1) Welcome to a new #accredited #tweetorial on managing #VTE at the extremes of weight & renal function. Free CE/#CME credit for following along with expert author @AryaRoopen from King’s Thrombosis Centre at King's College Hospital in London! Only the best for our learners! 

2) When we think about "special populations" in #VTE, we think weight, age, and #cancer status. @aakonc already addressed the last of those (earn credit still at cardiometabolic-ce.com/antithrombotic…). Learn the rest here! Hello to @ProfMakris @bhwords @MiddeldorpS @fniainle @AliTaherMD
3) This educational program is intended for health care providers & is supported by a grant from Bristol Myers Squibb & its Alliance partner Pfizer, Inc. Faculty disclosures at cardiometabolic-ce.com/disclosures/. Credit for #physicians #physicianassociates #nurses #NPs #pharmacists
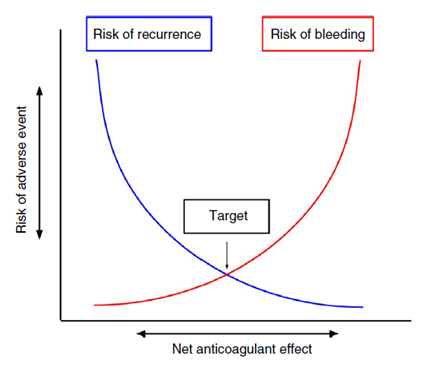
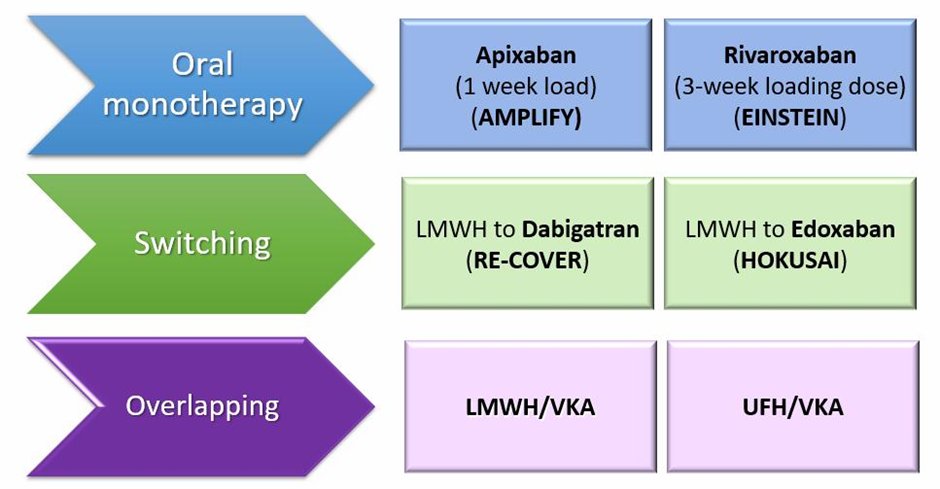
4) Treatment options for #VTE include initial use of heparin (usually low molecular weight heparin, #LMWH) overlapping with #warfarin, or initial LMWH switching to direct oral anticoagulant (#DOAC) or DOAC monotherapy. For most patients DOACs are the treatment of choice. 
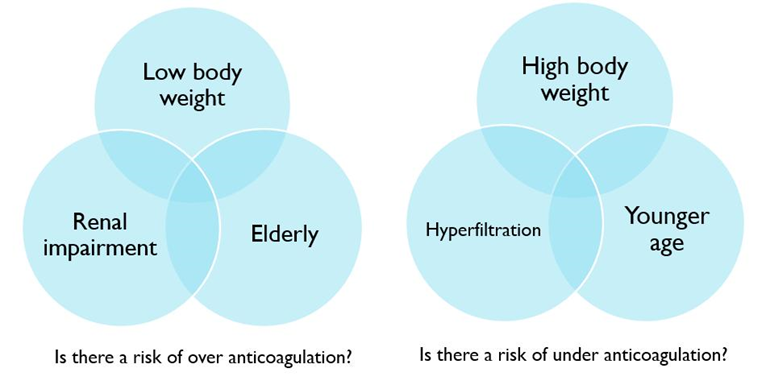
5) Treatment at extremes of body weight and/or #renal function can be challenging. What are the treatment options and what evidence is there to support them? 
6) Why limited data at extreme subgroups? Unfortunately these patients are under-represented in Ph3 clinical trials (lower proportion in population, exclusion criteria, recruitment bias). Under-representation = lack of confidence in treatment options for those subgroups 
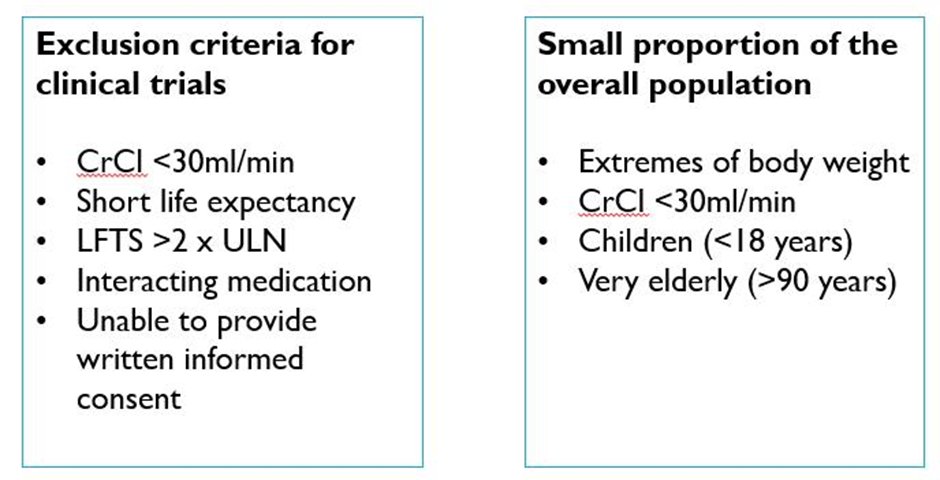
7) Body weight is needed to dose #LMWH and influences #warfarin dosing. Does the ‘one size fits all’ approach of #DOACs still apply to extreme patient subgroups? 
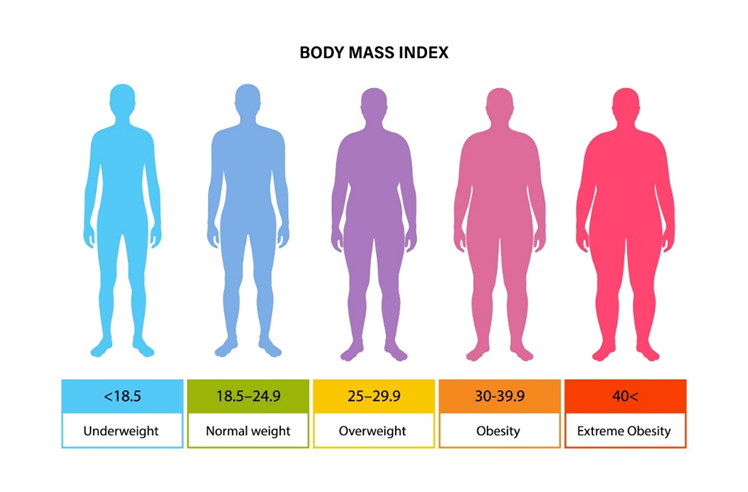
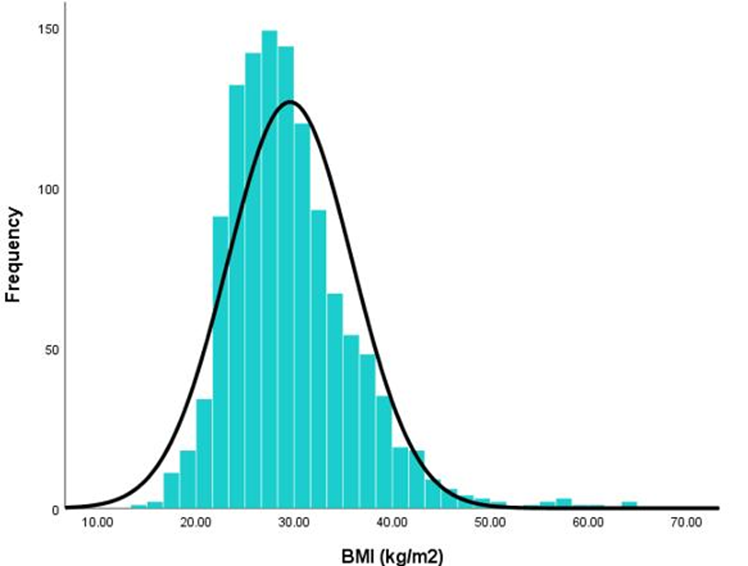
8) Worldwide obesity is on the rise & is a risk factor for VTE. According to the WHO, it has nearly tripled since 1975. We are more likely to see obese patients in the thrombosis clinic as seen in the BMI histogram from the FIRST registry of 🇬🇧 VTE cases. 
9) Let’s look at a case: 55♂️ with proximal DVT post-hip arthroscopy. PMH: HTN. BW 130 kg and Creatinine 150 umol/L (1.7mg/dL); CrCl 90 ml/min (or 75 ml/min using adjusted BW). How would we treat this man? 

10) What does the guidance say? The @ASH_hematology 2020 VTE treatment guidelines suggest: home treatment over hospital, DOACs over VKA (without a particular DOAC preference), for 3-6 months, & suggest against routine use of compression stockings.
🔓doi.org/10.1182/blooda…
🔓doi.org/10.1182/blooda…
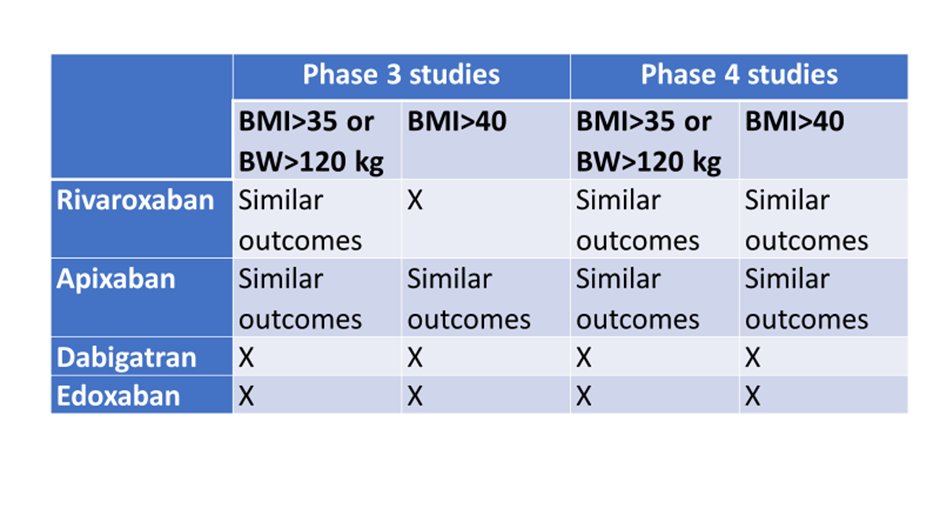
11) The @isth SSC guidelines (2016) suggested not using DOACs in patients w/extreme obesity (BMI>40 kg/m2 or BW >120 kg) & if DOACs were to be used, to perform peak and trough drug levels. However new evidence is now available on DOAC use in obesity.
🔓doi.org/10.1111/jth.13…
🔓doi.org/10.1111/jth.13…
12) Rivaroxaban is the best studied DOAC in obesity. Post-hoc analysis of VTE pts with BMI >35 in EINSTEIN showed no sig diff in recurrent VTE/major bleeding bet rivaroxaban & warfarin. Several observational studies also show no difference in outcomes.🔓pubmed.ncbi.nlm.nih.gov/27535349/
13) Apixaban can also be used in obesity. Post-hoc analysis of VTE pts weighing >120 kg or w/BMI >40 in AMPLIFY showed similar recurrent VTE/VTE-related deaths & less major bleeding than w/warfarin. Observational studies➡️similar results. 🔓pubmed.ncbi.nlm.nih.gov/33890242/
14) Here is the summary of efficacy and safety outcomes in VTE treatment clinical studies comparing DOACs with VKA in obese patients. (Modified from 🔓onlinelibrary.wiley.com/doi/full/10.11…) 
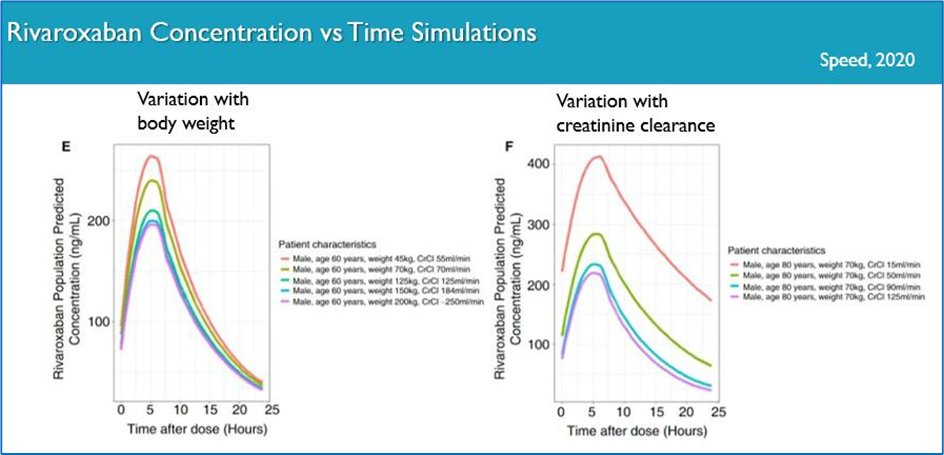
15) What do pharmacokinetic (PK) data say? A population PK model➡️ #CrCl & not BW was the most significant covariate affecting rivaroxaban exposure. Reduced exposure to apixaban has been noted in obesity but this is likely not clinically significant. 🔓onlinelibrary.wiley.com/doi/10.1111/jt… 
16) Let’s return to our patient with proximal DVT. He weighs 130 kg and has a busy job as an investment banker. What would you treat him with?
17) Please select your treatment of choice and return TOMORROW for more on this case and more education! Tip o' the hat to @rpharms @howe0001 @RZarychanski @ReenaM2703 @Denise11252734 @PriyaSriRajah @nicolai_leo @BritSocHaemThro @CapriniJoseph @SemThrombHemost @NNMN1 @KCHPharmacy
18) Welcome back!! @AryaRoopen is leading us through a first-rate program on managing #VTE at extremes of weight & in the face of⬇️#renal function. You are earning CE/#CME 🇺🇸🇪🇺🇨🇦🇬🇧. Please follow us for more #accredited #tweetorials!
19) Now as to yesterday's closing❓(scroll back to tweet 16 and answer if you haven't done so, before looking⤵️! Well, multiple answers could have been correct.
20) Correct answers include rivaroxaban apixaban & warfarin. The 2021 @isth SSC guideline for #VTE pts w/BMI >40 or BW>120 kg recommends standard doses rivaroxaban or apixaban. Dabigatran or edoxaban are advised against due to lack of supporting data.
🔓onlinelibrary.wiley.com/doi/full/10.11…
🔓onlinelibrary.wiley.com/doi/full/10.11…
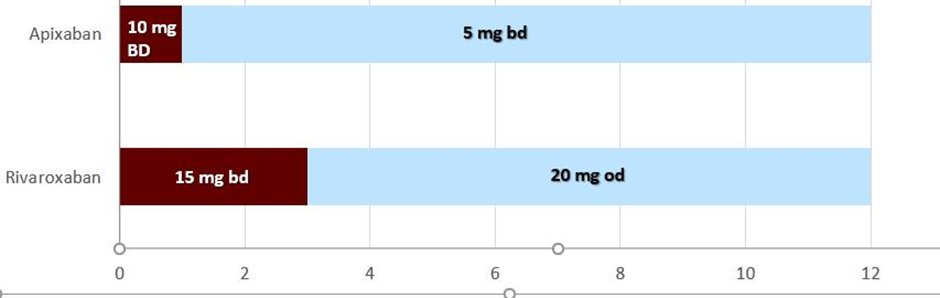
21) The patient had a provoked proximal DVT, he was treated with #apixaban 10 mg bd for 1 week then 5 mg bd for total of 6 months. He was treated as an outpatient, compression stockings were not prescribed and he was encouraged to remain active. He had a good clinical outcome.
22a) Previous guidance suggested monitoring DOAC levels in obesity. Therapeutic targets are not known & there is insufficient evidence to make clinical decisions or dose adjustments based on DOAC levels. The 2021 @isth guidance suggest against routine monitoring in this setting.
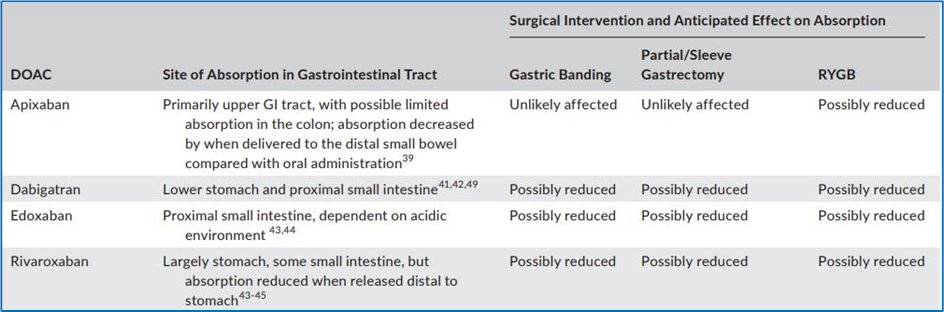
23) An interesting situation might arise if an obese patient on DOAC requires bariatric surgery, which might alter bioavailability. Data are scant and limited to small PK studies with little outcome information. 
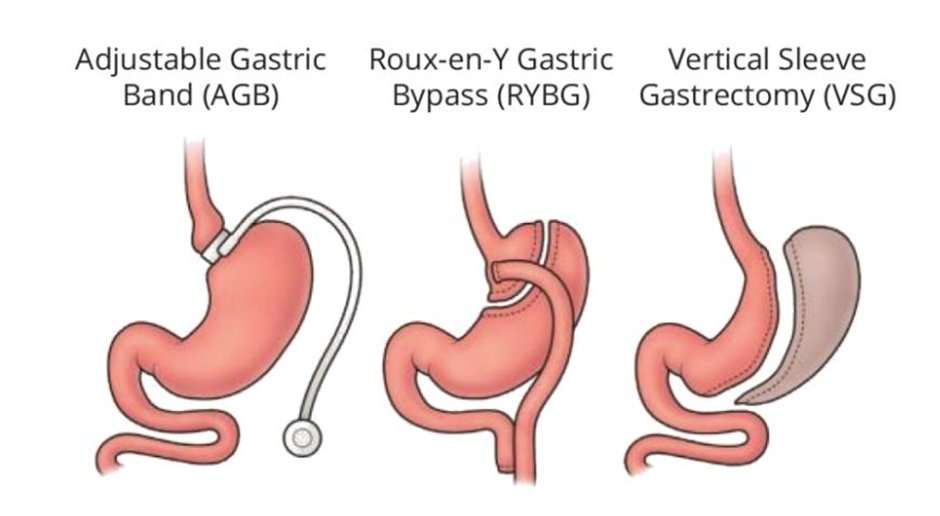
24) Because of the uncertainty re absorption & inter-individual variability @isth suggests🚫DOAC in the acute setting after bariatric surgery but to use parenteral anticoagulation with the possibility of switch to VKA or DOAC later, with monitoring.
🔓onlinelibrary.wiley.com/doi/full/10.11…
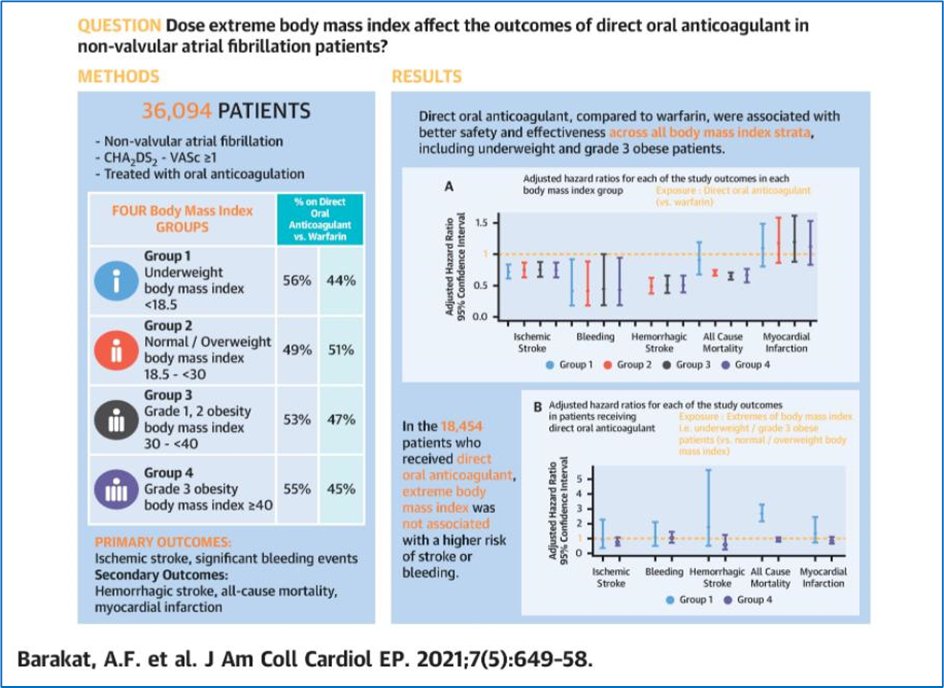
🔓onlinelibrary.wiley.com/doi/full/10.11…
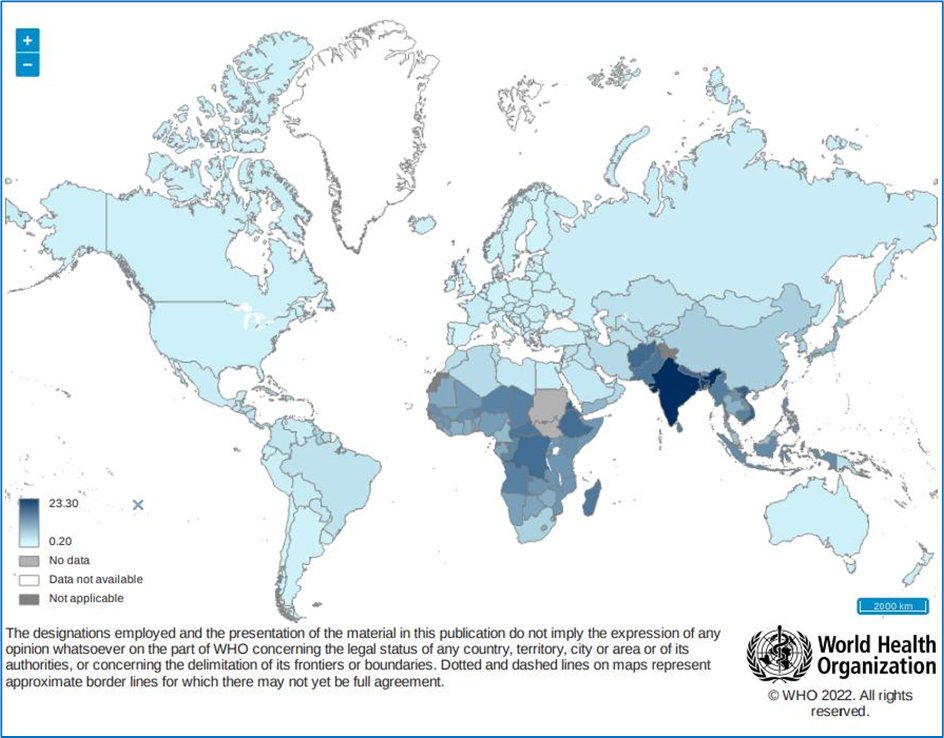
25a) It is increasingly common to see underweight patients that need treating for VTE. Prevalence of underweight among adults varies from 2% to 23% globally (WHO). Underweight patients might have other morbidities and have worse outcomes in hospital settings and higher mortality.
25b) See 🔓who.int/data/gho/data/… 
26) There is little evidence to inform dosing DOACs in underweight cases. SPCs for DOACs & VTE treatment guidelines do not help. Over-anticoagulation & bleeding risk are an obvious concern. With DOAC monotherapy this risk might be highest in the initial treatment period. 
27) Another case: 78♀️ dc'd home post prolonged stay w/pneumonia. Readmitted 10d later w/#PE. BW 48 kg, Creat 60, #CrCl 52 ml/min. Low body fat, finds SC injections painful. She lives alone & would struggle to attend hospital for blood tests. What would you treat her with?
28) Guidance? Data from dabigatran studies are scant. Rivaroxaban EINSTEIN data only included 2% underweight patients; outcomes not separately evaluated. Peak plasma riva levels are higher in underweight patients but clinical significance is uncertain. 🔓onlinelibrary.wiley.com/doi/10.1111/jt… 
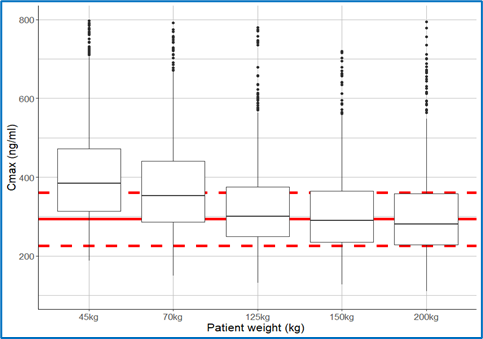
29) Apixaban AMPLIFY included 9% patients <60 kg, data not powered for outcome differences. PK study in underweight patients showed higher peaks but similar troughs. In normal BW population, apixaban safety data superior but unavailable in underweight. 🔓pubmed.ncbi.nlm.nih.gov/33890242/
30) The Edoxaban phase 3 VTE trial recruited 13% patients <60 kg, who received half dose of edoxaban. Separate outcome data are not available so no conclusion can be reached. In contrast, safety & efficacy of weight-based dosing for #LMWH is well established.
31) Outcome data for underweight VTE patients on DOACs are sparse but the existing data for #AFib patients across the extremes of body weight are reassuring with respect to safety & efficacy.
jacc.org/doi/abs/10.101…
jacc.org/doi/abs/10.101…
32) Coming back to the case, there is no single right answer. All options are valid: warfarin, standard dose rivaroxaban or apixaban, half dose edoxaban. The loading period of higher intensity anticoagulation with rivaroxaban or apixaban might be a concern.
33) Her low body fat means a prolonged period of injections is not desirable and the convenience factor with warfarin is low. With edoxaban the recommended reduction in dose below 60 kg might be an advantage as bleeding risk is potentially reduced.
34) My preference (@AryaRoopen) then would be for 5 days of LMWH followed by half dose edoxaban (30 mg od). Since this is a provoked event 3-6 months of anticoagulation would suffice.
Please RETURN TOMORROW to wrap up this program and grab your FREE CE/#CME!
Please RETURN TOMORROW to wrap up this program and grab your FREE CE/#CME!
35) Welcome back. You are just a few🖱️clicks away from FREE CE/#CME, but first @AryaRoopen will discuss #VTE management in patients with #KidneyDisease. It's another special population in the #anticoagulation🌍. 👋to @cpgale3 @SMithoowani @NHutchJones @TinaDuttDr @mmamas1973 
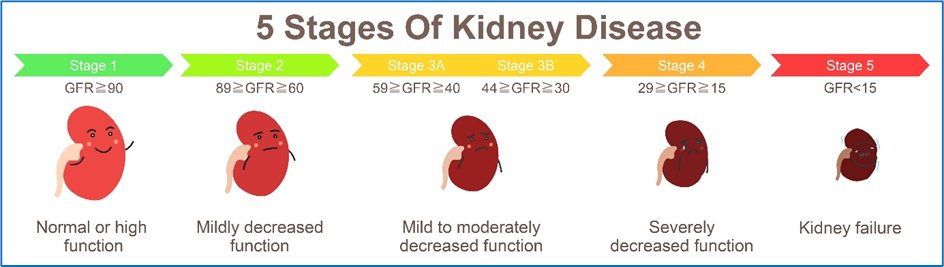
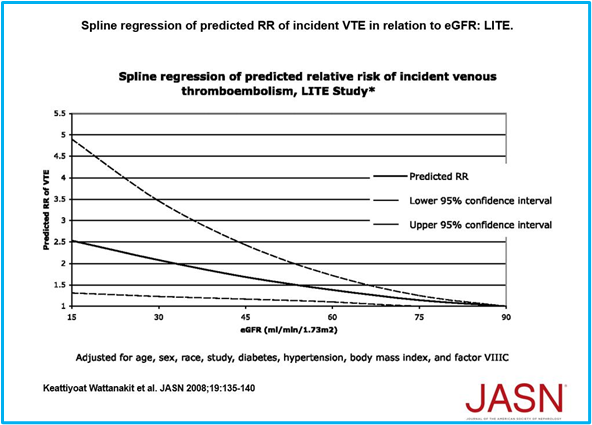
36) #CKD is a global health concern, affecting 11-13%, the majority stage 3.
CKD is associated with an increased risk of cardiovascular disease including VTE.
See jasn.asnjournals.org/content/19/1/1… and also more #accredited #tweetorials from @ckd_ce!
CKD is associated with an increased risk of cardiovascular disease including VTE.
See jasn.asnjournals.org/content/19/1/1… and also more #accredited #tweetorials from @ckd_ce!
37) Case 3⃣: 58♂️ diagnosed with unprovoked #PE after presenting to # ED with shortness of breath & chest pain. CTPA = PE. PMH: T2DM HTN CKD Stage 3b. Creatinine 223 (2.52), BW 90 kg. Accountant, known to be nonadherent with long term meds.
What would you treat him with?
What would you treat him with?
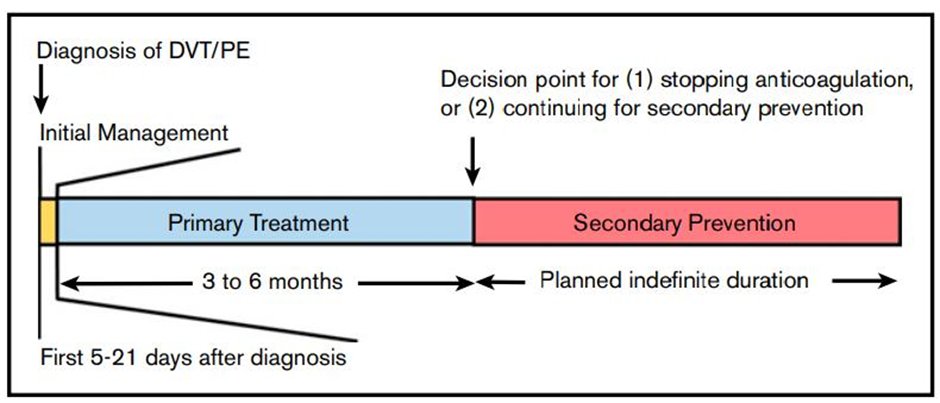
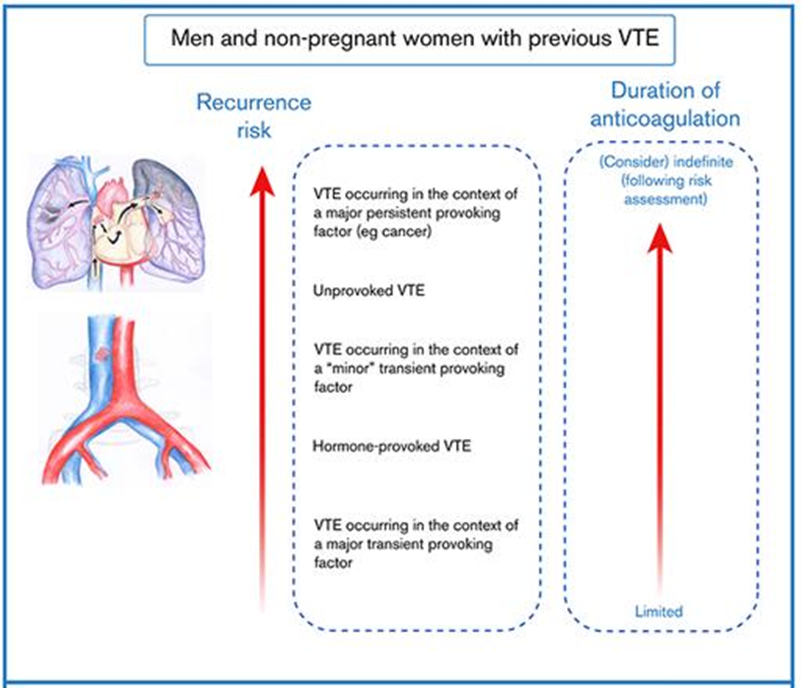
38) He would need initial anticoagulation 3-6mo & then a decision about continuing for secondary prevention. The unprovoked nature of his VTE, taken with his gender (& CKD) would put him at his risk of recurrence were he to stop anticoagulation.
🔓doi.org/10.1182/hemato…
🔓doi.org/10.1182/hemato…
39) This patient has #CKD but how does this influence #DOAC choice? 4 DOACs, 4 diff elimination pathways. All have one mechanism in common: renal clearance but to varying extents. Just remember: apixaban ¼ , rivaroxaban ⅓, edoxaban ½, & dabigatran ⅘!🔓academic.oup.com/europace/artic… 
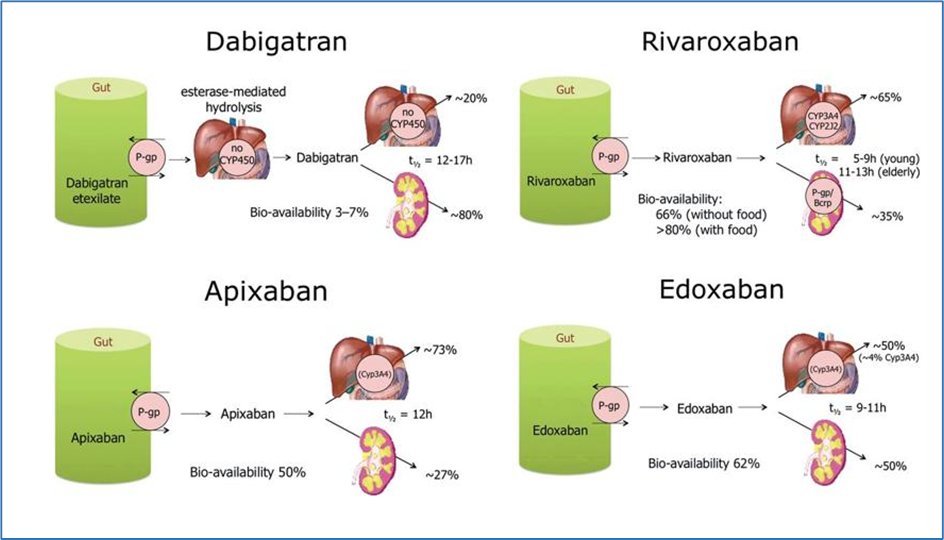
40) 🚨CHECK YOUR DOSE: RIVAROXABAN & APIXABAN prescribing guidelines are DIFFERENT for VTE & AF. Take CARE not to underdose, esp for patients with renal impairment: e.g. AF rivaroxaban dose⬇️to 15mg OD if CrCl <50ml/min but standard VTE maintenance dose is 20mg OD.
41) You are ready to calculate renal function, but which method should you use for the DOACs? The alternatives are:
a. eGFR-MDRD ➡️GFR = 32 mL/min/1.73 m²
b. eGFR-CKD-EPI ➡️ GFR = 29 ml/min/1.73 m²
c. Cockcroft-Gault ➡️CrCl = 41 ml/min
a. eGFR-MDRD ➡️GFR = 32 mL/min/1.73 m²
b. eGFR-CKD-EPI ➡️ GFR = 29 ml/min/1.73 m²
c. Cockcroft-Gault ➡️CrCl = 41 ml/min

42) All of the #DOAC Ph 3 studies calculated creatinine clearance using Cockcroft-Gault & dosing algorithms are based on these thresholds. So, although Cockcroft-Gault has its flaws it is the method of choice for DOACs.
mdcalc.com/creatinine-cle…, so for our pt, CrCl = 41 ml/min
mdcalc.com/creatinine-cle…, so for our pt, CrCl = 41 ml/min
43) And there is more! In patients with low BW, eGFR may overestimate renal clearance, especially in elderly patients with low body weight/BMI.
🔓bmjopen.bmj.com/content/3/9/e0…
Example: 75♀️, 50kg Creat 100umol/L (1.13 mg/dL). Cockcroft-Gault➡️34ml/min; EGFR–CKD-EPI ➡️51ml/min
🔓bmjopen.bmj.com/content/3/9/e0…
Example: 75♀️, 50kg Creat 100umol/L (1.13 mg/dL). Cockcroft-Gault➡️34ml/min; EGFR–CKD-EPI ➡️51ml/min
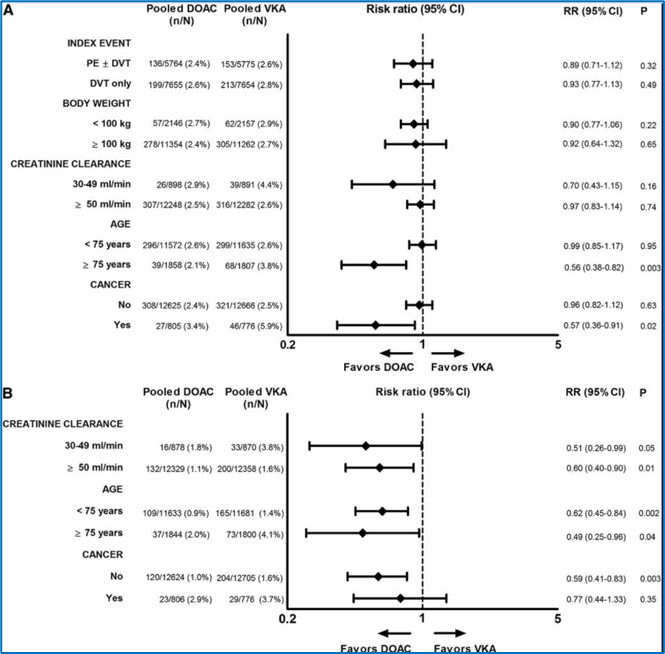
44) From phase 3 data are DOACs or warfarin more effective in moderate renal impairment? Meta analysis (A) says: non-inferior. In patients with moderate renal impairment is a DOAC safer than warfarin? Meta analysis (B) says: yes - less major bleeding 🔓ashpublications.org/blood/article/… 
45) Coming back to our patient. He could have any of: Apixaban 10mg BD for 7 days then 5mg BD (NOTE NO DOSE REDUCTIONS SPC recommends risk benefit assessment), Rivaroxaban 15mg BD 3/52 then 20mg OD, Edoxaban 30 MG OD after 5 day LMWH (reduced dose edoxaban as CrCL is <50ml/min).
46) I wouldn’t choose dabigatran in view of high proportion renal clearance. All the Xa inhibitors would be reasonable options for our patient. If adherence is an issue some might prefer once daily dosing but then OD vs BD and implications for adherence is another debate!
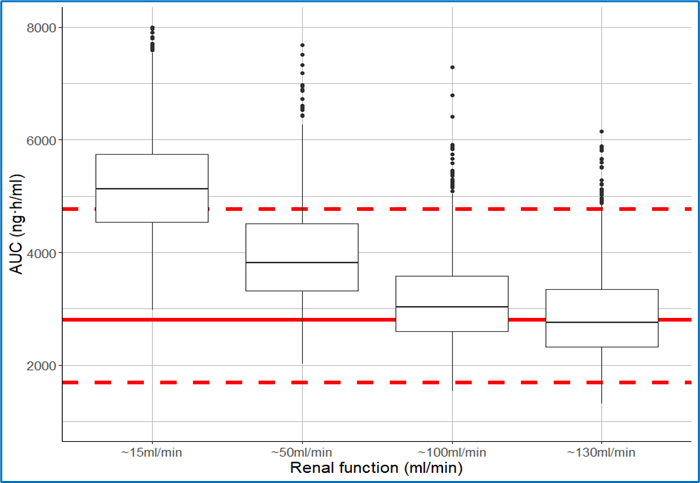
47) Population PK simulation studies illustrate the impact of CrCL on overall rivaroxaban exposure (area under the curve (AUC)). Renal function must be checked as AKI or a progressive decline in renal function may lead to accumulation for our patient. 🔓onlinelibrary.wiley.com/doi/full/10.11… 
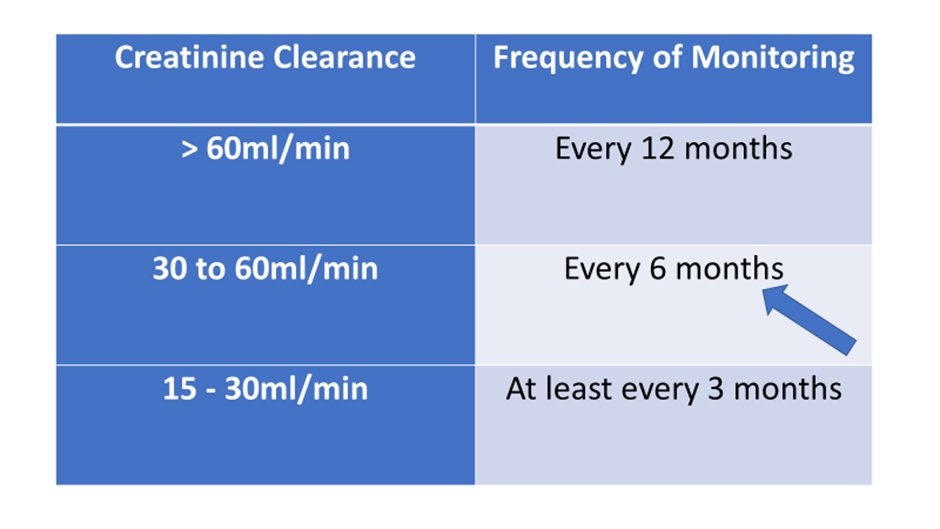
48) Assessment of renal function must be made at initiation and as part of ongoing review. Frequency of monitoring depends on CrCL, for our patient every 6 months! 
49) So that brings us to the end of this tweetorial on treating VTE at extremes of body weight & renal function. I hope you have found it interesting & useful! I am @AryaRoopen. Go grab your 0.5hr CE/#CME credit right now at cardiometabolic-ce.com/antithrombotic….
FOLLOW US for more programs!
FOLLOW US for more programs!
• • •
Missing some Tweet in this thread? You can try to
force a refresh