The latest from our team:
A deep dive into the long-term consequences of #COVID19 on kidney function and disease
#longcovid #PASC
@VAResearch @vahsrd @WUSTL @WUSTLpubhealth @WUSTLmed @WUSTLnews @VREFSTL
@Biostayan @BCBowe @JASN_News @ASNKidney
jasn.asnjournals.org/content/early/…
🧵
A deep dive into the long-term consequences of #COVID19 on kidney function and disease
#longcovid #PASC
@VAResearch @vahsrd @WUSTL @WUSTLpubhealth @WUSTLmed @WUSTLnews @VREFSTL
@Biostayan @BCBowe @JASN_News @ASNKidney
jasn.asnjournals.org/content/early/…
🧵
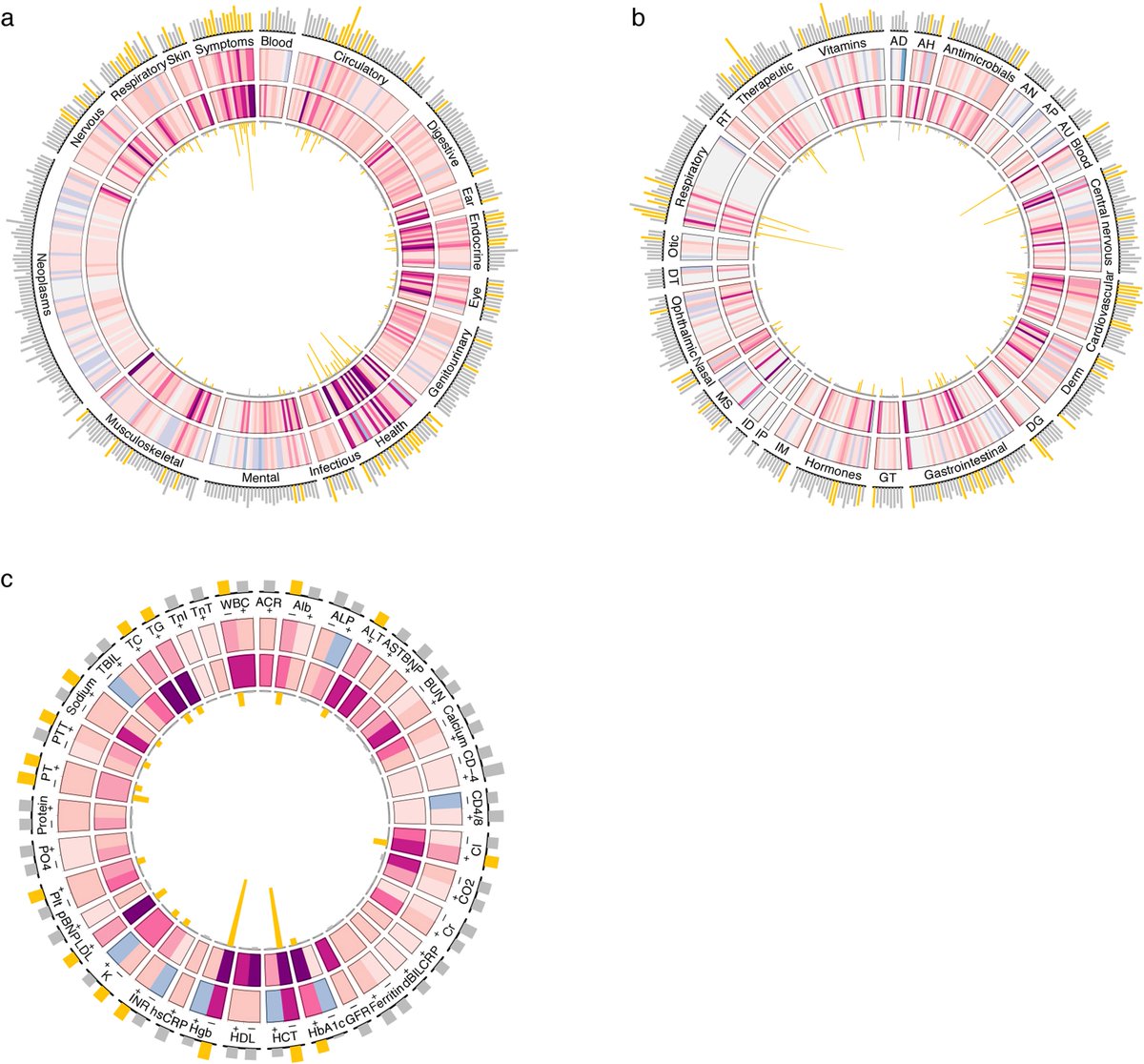
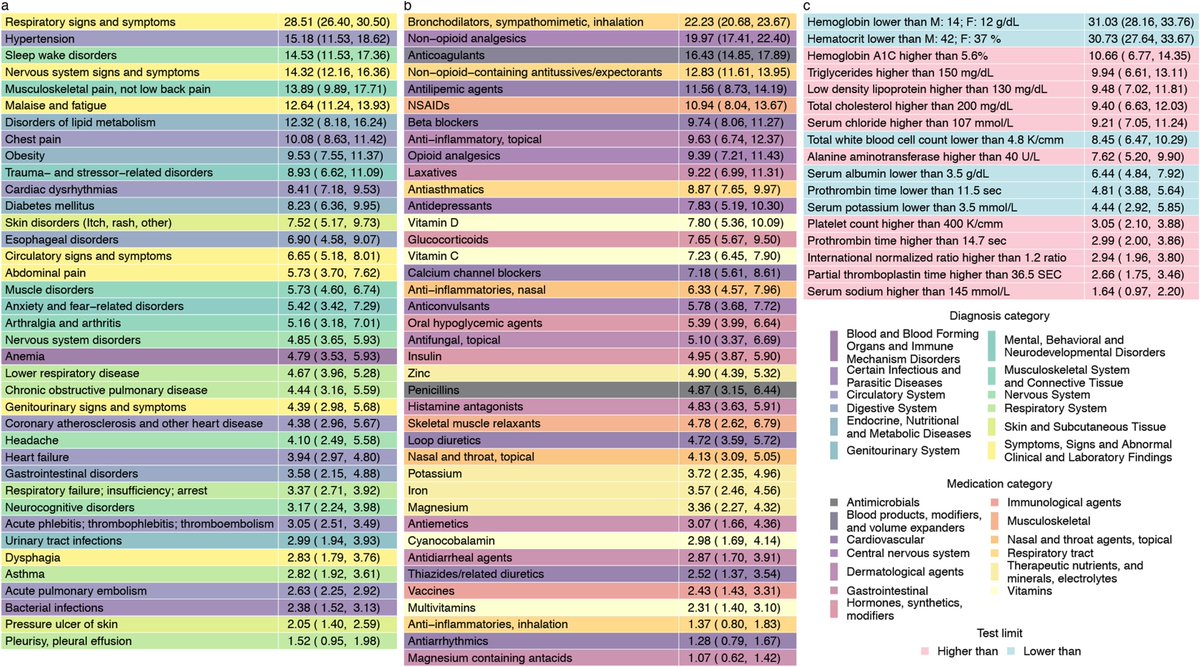
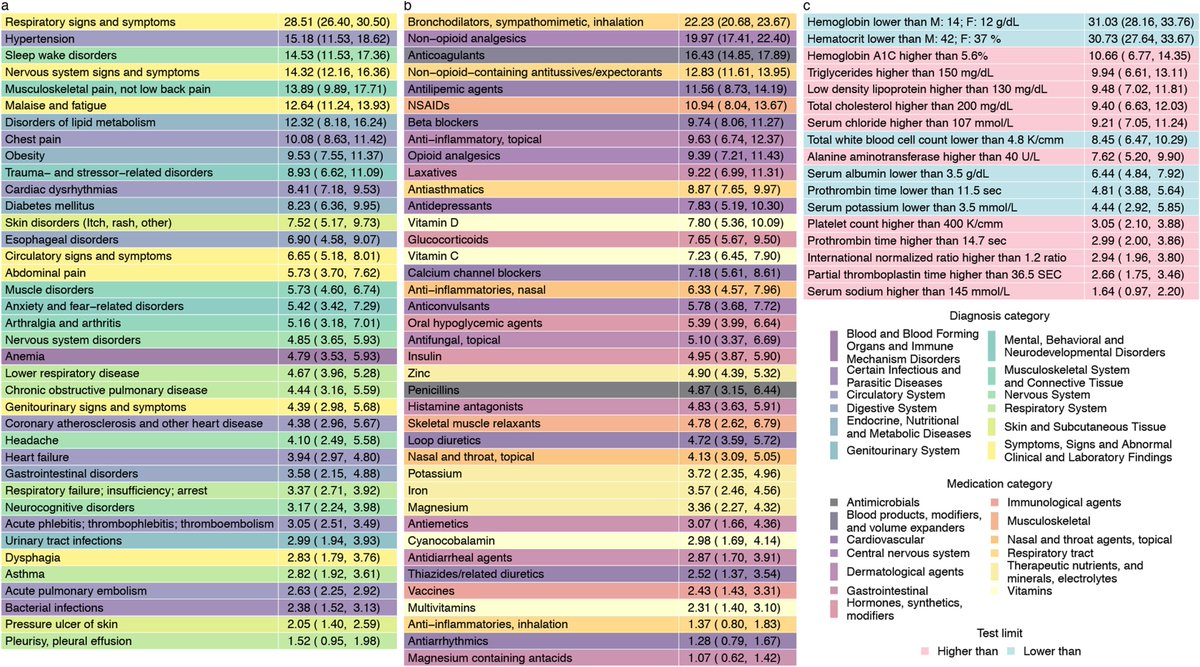
We previously provided a high dimensional characterization of post-acute sequelae of COVID-19
We showed that #LongCovid can affect nearly every organ system.
@Nature @NaturePortfolio
#COVID19 #PASC
nature.com/articles/s4158…
We showed that #LongCovid can affect nearly every organ system.
@Nature @NaturePortfolio
#COVID19 #PASC
nature.com/articles/s4158…
What happens to long term kidney function in people who survive acute #COVID19 ?
And are they at increased risk of #kidney disease?
To address this, we built a cohort of 89,216 US veterans with #COVID19 and 1,637,467 non-infected controls.
jasn.asnjournals.org/content/early/…
And are they at increased risk of #kidney disease?
To address this, we built a cohort of 89,216 US veterans with #COVID19 and 1,637,467 non-infected controls.
jasn.asnjournals.org/content/early/…
In the post-acute phase of COVID-19 #PASC , there were increased risks and burdens of:
Acute Kidney Injury (#AKI)
Kidney function decline (#eGFR decline >30, 40, 50%),
End Stage Kidney Disease (#ESKD)
Acute Kidney Injury (#AKI)
Kidney function decline (#eGFR decline >30, 40, 50%),
End Stage Kidney Disease (#ESKD)
The risks and burdens were higher in people who were hospitalized during the acute phase, and highest in those who needed ICU care during the acute phase.
But risks were evident even in those non-hospitalized (these people represent the majority of people with #COVID19).
But risks were evident even in those non-hospitalized (these people represent the majority of people with #COVID19).
People who were hospitalized and had acute kidney injury #AKI during the acute phase are at highest risk of poor kidney outcomes.
The risk was lower in people who did not have #AKI during the acute phase.
But again, risk was evident (and not trivial) among non-hospitalized.
The risk was lower in people who did not have #AKI during the acute phase.
But again, risk was evident (and not trivial) among non-hospitalized.
Compared to non-infected controls, 30-day COVID-19 survivors exhibited excess eGFR decline of -3.26 (-3.58, -2.94), -5.20 (-6.24, -4.16), and -7.69 (-8.27, -7.12) mL/min/1.73m2/year in non-hospitalized, hospitalized, and those in ICU during the acute phase of COVID-19 infection.
Summary:
What happens to the kidneys in survivors of COVID-19?
Increased risks of:
- Acute kidney injury
- Decline in kidney function
- End-stage kidney disease
jasn.asnjournals.org/content/early/…
What happens to the kidneys in survivors of COVID-19?
Increased risks of:
- Acute kidney injury
- Decline in kidney function
- End-stage kidney disease
jasn.asnjournals.org/content/early/…
Implications:
Kidney disease is a facet of the multifaceted #LongCovid #PASC
Post-acute care of people who had COVID-19 should involve attention to kidney function and disease.
Multidisciplinary post-acute COVID care clinics should include kidney care component
Kidney disease is a facet of the multifaceted #LongCovid #PASC
Post-acute care of people who had COVID-19 should involve attention to kidney function and disease.
Multidisciplinary post-acute COVID care clinics should include kidney care component
• • •
Missing some Tweet in this thread? You can try to
force a refresh