1) Welcome to a new #accredited #tweetorial on a🗝️ topic in #cancer care & #vascular medicine: #VTE (#DVT and #PE). Cancer patients are at⬆️risk from their disease, their comorbidities, & often from their treatment. It's a sticky wicket & @cardiomet_CE is proud to welcome ...
2) ... one of the world's leading authorities on cancer-associated VTE as new faculty both here and on @onc_ce: Dr. Alok Khorana @aakonc of @ClevelandClinic, to talk about advances and best treatment in this space! 

3) This educational program is intended for health care providers & is supported by a grant from Bristol Myers Squibb & its Alliance partner Pfizer, Inc. Faculty disclosures are listed at cardiometabolic-ce.com/disclosures/. Earn CE/#CME credit from prior programs at cardiometabolic-ce.com.
4) Let's start with a case. 67M retired schoolteacher w/remote history of smoking but no other significant comorbidities presents w/upper abdominal pain radiating to the back + weight loss. CT abdomen reveals mass in pancreas+liver mets. #FNA confirms #pancreaticadenocarcinoma.
5) Pt starts chemo with FOLFIRINOX; restaging CT chest after cycle 4 shows bilateral segmental #PE. On questioning, pt has fatigue but no chest pain or #SOB. Should #incidental #PE be treated with anticoagulation? Mark your answer before scrolling⬇️!
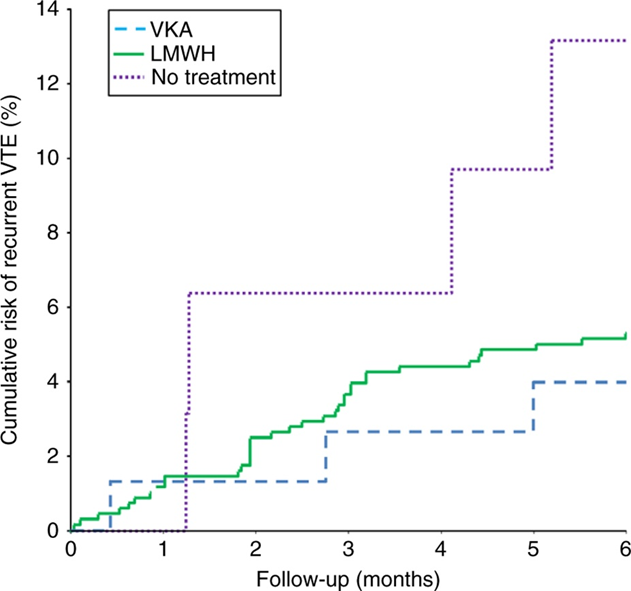
6) The correct answer is a., full-dose. A large pooled analysis of incidental #PE found recurrent #VTE was lower with anticoag LMWHs or vitamin K antagonists (6.2% or 6.4%), compared to 12% in untreated patients (HR 2.6; 95% CI 0.91-7.3)
🔓pubmed.ncbi.nlm.nih.gov/26469193/
🔓pubmed.ncbi.nlm.nih.gov/26469193/
7) Current @ASCO guidelines recommend treating incidentally diagnosed #PE in #cancer patients with anticoagulation as well “Rec 4.7 Incidental PE and DVT should be treated in the same manner as symptomatic VTE, given . . .
8) . . . their similar clinical outcomes compared with patients with cancer with symptomatic events”
🔓ascopubs.org/doi/10.1200/JC…
🔓ascopubs.org/doi/10.1200/JC…
9) There are less data for isolated subsegmental #PE or visceral vein thrombi (e.g., portal vein thrombus) so @ASCO recommends anticoagulation on a case-by-case basis
🔓ascopubs.org/doi/10.1200/JC…
🔓ascopubs.org/doi/10.1200/JC…
10) Now that you’ve made a decision to anticoagulate, which agent should you choose?
11) Well, there are 2 time-related aspects to treatment – initial (first few days) and long-term (up to 6 mos, or longer)
12) For initial treatment – if pt requires admission, @ASCO guidelines prefer #LMWH over #UFH. Otherwise, #DOACs (#apixaban, #rivaroxaban) or LMWH transitioning to warfarin or LMWH monotherapy are all acceptable options . . . but let’s break down pros/cons
13) What about d., aspirin? Trick choice - Aspirin should obviously never be chosen for treatment.
14) c. Warfarin? That's also tricky due to drug-drug interactions with 5FU+others, need for INR monitoring but may be appropriate choice in low- & middle-income countries #LMIC or other financial 💰 considerations
15) Between LMWH and DOACs, we now have several #RCTs to provide evidence, which is great! Most recent meta-analysis is here: sciencedirect.com/science/articl…
It's🚫open access so here are some details: 4 RCTs in pts w/cancer+VTE comparing a factor Xa inhibitor (FXaI) to LMWH.
It's🚫open access so here are some details: 4 RCTs in pts w/cancer+VTE comparing a factor Xa inhibitor (FXaI) to LMWH.
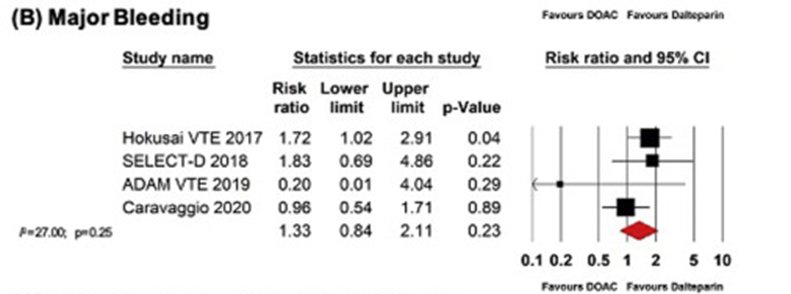
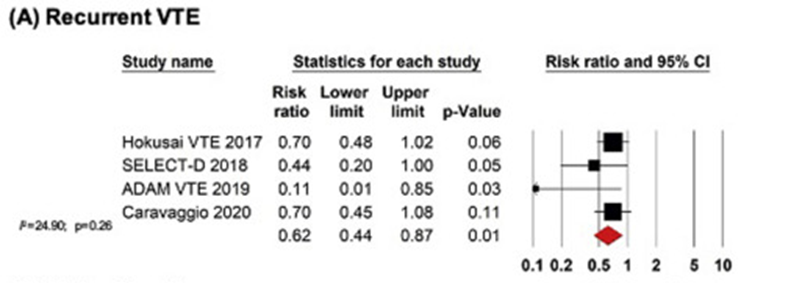
16) A meta-analysis was performed with a primary outcome of VTE recurrence & key secondary outcomes of major bleeding, clinically relevant non-major bleeding #CRNMB & #gastrointestinal bleeding #GIB. VTE recurrence was lower in the FXaI group, w/absolute risk difference of -4%.
17) That's a #NNT of 25 for prevention of rec VTE with FXaI, & there was no sig diff in major bleeding between groups, tho rates of #GIB and #CRNMB were greater with FXaIs. Conclusion: in pts w/cancer+VTE, VTE recur is sig lower w/FXaI than w/LMWH w/o⬆️risk of major bleeding.
18) In general, DOAC studies suggest improvement in recurrent VTE vs LMWH (which already previously showed improvement in rec VTE over warfarin) 
20) If you look closely, increased major bleeding was primarily driven by #GIcancers (but really primarily luminal GI cancers) and noted in earlier trials but not in the more recent trials (?selection vs drug).
21) For our patient with pancreatic cancer, risk of major bleeding is not substantially increased with DOAC. In our experience @ClevelandClinic, pts prefer convenience (and lower cost) of DOAC vs LMWH (yes, even generic is more expensive).
22) Tune in tomorrow to discuss whether this patient's #PE could have been prevented!
Nods to @ThrombosisCan @AlbertaPHdoc @LaurentBertole1 @ilyassahinMD @MarcCarrier1 @AggieLeeMD @SimonNoble @jzbos @cihan_ay_MD
Nods to @ThrombosisCan @AlbertaPHdoc @LaurentBertole1 @ilyassahinMD @MarcCarrier1 @AggieLeeMD @SimonNoble @jzbos @cihan_ay_MD
23) Welcome back! You are earning 0.5h CE/#CME for #physician #physicianassociate #nurses #nursepractitioner #pharmacist while you are engaged with expert faculty @aakonc of @ClevelandClinic, who us teaching us about #VTE associated with #cancer. Hello @bhwords @ProfMakris @isth
24) Case reminder: 67M diagnosed with #pancreaticcancer developed #PE 2 months after 1L therapy with FOLFIRINOX. Could this have been prevented?
25) Prevention of #VTE is well-known in many settings e.g., post #orthopedics surgery, in-hospital, post-abd surgery etc. In #cancer patients, VTE prevention can be considered as well.
26) Although #VTE prophylaxis is used mostly in post-surgical and inpatient settings in pts with cancer, most VTEs actually occur in outpatient setting (since most systemic therapy for cancer is outpatient)
27) #VTE prevention is important because rates have recently been shown to be rising. ashpublications.org/blood/article/… 
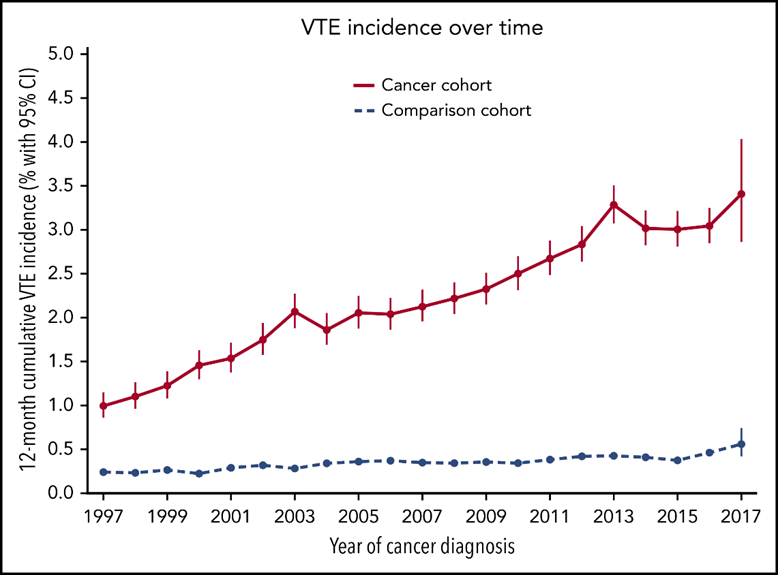
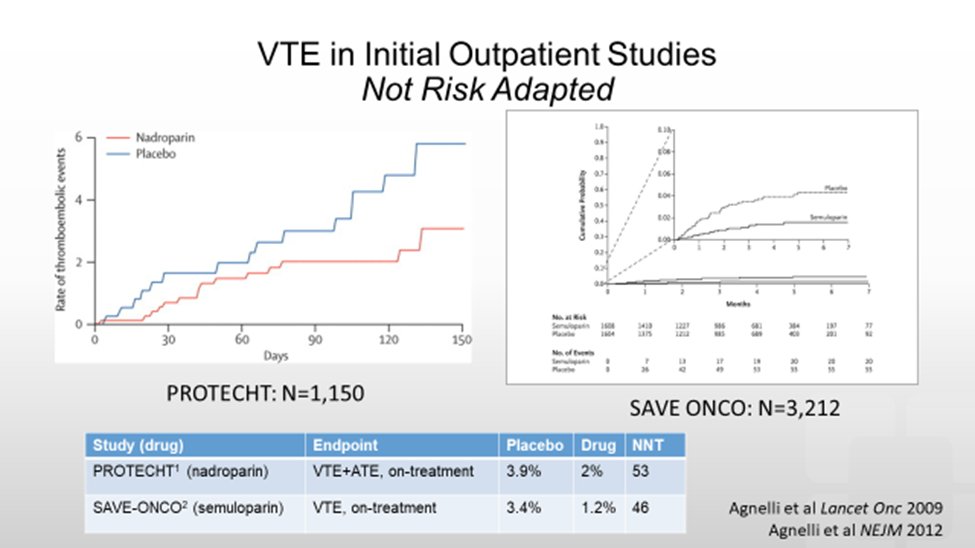
28) Initial studies using LMWH prophylaxis showed statistically significant reduction in #VTE but rates were low since patients were not selected based on risk 
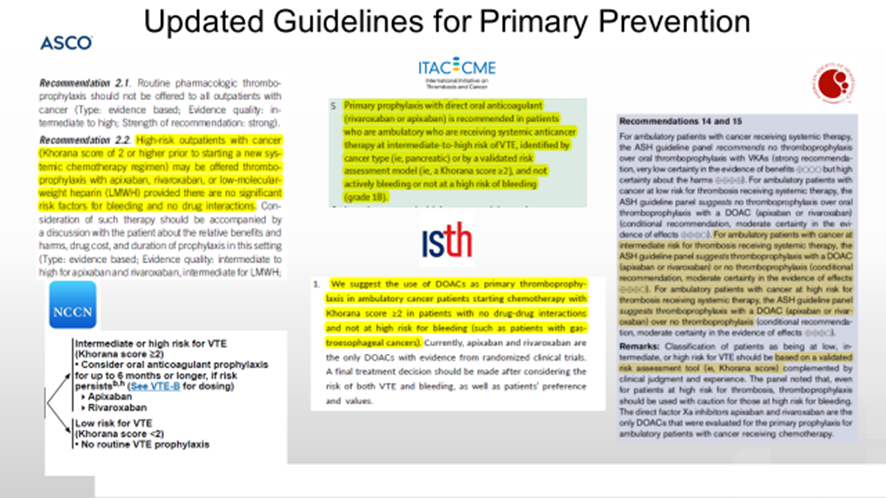
29) In 2008, we @aakonc @gary_lyman @NicoleKuderer published the first risk assessment model to identify pts at higher risk for #VTE 
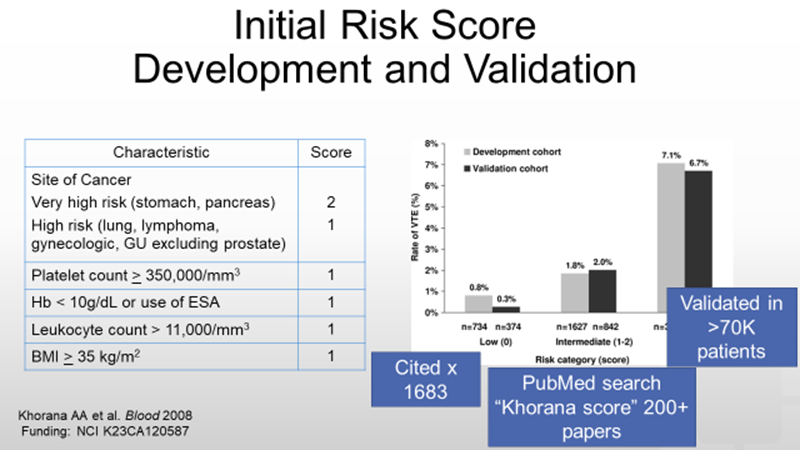
30) Validation has occurred in over 70K patients, first by Vienna grp @Cihan_Ay_MD & most recently in an Asian population (with modification for BMI) 



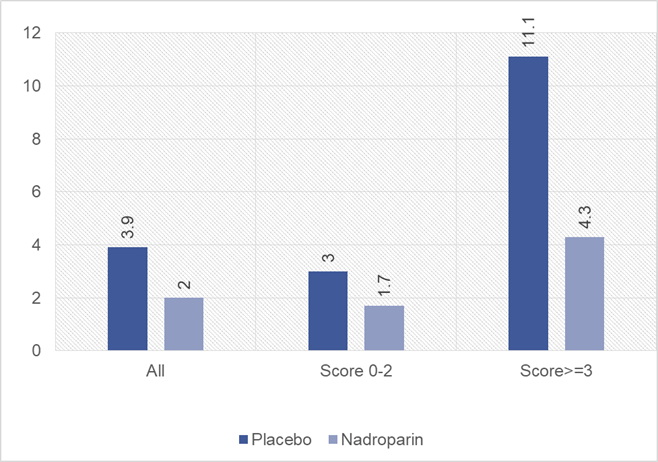
31) When you apply risk stratification to some of the older studies, you get much greater absolute and relative benefit for patients, eg in #PROTECHT study by Verso et al
link.springer.com/article/10.100…
link.springer.com/article/10.100…
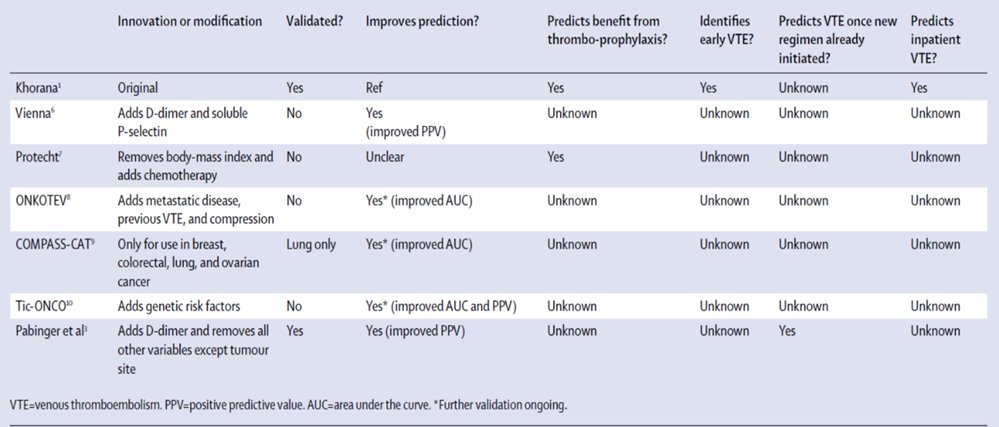
32) 14 yrs later, there are now multiple risk tools (listed here, in various stages of validation). Esp validated is #Viennascore by Pabinger, @cihan_ay_MD, et al
🔓thelancet.com/journals/lanha…
🔓thelancet.com/journals/lanha…
33) Prospective #RCTs confirm benefit and safety of outpatient #DOAC/#LMWH prophylaxis in patients at higher risk for VTE as shown in this pooled analysis by Bosch et al of 6 RCTs 🔓ashpublications.org/bloodadvances/… 
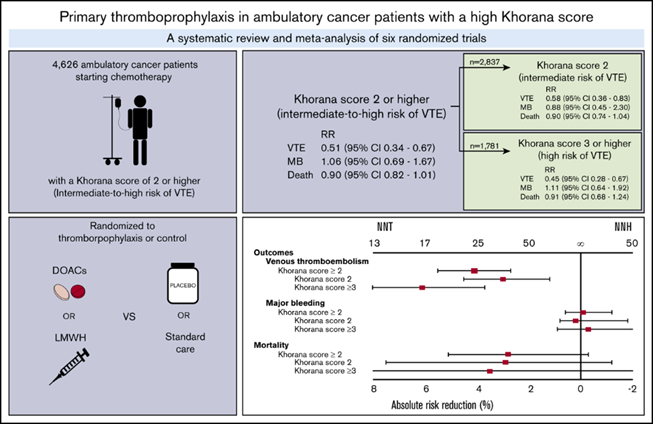
34) Specifically in #GIcancers (like our case), subgroup analysis of #AVERT showed substantial benefit with apixaban prophylaxis (4.6% VTE w/apixaban vs 20% w/placebo; 1 excess major bleed with apixaban NS) sciencedirect.com/science/articl…
35) Thus, there is ample evidence from multiple RCTs (including some specifically for pancreatic cancer) that prophylaxis is beneficial
36) Regardless, I often get “devil’s advocate” Qs that since prophylaxis does not improve OS it is not necessary to use. But this is a standard not applied to, say, anti-emetics or bone-strengthening agents. Reduction of VTE is a good for patients, regardless of impact on OS.
37) All relevant guidelines now recommend consideration of primary prevention with #DOAC or #LMWH for a pt such as the one discussed in our case. Key now is to implement! 
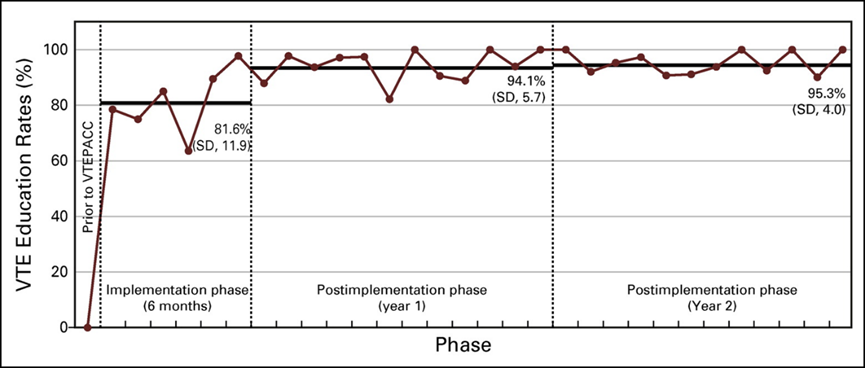
38) A terrific model for #implementationscience comes from Vermont @ChrisHolmesMD where 94% of at-risk pts went on outpt prophylaxis slaying myth that cancer pts are not interested in outpt prevention @StopTheClot @lesllake @BethWaldron
🔓ascopubs.org/doi/full/10.12…
🔓ascopubs.org/doi/full/10.12…
39) And that's it, you made it! FREE CE/#CME! Just point your 🖱️to cardiometabolic-ce.com/antithrombotic… and grab your certificate! And FOLLOW us at @cardiomet_ce and at @onc_ce for more expert-led programs such as this!
@academiccme #FOAMed @MedTweetorials @ckd_ce @Myeloma_Doc @AlexSpyropoul
@academiccme #FOAMed @MedTweetorials @ckd_ce @Myeloma_Doc @AlexSpyropoul
• • •
Missing some Tweet in this thread? You can try to
force a refresh