
How come #COVID19 is mostly mild in children? And why do #MISC affect mostly young people?
An interesting hypothesis by @BrodinPetter considering the trade-off between growth and immunity, while most of the studies focus on resistance rather than tolerance 1/
An interesting hypothesis by @BrodinPetter considering the trade-off between growth and immunity, while most of the studies focus on resistance rather than tolerance 1/
Tolerance to the initial infection may allow virus to stay in gut longer, leak through gut wall, and trigger T cell activation. Could a milder systemic immune response lead to viral persistence in the gut of children? 2/ 



“Energy allocation for growth increases the threshold to mount expensive systemic inflammatory responses unless absolutely required”
3/
3/
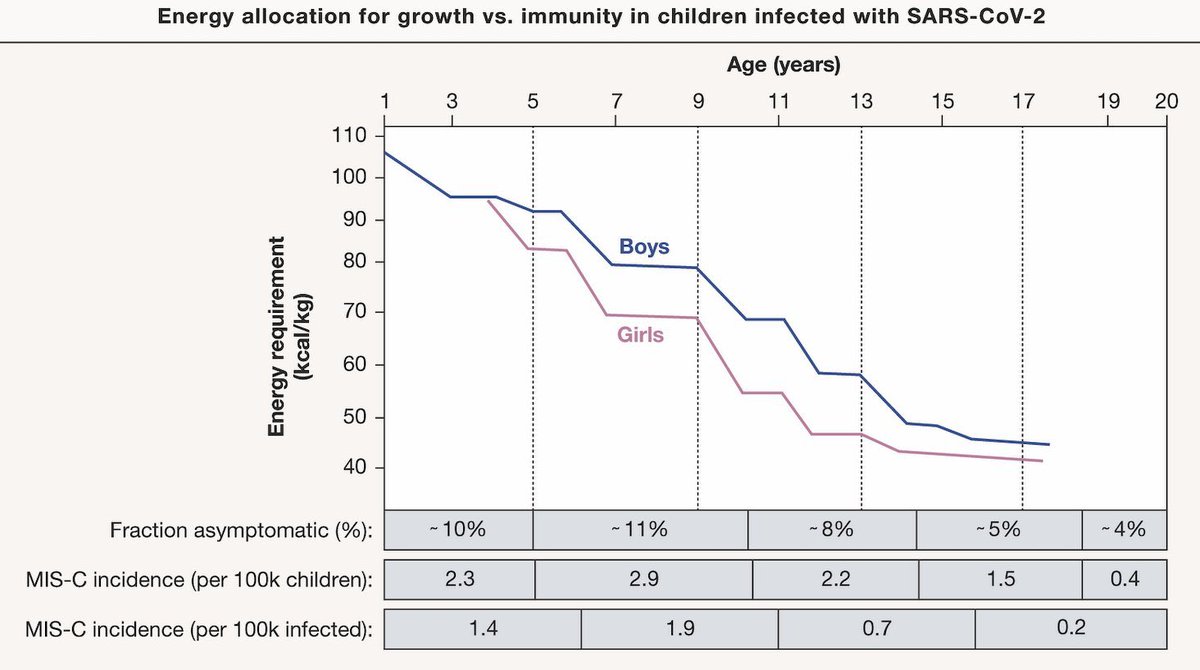
Indeed a thought provoking hypothesis of why kids can have mild COVID then develop severe MIS-C weeks to months later. Tolerance to the initial infection may allow virus to stay in gut longer, leak thru gut wall, & trigger T cell activation. 4/
https://twitter.com/brodinpetter/status/1483868478851452928?s=21
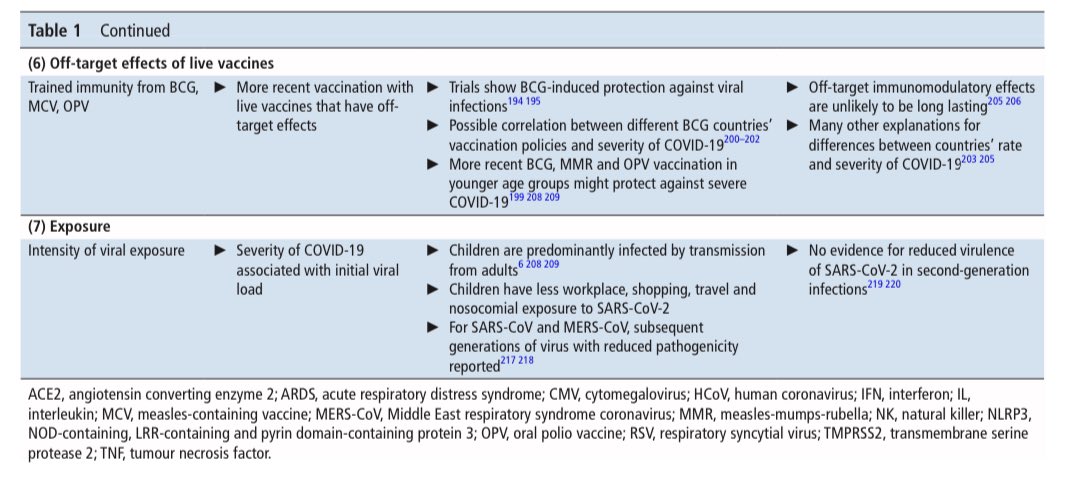
There is an earlier review on, “Why is COVID-19 less severe in children?” The review also discusses the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections 5/
adc.bmj.com/content/archdi…


adc.bmj.com/content/archdi…


• • •
Missing some Tweet in this thread? You can try to
force a refresh







