1/12 The jump from classroom teaching to clinical rotations is made tougher by the fact that physicians have illness-specific frameworks for presentations and documentation. Let's explore a bunch of them (feedback is most welcome)!
#MedTwitter #MedEd #FOAMed
#MedTwitter #MedEd #FOAMed
2/12 Let's start with anemia. It is ideal if you report the baseline Hgb and an interpretation of the MCV. #HemeTwitter 

3/12 For VTEs, it is helpful to tell the listener/reader if you think it is provoked vs. unprovoked. A hypercoagulable work-up should not be sent routinely. 

4/12 Next is heart failure. Reporting the medications with mortality benefit (for HFrEF) can be valuable in identifying if another medication needs to be started.
#CardioTwitter, thoughts on best practices?
#CardioTwitter, thoughts on best practices?

5/12 The anatomy of lesions in CAD, which arteries have been stented, and anti-platelet agents can be helpful. 

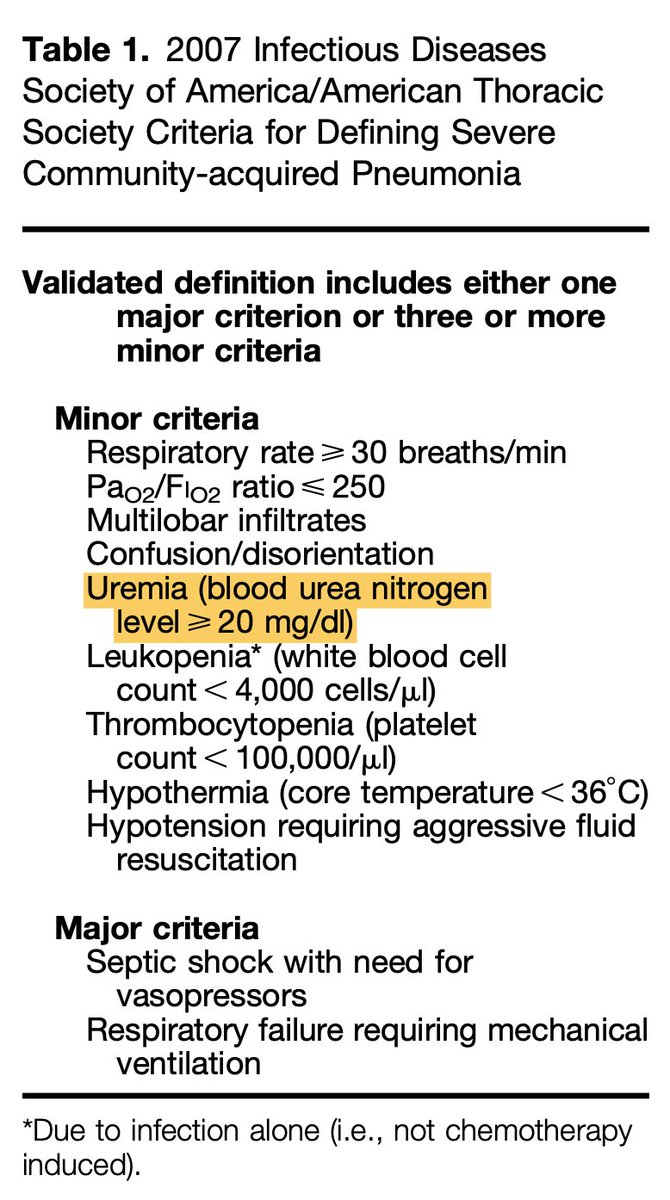
7/12 Next is sepsis! Here are some helpful qualifiers to stay organized (along with definitions of severe sepsis and septic shock) 

9/12 Next up is diabetes #EndoTwitter 

10/12 It is helpful to delineate pathologic from non-pathologic fractures as this helps delineate treatment options #OrthoTwitter 

11/12 COPD is up next! Remember that the goal O2 sat in patients with COPD is 88-92% to prevent uncoupling of compensatory hypoxic vasoconstriction #PulmTwitter 

12/12 Here is a compilation of all of them.
drive.google.com/file/d/1EAu5vy…
Please feel free to chime in with thoughts and additional illnesses that I can add to the list!
drive.google.com/file/d/1EAu5vy…
Please feel free to chime in with thoughts and additional illnesses that I can add to the list!
• • •
Missing some Tweet in this thread? You can try to
force a refresh