Lung Ultrasound #LUS 2/10
#IVC long axis 3/10
#IVC short axis + tilting 4/10
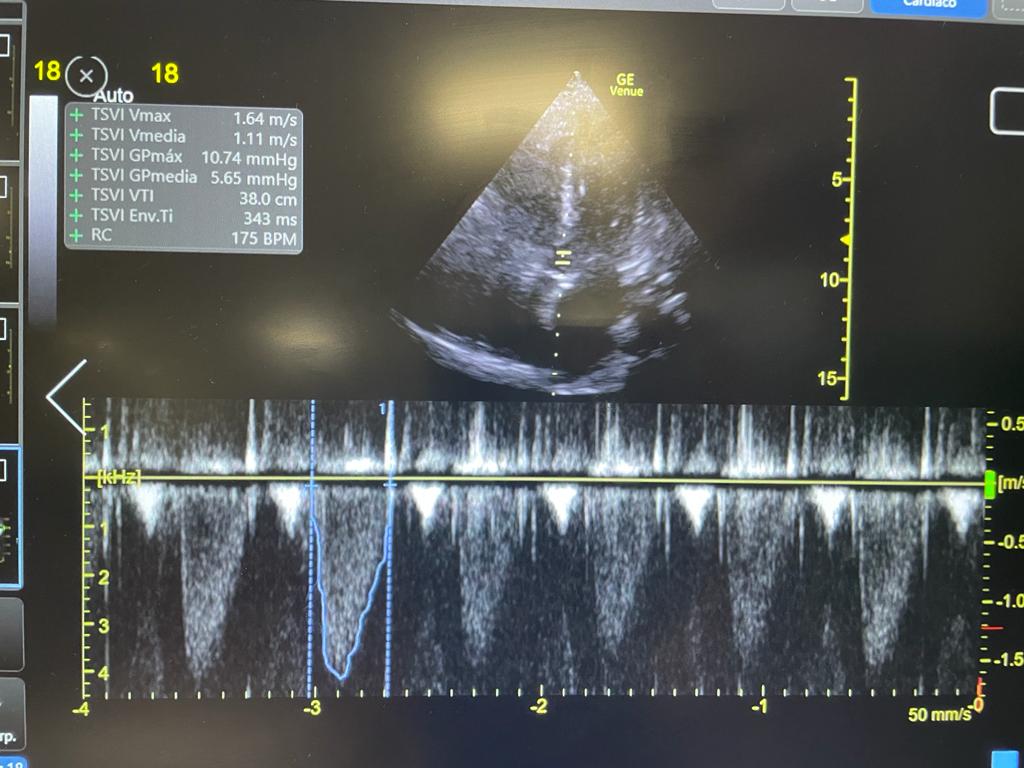
#echofirst PLAx + A4ch 5/10
Hepatic Vein Color Doppler 6/10
Kidneys 8/10
Impression:
Dry lungs, IVC with intramural tumor extending to the right atrium. LV OK. No flow on IVC or HV. Low stroke volume. Normal right kidney (some free fluid). Left kidney tumor
9/10
Dry lungs, IVC with intramural tumor extending to the right atrium. LV OK. No flow on IVC or HV. Low stroke volume. Normal right kidney (some free fluid). Left kidney tumor
9/10
There is severe leg edema with low preload (low stroke volume, no lung edema) and no flow in the IVC
This is Inferior Vena Cava Syndrome!
Cause is RCC invading the IVC and RA
Nice review here: doi.org/10.7326/0003-4…
END/
This is Inferior Vena Cava Syndrome!
Cause is RCC invading the IVC and RA
Nice review here: doi.org/10.7326/0003-4…
END/
• • •
Missing some Tweet in this thread? You can try to
force a refresh