今天在 🇹🇼 #天下 @CWM_en 雜誌已刊出: "台灣抗疫成就 遠距工作、創新檢測成關鍵 "。 我與 @cptwei 寫了一篇有關建議 #Taiwan 對抗升 #COVID19 疫情的文章,主要是落實遠距工作、新的科學性篩檢方式。所有工作性質可以遠距辦公的員工,都必須改為遠距工作。重點如下 ⬇️ 1/6 opinion.cw.com.tw/blog/profile/5…
當前的台灣可說是提供了病毒滋養的溫床 — 尤其SARS-CoV-2 #Alpha (B.1.1.7)。依賴症狀的檢疫措施將會漏掉至少 50% 的病毒感染者。新型冠狀病毒會懸浮在空氣中並隨時間經過充斥整個房間。像辦公室這種通風不良的空調環境尤其危險。2/6 

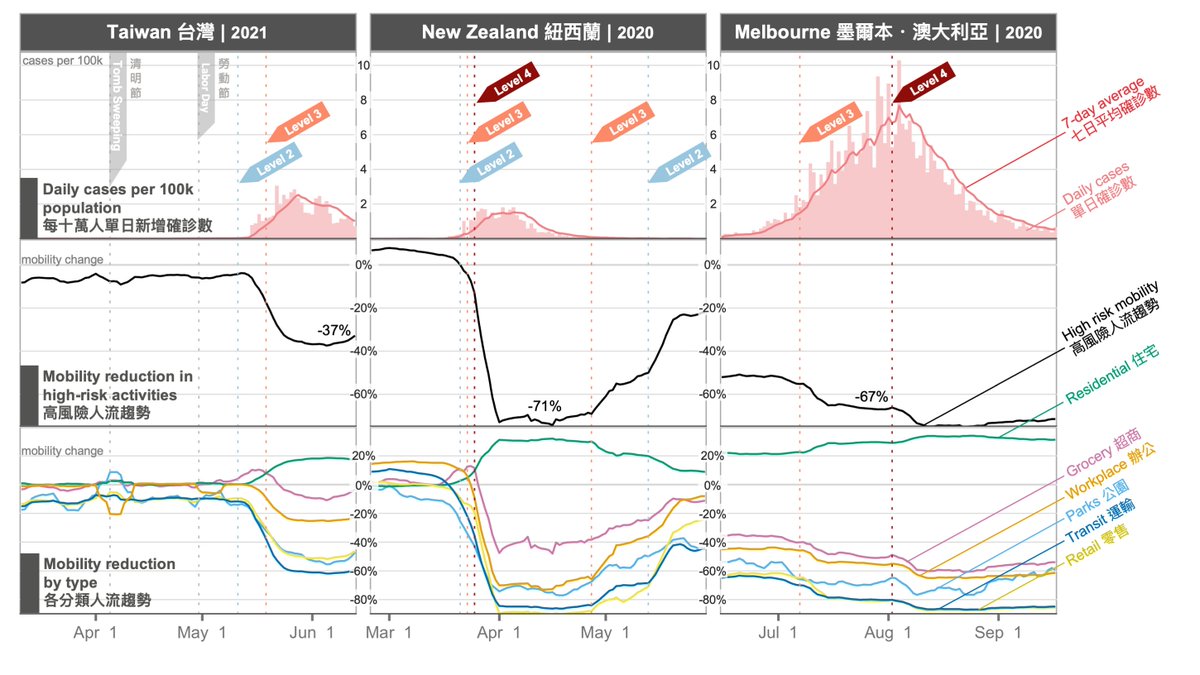
非必要地進公司辦公,會增加原可避免的傳染機會。特別是工作上的接觸通常是(應雇主要求)而非自願地,從四面八方聚集大量人群,並且持續相當長一段時間。應為社區人流居高不下。因此增加遠距辦公,我們確信 是控制這波爆發非常關鍵的政策。3/6 
依賴症狀的檢疫措施將會漏掉至少 50% 的病毒感染者。因此,需要擴展測試。有兩個選項可以大幅增加檢測量能和節省成本: 1)是使用檢體群檢測(pool testing),這是指兩個以上的樣本在PCR前混合; 2)即污水檢測。這個努力會有持續的回報,因為在可見的未來,新型冠狀病毒很可能會在人群中流通。4/6 

我們相信台灣可以繼續成為預防新冠肺炎的領導者,也必須如此,因為世界其他國家也正引頸企盼。🙏 感謝 @catielila 構思這件作品; @mitchlinmusic 負責視覺和編輯; @hsianglingg 翻譯; @kwangliu 編輯; 和 @Jim_Reynolds02 和許多其他人的出色反饋。台灣加油!6/6 

• • •
Missing some Tweet in this thread? You can try to
force a refresh














