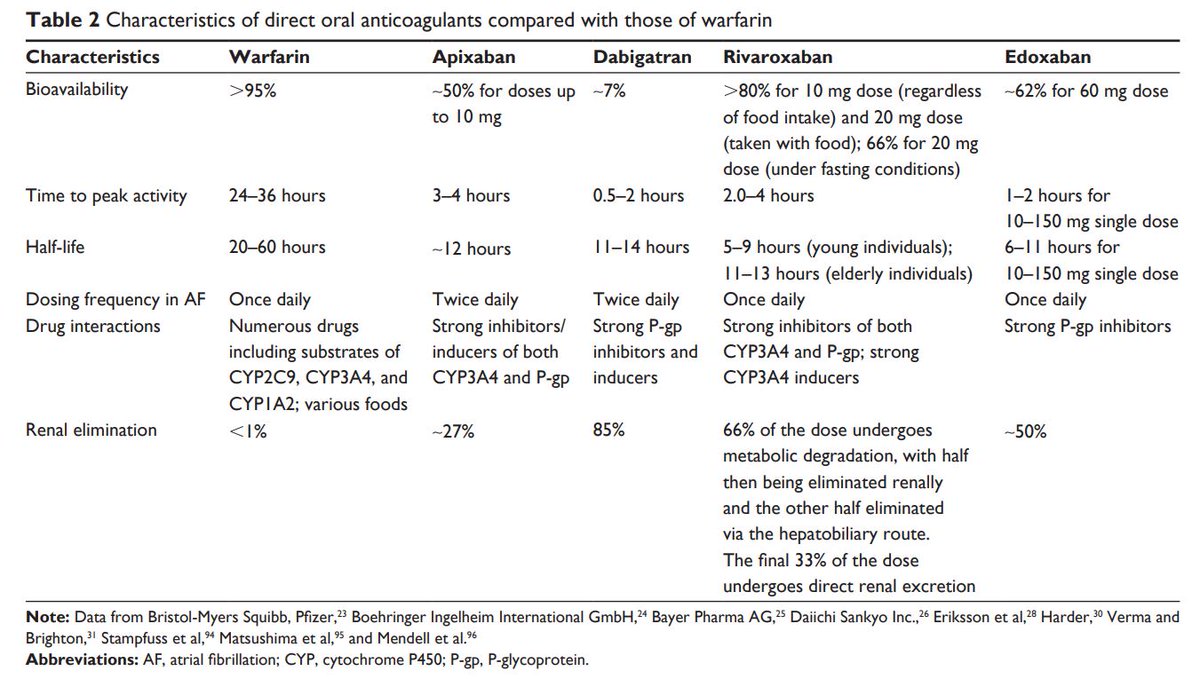
❌ Drugs to stop i.e. DAPTs, anticoagulants
Always ⚖️ risks (of thromboembolism) and benefits (easier hemostasis)
Risks of PUD re-bleeding ⬆️ in first 3⃣ days
The 2021 @ESGE_news guidelines in @endoscopyjrnl shared by @drkeithsiau are great!
❌ Drugs to stop i.e. DAPTs, anticoagulants
Always ⚖️ risks (of thromboembolism) and benefits (easier hemostasis)
Risks of PUD re-bleeding ⬆️ in first 3⃣ days
The 2021 @ESGE_news guidelines in @endoscopyjrnl shared by @drkeithsiau are great!
https://twitter.com/drkeithsiau/status/1382728838866743296?s=19
13/
⏳
Time is therapeutic!
In hemodynamically stable patients, withholding DOACs for a suitable duration according to the renal function can definitely help
⏳
Time is therapeutic!
In hemodynamically stable patients, withholding DOACs for a suitable duration according to the renal function can definitely help

14/
And for a thread discussing the GI safety and efficacy of #DOACs here's the link 👇
In summary: seems that apixaban has a more favourable GI safety profile (no COI)
And for a thread discussing the GI safety and efficacy of #DOACs here's the link 👇
In summary: seems that apixaban has a more favourable GI safety profile (no COI)
https://twitter.com/RashidLui/status/1376936027894337538?s=19
15/
In hemodynamically unstable cases or uncontrolled bleeding reversal agents may also need to be considered
In hemodynamically unstable cases or uncontrolled bleeding reversal agents may also need to be considered
https://twitter.com/RashidLui/status/1376936051504111618?s=19
16/
Finally we arrive at peri-endoscopic mx!
Wt is the role of pre-endoscopy prokinetics?
- A MA in @GIE_Journal showed that erythromycin or metoclopromide given immediately before OGD/EGD ⬇️ the need for repeat endoscopy but not other parameters
ncbi.nlm.nih.gov/books/NBK79206/
Finally we arrive at peri-endoscopic mx!
Wt is the role of pre-endoscopy prokinetics?
- A MA in @GIE_Journal showed that erythromycin or metoclopromide given immediately before OGD/EGD ⬇️ the need for repeat endoscopy but not other parameters
ncbi.nlm.nih.gov/books/NBK79206/

17/
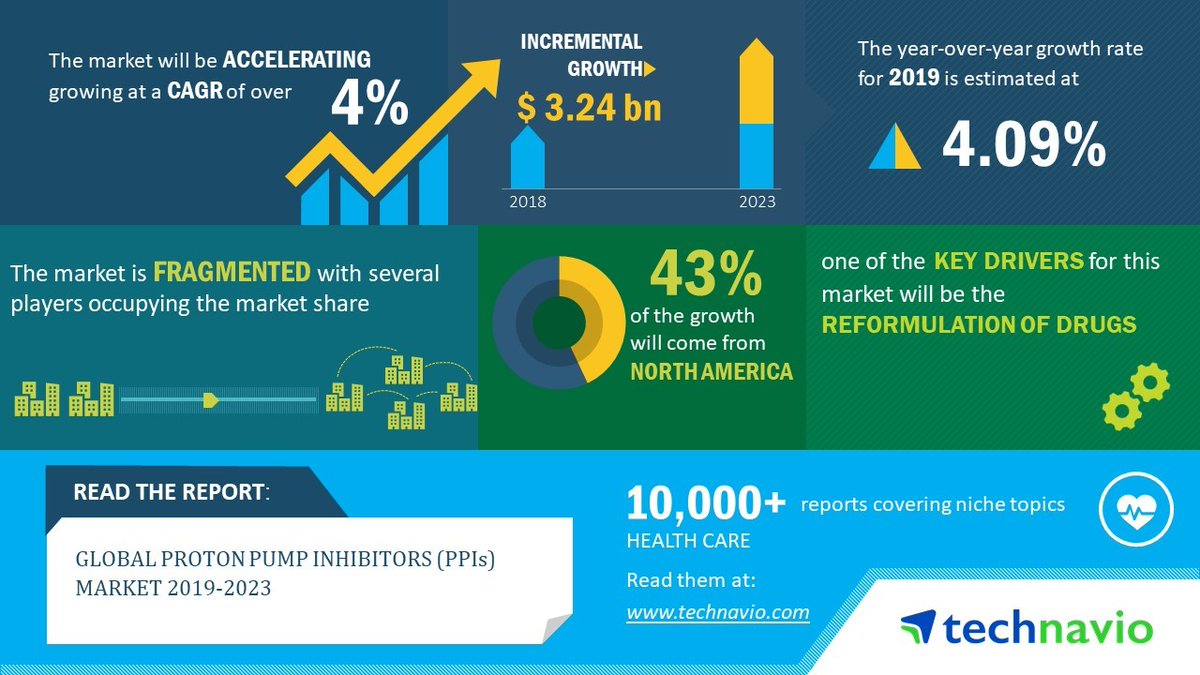
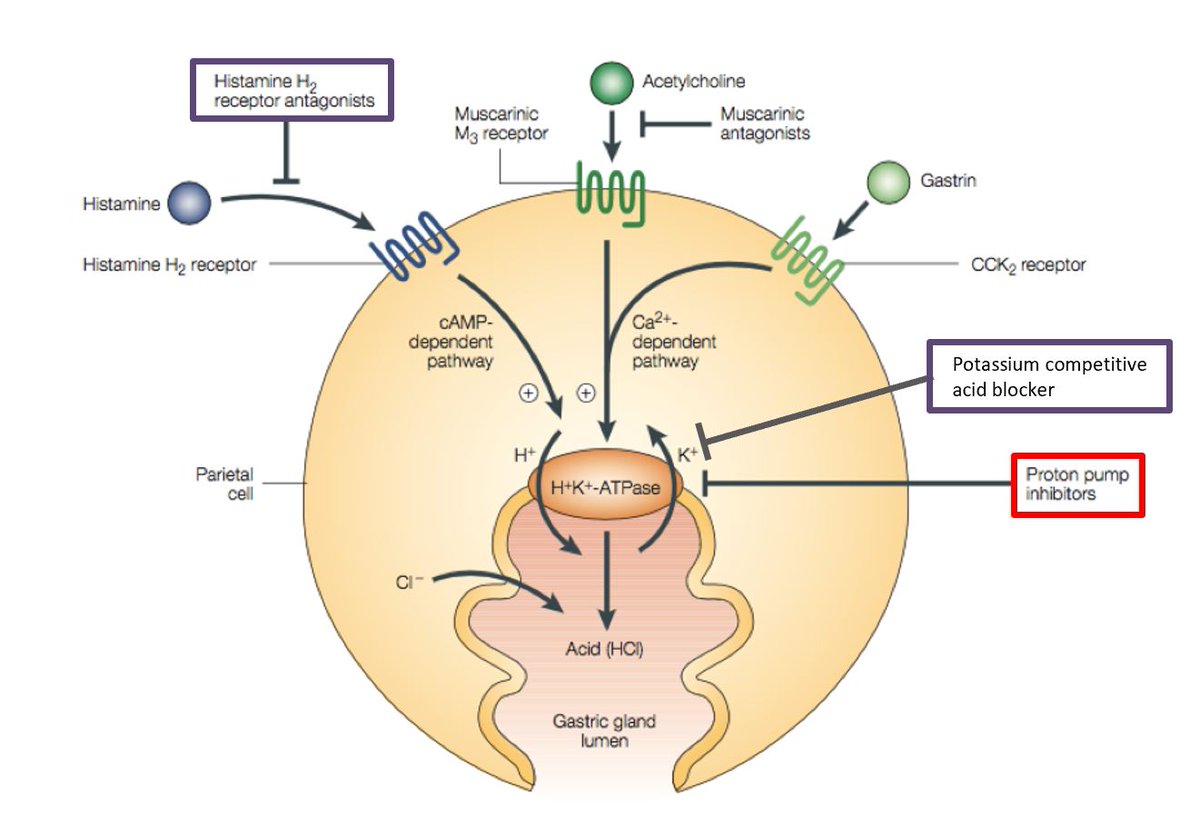
How about PPIs?
A landmark trial by Prof Lau @CUHKMedicine showed that pre-emptive PPI infusion:
⬇️ Endoscopic grade of lesions
⬇️ Need for endoscopic treatment
↔️ Similar rates of recurrent bleeding, surgery and 30-day ☠
nejm.org/doi/full/10.10…

How about PPIs?
A landmark trial by Prof Lau @CUHKMedicine showed that pre-emptive PPI infusion:
⬇️ Endoscopic grade of lesions
⬇️ Need for endoscopic treatment
↔️ Similar rates of recurrent bleeding, surgery and 30-day ☠
nejm.org/doi/full/10.10…


18/
Moving on to endoscopy, the timing of procedure has been debated for quite a while
A UK audit across 20 centres the median time to endoscopy was 21.2 h (IQR 12-35.7) with early endoscopy (<24 h achieved in ~60% of cases) but is pushing it earlier better?

Moving on to endoscopy, the timing of procedure has been debated for quite a while
A UK audit across 20 centres the median time to endoscopy was 21.2 h (IQR 12-35.7) with early endoscopy (<24 h achieved in ~60% of cases) but is pushing it earlier better?


19/
Another RCT by Prof Lau > 500 pts with overt UGIB and a GBS of >= 12 were randomised to urgent (<6h) or early (6-24h) showing that urgent scoping was not ass with ⬇️30day mortality
⚠️Excluded pts who did not stabilize with resuscitation, small no. of variceal bleeds

Another RCT by Prof Lau > 500 pts with overt UGIB and a GBS of >= 12 were randomised to urgent (<6h) or early (6-24h) showing that urgent scoping was not ass with ⬇️30day mortality
⚠️Excluded pts who did not stabilize with resuscitation, small no. of variceal bleeds


20/
So we finally arrive to the point where we put a scope in
We classify the endoscopic appearance of ulcers by the Forrest classification with great examples by @EndoscopyCampus endoscopy-campus.com/en/classificat…
The rebleeding rates (w/o therapy) are tabulated here
So we finally arrive to the point where we put a scope in
We classify the endoscopic appearance of ulcers by the Forrest classification with great examples by @EndoscopyCampus endoscopy-campus.com/en/classificat…
The rebleeding rates (w/o therapy) are tabulated here

21/
Anything above IIa should be treated
We should try removing the clot in IIb and see what it becomes
In a MA, dual endoscopic therapy has largely superceded adrenaline injections alone
Anything above IIa should be treated
We should try removing the clot in IIb and see what it becomes
In a MA, dual endoscopic therapy has largely superceded adrenaline injections alone

22/
So what's the role of PPI after endoscopy?
2 RCTs again led by my mentors @CUHKMedicine showed that 72h of PPIs afterwards
⬇️Rebleeding
⬇️Need of Surgery
But didnt show a sig difference for reducing mortality

So what's the role of PPI after endoscopy?
2 RCTs again led by my mentors @CUHKMedicine showed that 72h of PPIs afterwards
⬇️Rebleeding
⬇️Need of Surgery
But didnt show a sig difference for reducing mortality


24/
Excellent reading materials for further interest
@BritSocGastro #AUGIB care bundle
fg.bmj.com/content/11/4/3…
A great updated review in DEN
onlinelibrary.wiley.com/doi/full/10.11…

Excellent reading materials for further interest
@BritSocGastro #AUGIB care bundle
fg.bmj.com/content/11/4/3…
A great updated review in DEN
onlinelibrary.wiley.com/doi/full/10.11…


25/
To conclude:
- risk stratification
- Mx: ABC and DAVIDS
- restrictive transfusion unless hemodynamically unstable, ischemic events
- ❌endoscopy if perforation, IO
- tx pre, during and post endoscopy
- balance risk and benefits on resumption of antiplatelets/anticoagulants
To conclude:
- risk stratification
- Mx: ABC and DAVIDS
- restrictive transfusion unless hemodynamically unstable, ischemic events
- ❌endoscopy if perforation, IO
- tx pre, during and post endoscopy
- balance risk and benefits on resumption of antiplatelets/anticoagulants
• • •
Missing some Tweet in this thread? You can try to
force a refresh