Do You keep slamming Your face because You missed the 1st #HFA @escardio Clinical Practice Update Course on #HeartFailure, orchestrated masterfully by MC Mullens?
Are You particularly disappointed to have missed the clinical pearls of #HFA giants @kevin_damman & @FinnGustafsson?
Are You particularly disappointed to have missed the clinical pearls of #HFA giants @kevin_damman & @FinnGustafsson?
Catch up for 2 months on the platform on demand: escardio.org/Education/Cour…
I'll release just a teaser under the form of a clinical case below. You might call on my partners in crime @Ph_Bertrand & @petranijst to do the same...
Have fun & see you live without #COVID next year!
I'll release just a teaser under the form of a clinical case below. You might call on my partners in crime @Ph_Bertrand & @petranijst to do the same...
Have fun & see you live without #COVID next year!
@Ph_Bertrand @petranijst 61 y/o woman
PMH: Chronic HCV, hypertension, poorly controlled diabetes (HbA1c 9.6%), obesity (BMI 32 kg/m²)
Currently no meds
Found in apartment with motoric aphasia & right hemiplegia due to ischemic stroke (middle cerebral artery)
R/No thrombolysis (subacute), thrombectomy!
PMH: Chronic HCV, hypertension, poorly controlled diabetes (HbA1c 9.6%), obesity (BMI 32 kg/m²)
Currently no meds
Found in apartment with motoric aphasia & right hemiplegia due to ischemic stroke (middle cerebral artery)
R/No thrombolysis (subacute), thrombectomy!

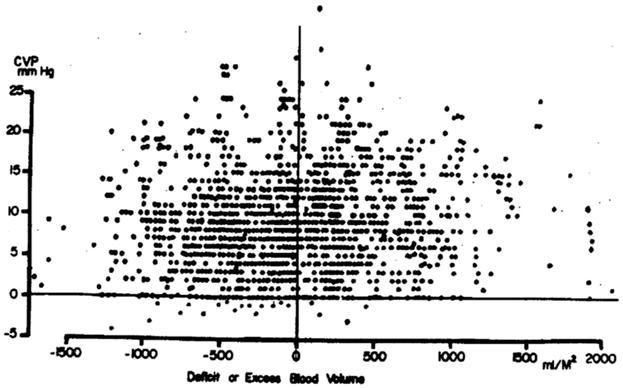
Chest X-ray shows cardiomegaly with signs of congestion... Severe orthopnoea, jugular venous distension, bilateral oedema... 

Further history:
- Stable NYHA II, but progressively worse breathlessness for 10 days
- No chest pain
- No familial history
- Drinks half a bottle of wine every day
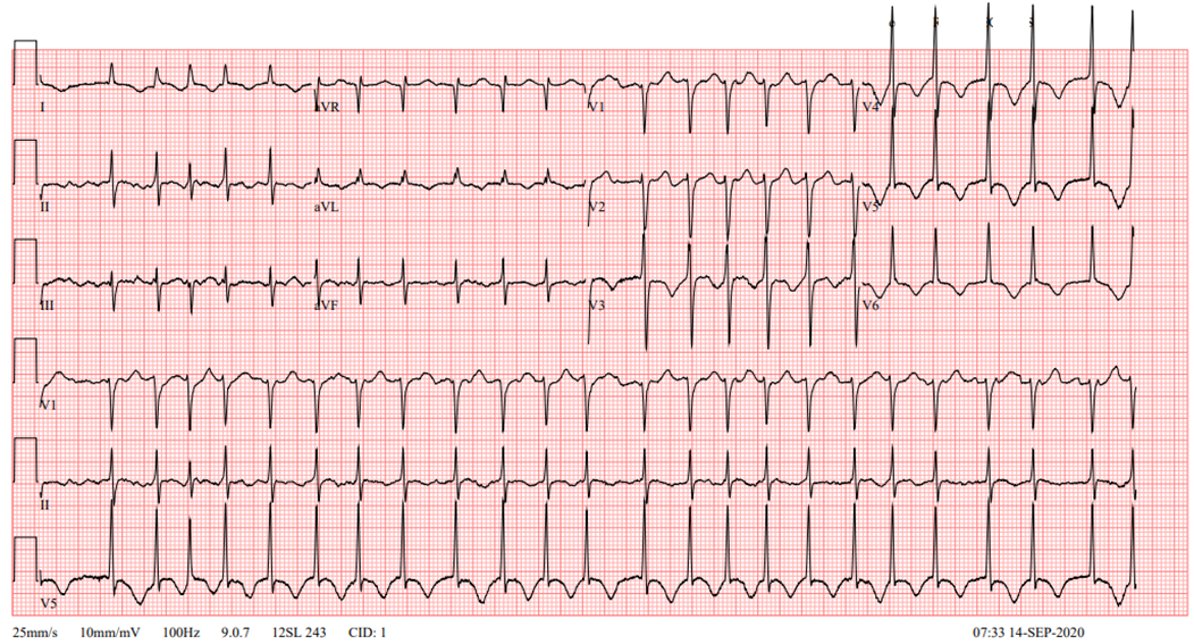
BP: 103/74 mmHg
HR: 130 /min
- Stable NYHA II, but progressively worse breathlessness for 10 days
- No chest pain
- No familial history
- Drinks half a bottle of wine every day
BP: 103/74 mmHg
HR: 130 /min
Bonus question 1: Most likely hemodynamic profile
However, be wary of a pulse pressure of only 29 mmHg in this case, this patient is likely cold even before You see the echo. Look at that EF:
There's some #MR as well, probably moderate at first look:
What would You do?
We clearly want to diurese this patient. Trying to convert to sinus rhythm is likely not going to be effective in a case like this.
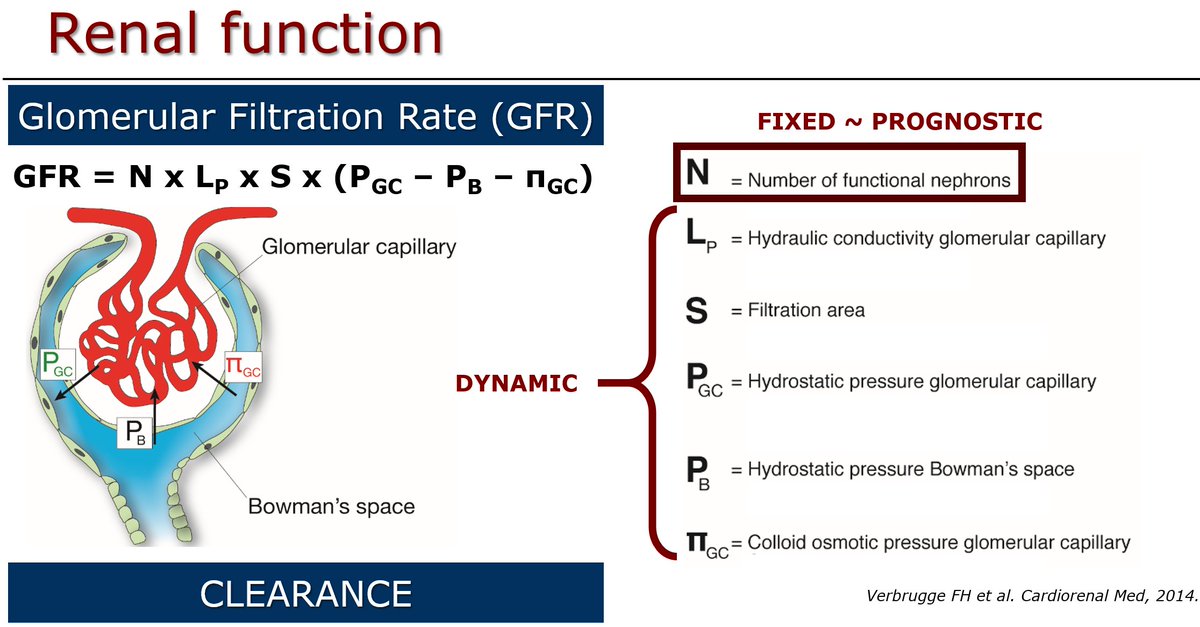
BUT... kidneys can only excrete what they receive from the heart!
1st restore kidney perfusion
2nd open the floodgates...
BUT... kidneys can only excrete what they receive from the heart!
1st restore kidney perfusion
2nd open the floodgates...
My biggest disappointment in the new guidelines: underappreciation of what vasodilators can do...
#SBP pretty useless for decision making
This case: low SBP, rather high DBP, low PP with MAP 84 mmHg (!)
With elevated filling pressures this can only mean vasoconstriction...
#SBP pretty useless for decision making
This case: low SBP, rather high DBP, low PP with MAP 84 mmHg (!)
With elevated filling pressures this can only mean vasoconstriction...
So we started nitroprusside, uptitrated towards 130 µg/min IV:
SBP: 103 => 109 mmHg
DBP: 74 => 54 mmHg
MAP: 86 => 72 mmHg
Sv02: 48% => 67%
Now we started IV diuretics, patient is 5L negative...
SBP: 103 => 109 mmHg
DBP: 74 => 54 mmHg
MAP: 86 => 72 mmHg
Sv02: 48% => 67%
Now we started IV diuretics, patient is 5L negative...
What do we need to complete the diagnostic work-up?
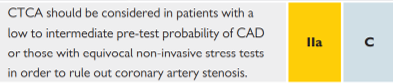
We want to exclude ischaemic heart disease don't we?
- HCV is risk factor
- Obesity & diabetes as well
- Hypertension
- 61 y/o
Guidelines push us more towards CT and I would tend to agree
- HCV is risk factor
- Obesity & diabetes as well
- Hypertension
- 61 y/o
Guidelines push us more towards CT and I would tend to agree
But... Are Your waiting lists for CCT also exploding? We just have so much easier access to coronary angiography, so that is what we ended up doing...
Posterior descendens lesion was stented (DES), otherwise no significant stenoses...
Posterior descendens lesion was stented (DES), otherwise no significant stenoses...
What's the diagnosis?
Probably, we can't tell for sure at this moment. But it ain't no ischemic CMP for sure! Because there are several #HFpEF risk factors (below) and a relatively preserved RV, tachyCMP remains high on my list 

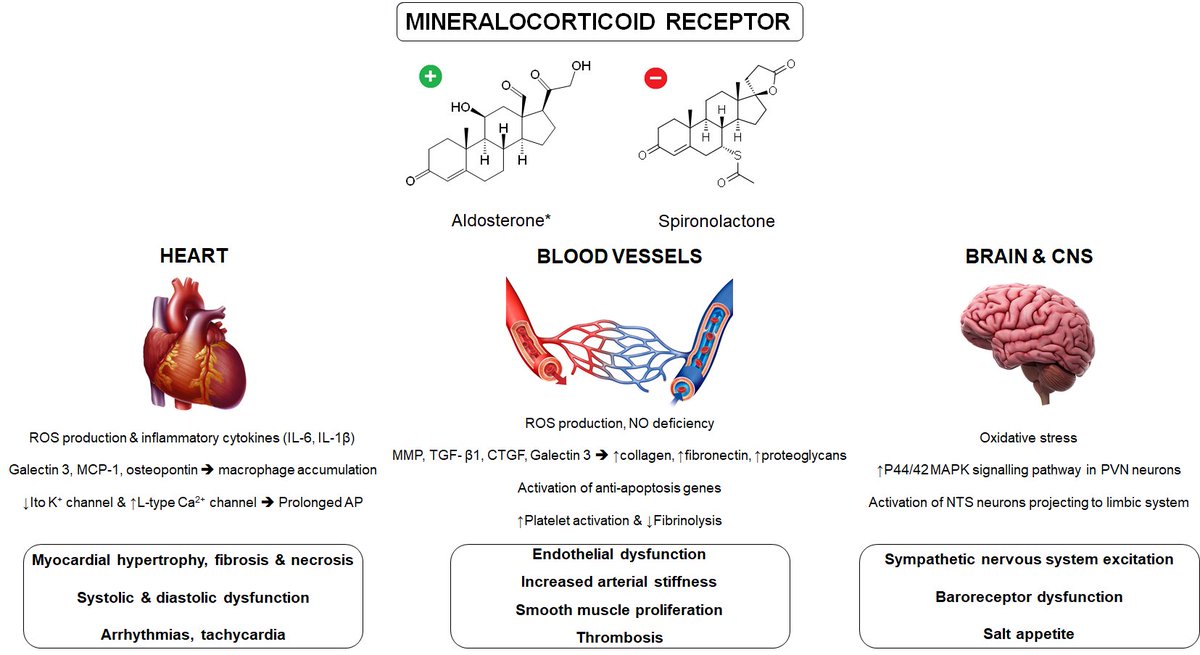
#SGLT2i & #MRA were introduced during decongestive treatment. Patient now is dry and on oral meds:
- Heparin (DOAC to be started at discharge)
- Dapagliflozin 10 mg OD
- Spironolactone 25 mg OD
- Bisoprolol 1.25 mg OD
- Digoxin 0.125 mg OD
BP 92/63 mmHg; HR 123 bpm, still in AF
- Heparin (DOAC to be started at discharge)
- Dapagliflozin 10 mg OD
- Spironolactone 25 mg OD
- Bisoprolol 1.25 mg OD
- Digoxin 0.125 mg OD
BP 92/63 mmHg; HR 123 bpm, still in AF
What's next?
LVEF is poor, there might be a temporal relationship between #Afib & loss of LV function, this is probably a case for rhythm control (IIa-B recommendation in the new guidelines).
We went straight for ablation because we were really stuck for uptitration of beta blocker & ARNi
We went straight for ablation because we were really stuck for uptitration of beta blocker & ARNi
Immediately after ablation, managed to add low dose losartan (25 mg OD) & uptitrate bisoprolol to 2.5 mg OD.
After one month:
- regained some functionality in leg, normal speech
- BMI 23 kg/m²
- HbA1c 5.4%
- No congestion
- BP 112/73 mmHg
- Holter 44-138 bpm, no ectopy
- EF 30%
After one month:
- regained some functionality in leg, normal speech
- BMI 23 kg/m²
- HbA1c 5.4%
- No congestion
- BP 112/73 mmHg
- Holter 44-138 bpm, no ectopy
- EF 30%
Final question:
This is after switching to ARNi and uptitrating slowly towards 103/97 mg BID 8 months after the initial presentation:
MR has disappeared by the way... Final diagnosis tachycardiomyopathy. You might discuss with your patient if You want to do genetics. Not entirely unlikely that You would find a TTN mutation here... Shared decision-making!
• • •
Missing some Tweet in this thread? You can try to
force a refresh