1) Welcome to a new #accredited #tweetorial on Cardiorenal Disease in T2D & the Impact of Blocking the MR in Patients w/DKD, another CE/#CME program by one of the @GoggleDocs, this time our friend @AmarPut, Diabetes & Endocrine Consultant in the West Midlands 🇬🇧. #CaReMe #FOAMed 

2) This program is supported by an educational grant from Bayer & is intended for #healthcare providers. Author disclosures can be found at ckd-ce.com/disclosures/. Prior programs, still available for CE/#CME credit, are at ckd-ce.com. CE/#CME credit 🇬🇧🇪🇺🇨🇦🇺🇸
3) So first – the ‘triple threat’ . . . We know of the link between the 🫀 and the kidneys and the ‘#cardiorenal’ syndrome, but what about in the setting of #diabetes?
4) Diabetes is a well known independent risk factor for #cardiovascular and #renal disease with recent #CVOTs highlighting this link.
5) Given the newer data we have especially from trials such as #EMPEROR reduced and preserved, &#CREDENCE, #DAPA CKD/HF, there appears to be relevance to looking at this dual pathology in the setting of type 2 diabetes management…
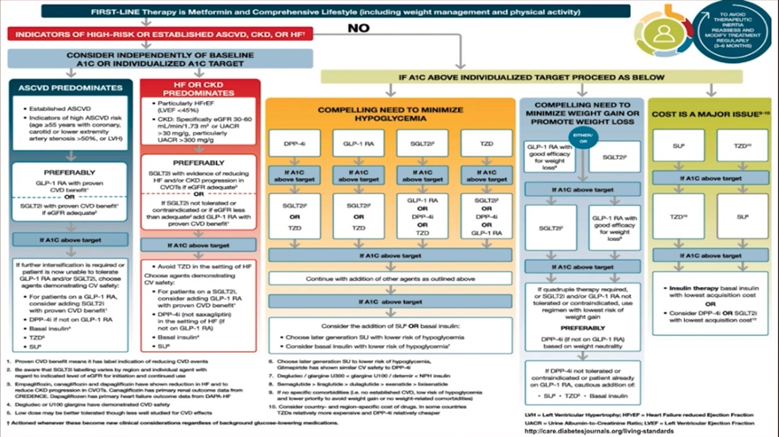
6) ADA/EASD @AmDiabetesAssn / @EASDelearning and many other #Guidelines mention the importance of #riskreduction for #CVD and renal separately in DM but do not mention a ‘cardiorenal’ entity separately in management 
7) Perhaps this and multimorbidity might be something to explore in future guidance 🤔…but that is for another time!
A question: Approximately what percentage of patients in the 🇺🇸with #T2DM have #CKD?
A question: Approximately what percentage of patients in the 🇺🇸with #T2DM have #CKD?
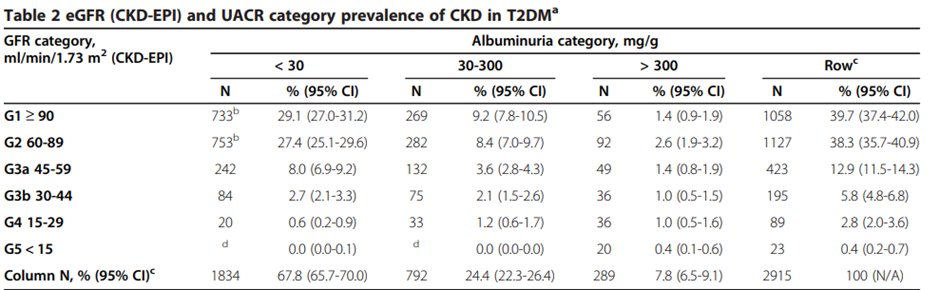
8) Data from the 🇬🇧and the 🇺🇸show that about 20% - 40% of patients with diabetes develop #CKD. (US data below, from 🔓pubmed.ncbi.nlm.nih.gov/24990184/) 
10) Cardiovascular disease (#CVD) is a leading cause of morbidity and mortality in T2DM. It has an overall prevalence of 32.2%, and is responsible for about 50% deaths globally. See 🔓pubmed.ncbi.nlm.nih.gov/29884191/ 
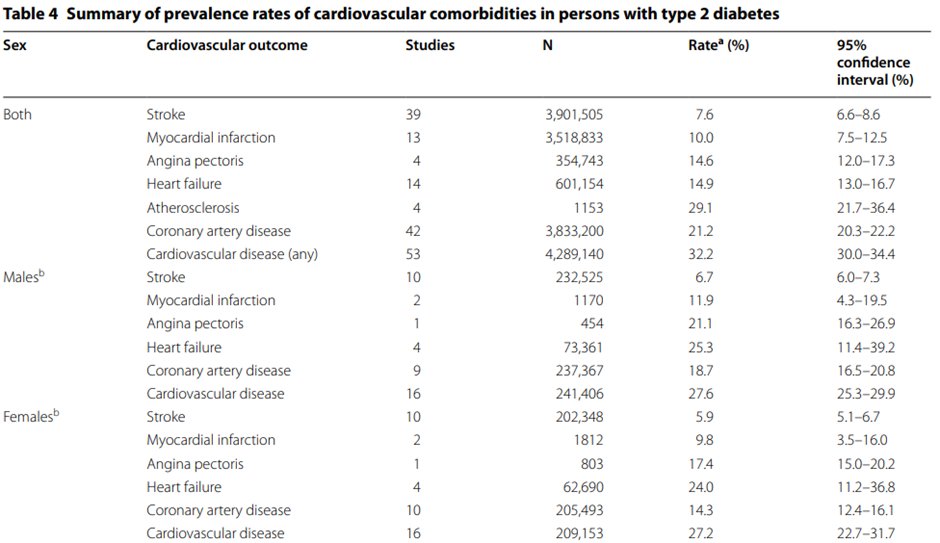
11) CVD risk in a person w/diabetes is ⬆️by the presence of #CKD & #uACR excretion has been associated with ⬆️CV risk.
It has also been suggested that endothelial dysfunction in diabetes may ➡️development and progression of renal and cardiac pathologies.
It has also been suggested that endothelial dysfunction in diabetes may ➡️development and progression of renal and cardiac pathologies.
12) This appears to cause intractable changes in volume regulation, sodium homeostasis, inflammation, & metabolism that lead to cardiorenal disease and mortality. 🔓frontiersin.org/articles/10.33…
13) But what about the combined comorbidity?
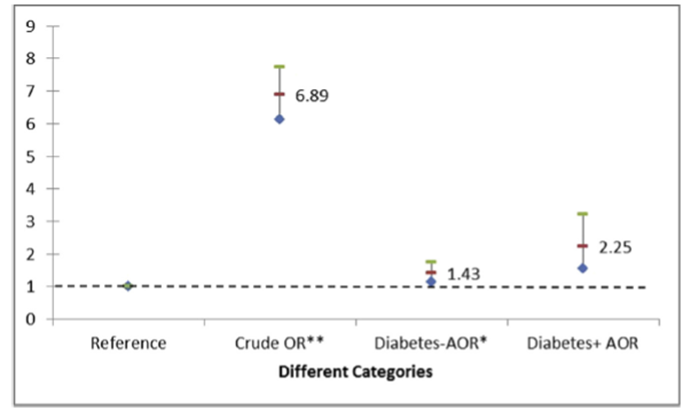
This study (🔓pubmed.ncbi.nlm.nih.gov/28089648/) looked at the prevalence of CKD in pts w/diabetes with (& without) CVD, noting the higher likelihood of CKD in the presence of CVD (with a strong prevalence of type 2 cardiorenal syndrome).
This study (🔓pubmed.ncbi.nlm.nih.gov/28089648/) looked at the prevalence of CKD in pts w/diabetes with (& without) CVD, noting the higher likelihood of CKD in the presence of CVD (with a strong prevalence of type 2 cardiorenal syndrome).
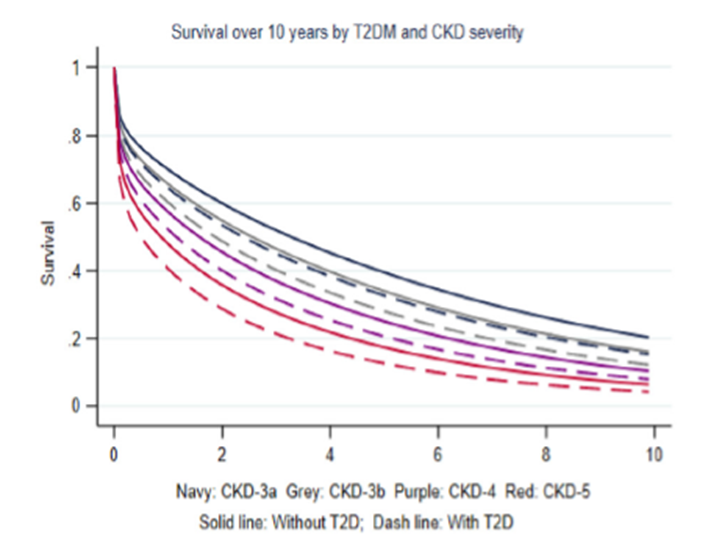
14) In a cohort of people with new onset #HF, hospitalisation and mortality was higher in patients with T2D or CKD, and worst in those with both comorbidities. See 🔓thelancet.com/journals/eclin…
@kamleshkhunti @profmjdavies @scelee1 @LDC_tweets
@kamleshkhunti @profmjdavies @scelee1 @LDC_tweets
15) But what about presence of #T2DM in pts w/#cardiorenal syndrome? Read on…
In a study of pts admitted with cardiorenal syndrome, those w/CRS had a higher prevalence (2/3rds patients) of diabetes, mostly T2DM, & high 1-yr mortality. 🔓pubmed.ncbi.nlm.nih.gov/32912147/
In a study of pts admitted with cardiorenal syndrome, those w/CRS had a higher prevalence (2/3rds patients) of diabetes, mostly T2DM, & high 1-yr mortality. 🔓pubmed.ncbi.nlm.nih.gov/32912147/
16) Though we focus on #T2DM, there have been data also looking at those with #T1DM…
So… is the risk of #cardiorenal disease at younger ages higher in those with type 1 or type 2 DM?
So… is the risk of #cardiorenal disease at younger ages higher in those with type 1 or type 2 DM?
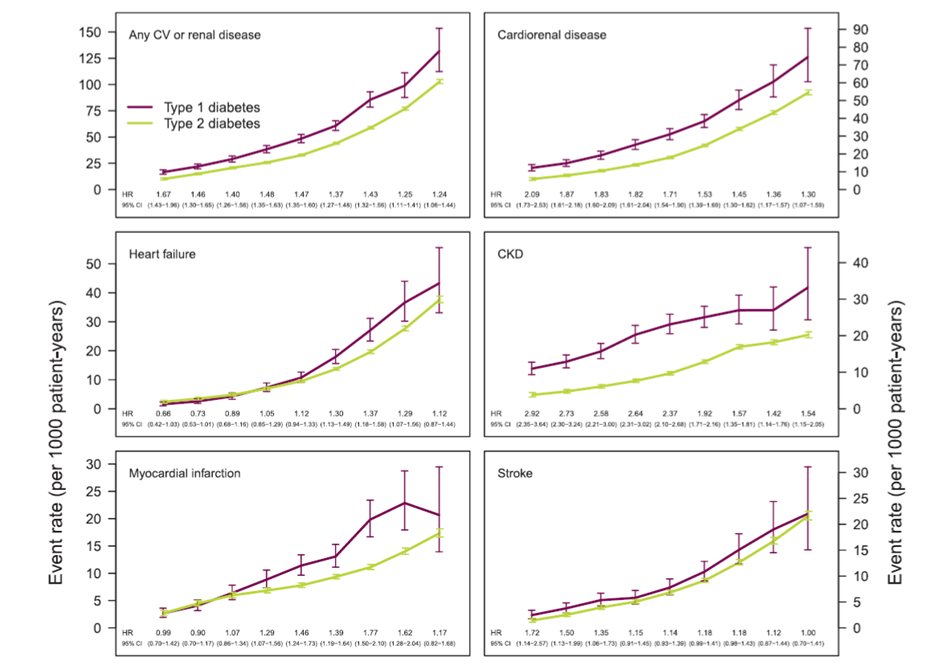
17) Adult patients with T1D vs T2D had an overall greater risk of cardiorenal disease (#HF and #CKD) across all ages, MI and all-cause death at middle-older ages, and stroke at younger ages. Sobering! 
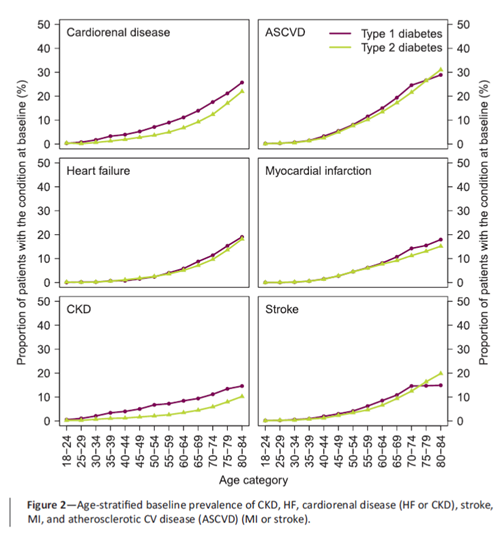
18) Total age-adjusted #CVRD burden & risks were greater among those with #T1D compared with #T2D (🔓pubmed.ncbi.nlm.nih.gov/33653822/) 
19) This suggests that there is indeed a role for assessment for cardiorenal disease in those with T2D of course individually, but actually as combined co-morbidities to aid management of this triple threat!
And what of the management…
And what of the management…
20) Slightly beyond the scope of this tweetorial but a few tantalizing considerations…
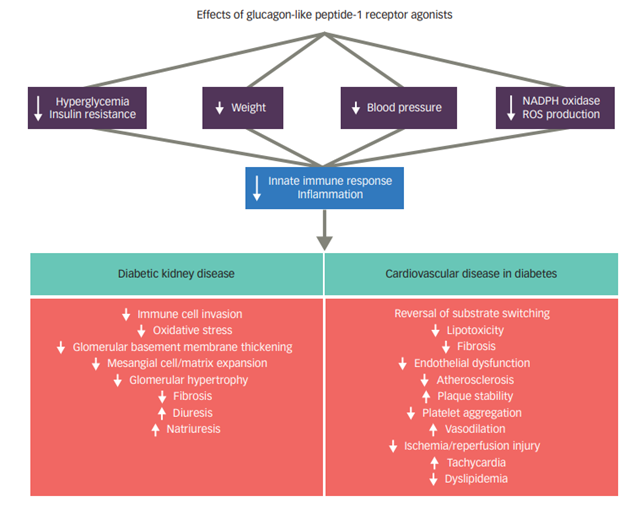
Looking at the mechanisms of #GLP-1 RAs we could see how they might be beneficial in those with #cardiorenal disease … (🔓doi.org/10.17925/USE.2…)
Looking at the mechanisms of #GLP-1 RAs we could see how they might be beneficial in those with #cardiorenal disease … (🔓doi.org/10.17925/USE.2…)
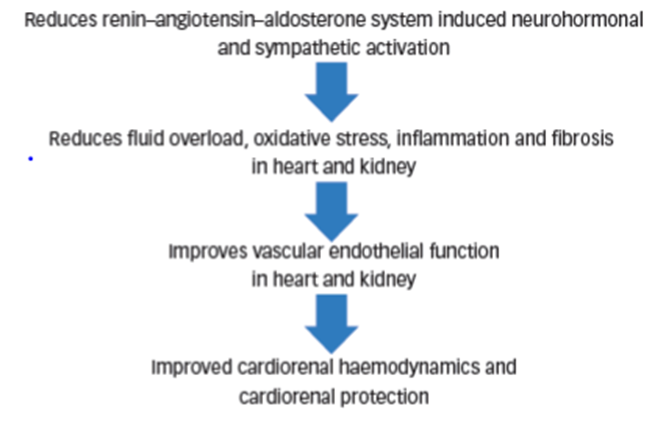
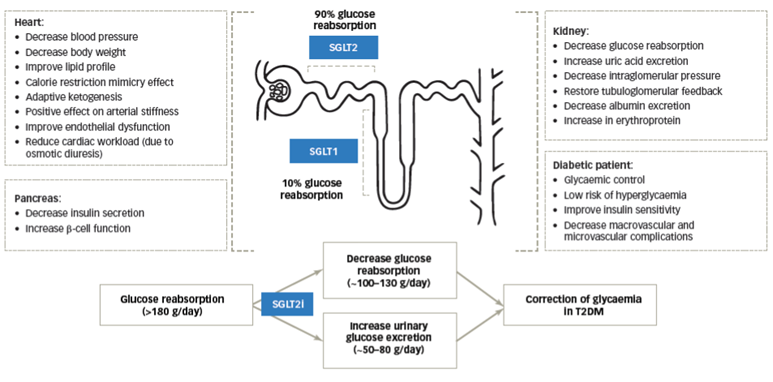
21) But it's in the #SGLT2i area where we get stronger support for use in CRS…
(🔓pubmed.ncbi.nlm.nih.gov/33117442/)
(and 👏@Sglt2inhibitorL @GoggleDocs @RpratleyMD @AliceYYCheng @drricardocorrea @edgarvlermamd @nephondemand )
(🔓pubmed.ncbi.nlm.nih.gov/33117442/)
(and 👏@Sglt2inhibitorL @GoggleDocs @RpratleyMD @AliceYYCheng @drricardocorrea @edgarvlermamd @nephondemand )
24) Interesting thoughts and considerations, it remains to be seen if this is likely to occur clinically…what do you think? Comment below . . . and return TOMORROW for more education on #cardiorenal syndrome and #diabetes!
25) Welcome back! You're on a @GoggleDocs-led tour of #cardiorenal syndrome and #DKD. We'll be talking about #MRAs too as YOU earn🆓CE/#CME: 0.75h credit for #physicians #physicianassociates #nurses #NPs #pharmacists 🇺🇸🇬🇧🇨🇦🇪🇺!
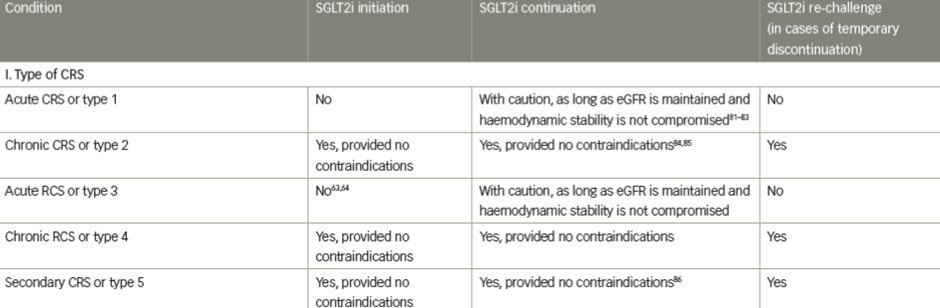
26) So we left off yesterday (scroll ⤴️) talking about the potential role for #SGTL2i in the management of #CRS with #diabetes.
Now…something that definitely is in practice…#mineralocorticoid antagonism in #DKD!
Now…something that definitely is in practice…#mineralocorticoid antagonism in #DKD!
27) We are intentionally not covering finerenone as this has been well covered by fellow @GoggleDocs member @drkevinfernando (earn credit still at ckd-ce.com/mra1/).
But . . .
But . . .
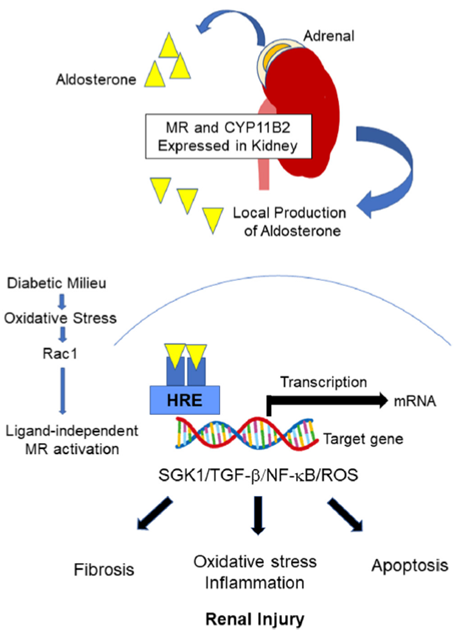
28) It's important to know that in #DKD, overactivation of #MR has been implicated as a driver of inflammation and fibrosis.
Local activation of #RAAS has been shown to contribute to DKD (see 🔓frontiersin.org/articles/10.33…)
Local activation of #RAAS has been shown to contribute to DKD (see 🔓frontiersin.org/articles/10.33…)
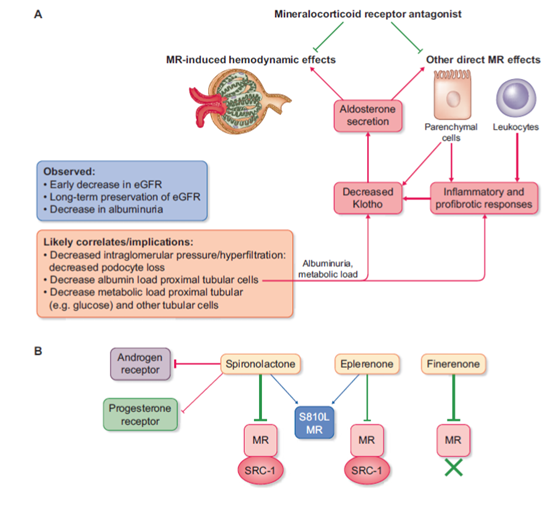
29) #MRAs have been suggested as an option in DKD management through potential mechanistic reasons (🔓academic.oup.com/ndt/advance-ar… and accompanying 🆓📽️highlights at academic.oup.com/ndt/pages/auth… ) 
30) And as per our friends at @goKDIGO, ACE/ARBs have long been and remain the staple medication of CKD/DKD management 
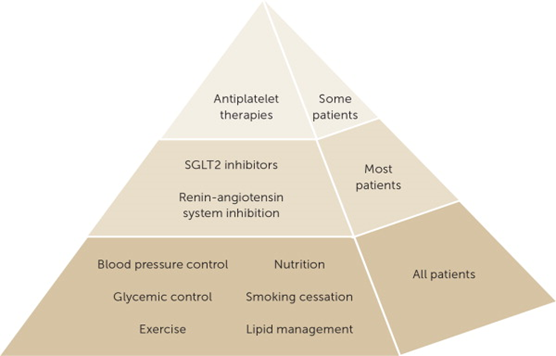
31) However, long-term administration of ACE/ARBs paradoxically⬆️aldosterone levels (aldosterone breakthrough) - thereby suggesting MRAs may be of benefit…but this increases the risk of hyperkalaemia (and yes you can earn MORE🆓credit on hyperK mgt at cardiometabolic-ce.com/category/hyper…)…
32) Studies of medications in addition to ACE/ARBs have also highlighted this with the well-known #ALTITUDE study looking at #aliskrein as add on to ACEi/ARB stopped early with the risk of hyperkalaemia notable (🔓nejm.org/doi/full/10.10…) 
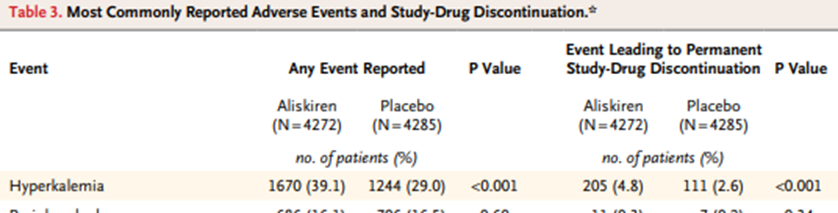
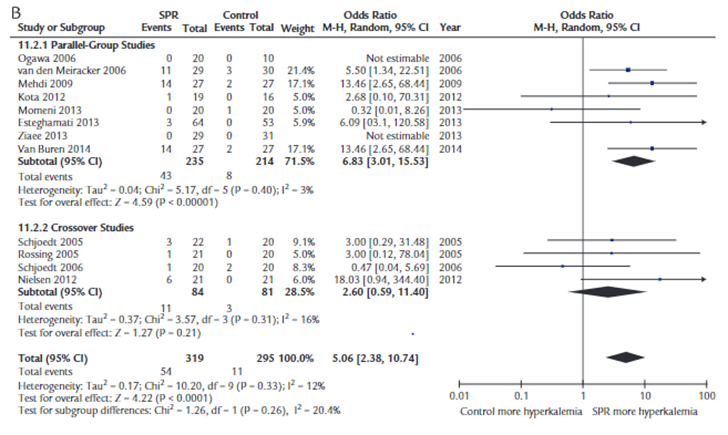
33) ... though a 2015 paper (🔓pubmed.ncbi.nlm.nih.gov/25220494/) reviewing studies with a total over 500 patients suggests that overall it may not be that high…🤔 
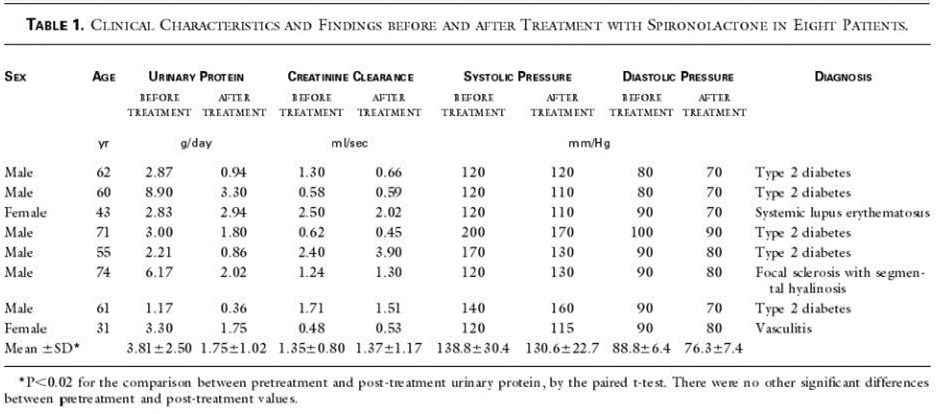
34) Since #spironolactone has the longest history of all the MRAs, MRA-in-DKD studies were performed with it. 1st report of proteinuria⬇️from spironolactone as an add-on therapy to a RAS inhibitor in patients with CKD (5 of 8 had DKD) was in 2001 (nejm.org/doi/10.1056/NE…): 
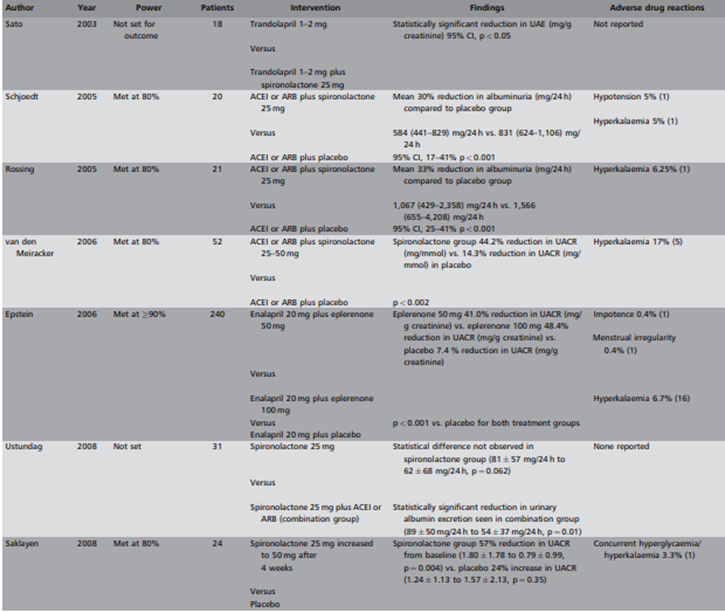
35) The first small, double-blinded, controlled, 2-period crossover study was performed by K. Rossing et al, 🔓doi.org/10.2337/diacar….
36) 21 patients w/T2DM on RAASi were treated w/spironolactone 25mg or placebo x 8wks ➡️ significant ⬇️ in albuminuria (& BP)….with minimal hyperkalaemia in this case…however…
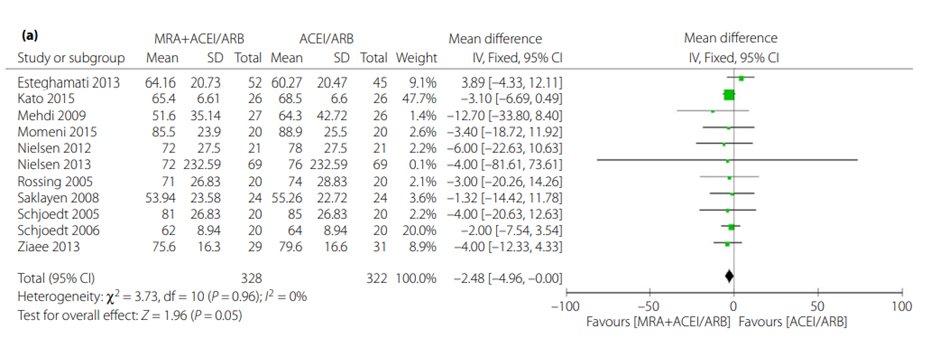
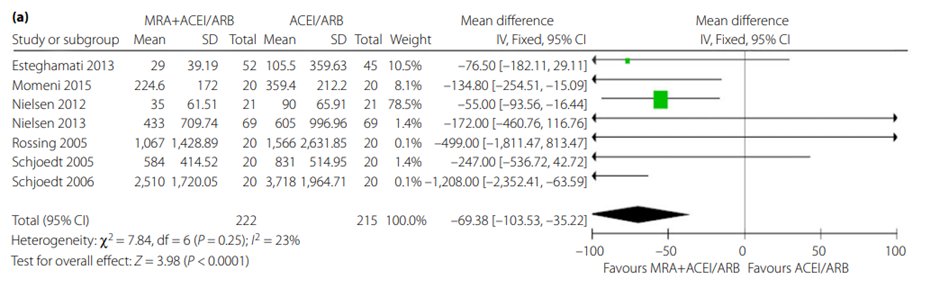
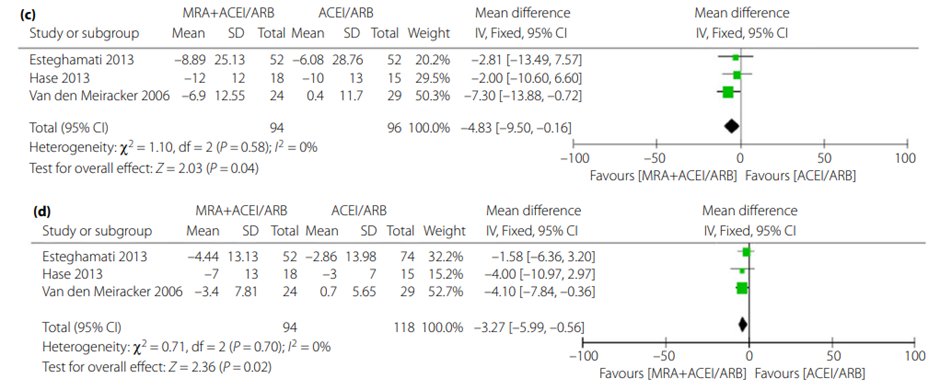
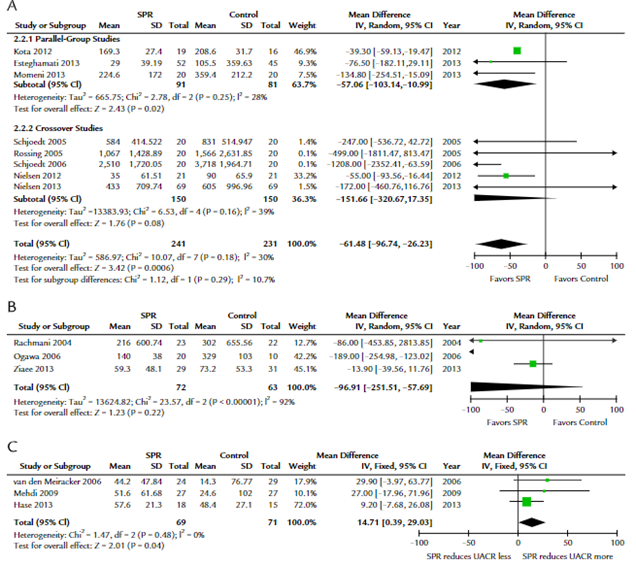
This metanalysis of spironolactone shows reductions in uACR with no significant change in eGFR…
This metanalysis of spironolactone shows reductions in uACR with no significant change in eGFR…
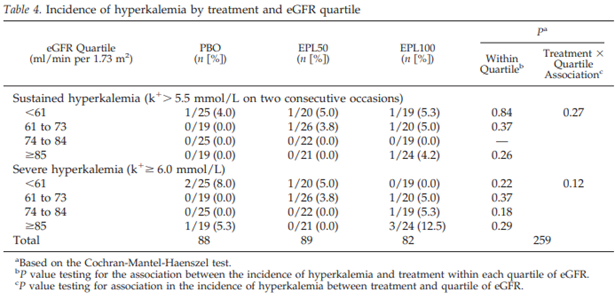
38) What about the other well known (second-generation) steroidal MRA…#eplerenone?
39) Alas, not much data here, but we do have… 🔓cjasn.asnjournals.org/content/1/5/940: 268 pts w/T2D+albuminuria (UACR 50 mg/g), open-label run-in with enalapril 20 mg OD then.. 12wk tx w/eplerenone 50 mg v 100 mg v placebo.
Notable changes in uACR with less eGFR decline were promising


Notable changes in uACR with less eGFR decline were promising



41) ... though one study is not strong enough to reassure, with the the risk of hyperkalaemia still a caution. accessdata.fda.gov/drugsatfda_doc…
42) So TOMORROW we'll look at the whole field of #MRAs in general . . . AND provide your super secret (not really) link to your🆓CE/#CME, all delivered RIGHT HERE on Twitter and @ckd_ce! Be sure to COME BACK!
@HecmagsMD @ChristosArgyrop @nephondemand @edgarvlermamd @kdpsinghlab
@HecmagsMD @ChristosArgyrop @nephondemand @edgarvlermamd @kdpsinghlab
43) WELCOME BACK! You are some great @GoggleDocs-led learning and just a few🖱️clicks away from FREE CE/#CME! We're wrapping up this discussion of #cardiorenal disease, #DKD, and #MRAs.
@drpatrickholmes @HannahBeba @dguerrot @RpratleyMD @AgarwalRajivMD @MasriAhmadMD @cpcannon
@drpatrickholmes @HannahBeba @dguerrot @RpratleyMD @AgarwalRajivMD @MasriAhmadMD @cpcannon
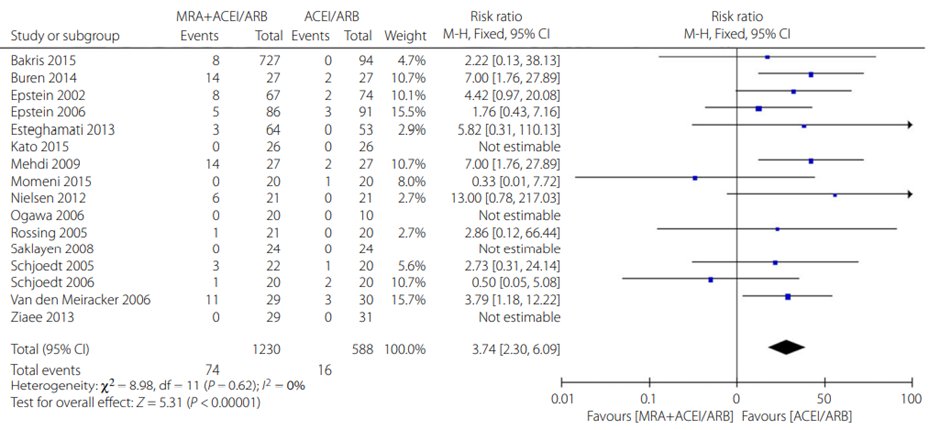
44) Let’s broaden the field to look at MRAs in general… this analysis of MRAs also noted benefits seen with individual therapies: 🔓onlinelibrary.wiley.com/doi/10.1111/jd…
49) Coming full circle🔄…what about MRAs in pts w/cardiorenal disease in the setting of #diabetes?
The answer: Use of Mineralocorticoid Receptor Antagonists in Patients With Heart Failure and Comorbid Diabetes Mellitus or Chronic Kidney Disease 🔓ahajournals.org/doi/10.1161/JA…

The answer: Use of Mineralocorticoid Receptor Antagonists in Patients With Heart Failure and Comorbid Diabetes Mellitus or Chronic Kidney Disease 🔓ahajournals.org/doi/10.1161/JA…
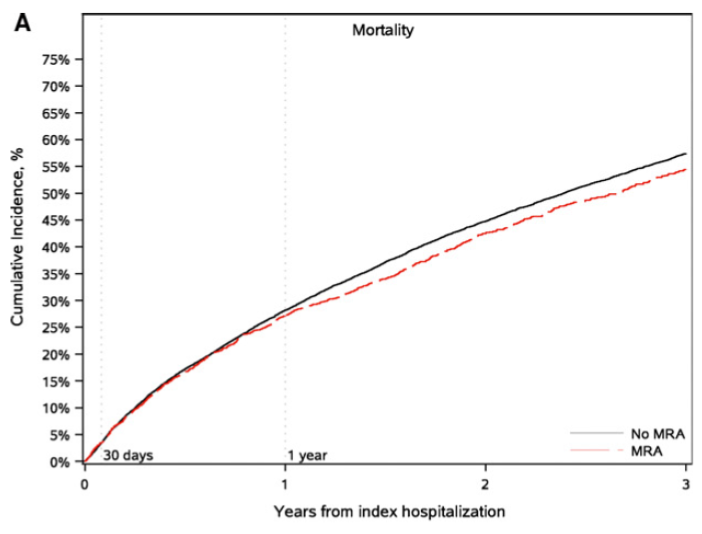

50) Again, potential benefit in mortality reduction but notable increase in hospitalization for #hyperkalaemia!
MRAs have a role in DKD in⬇️albuminuria. Hard outcomes such as kidney disease progression, cardiovascular events and mortality data are not so clear for earlier MRAs
MRAs have a role in DKD in⬇️albuminuria. Hard outcomes such as kidney disease progression, cardiovascular events and mortality data are not so clear for earlier MRAs
51) However, the use of steroidal MRA in #DKD has been limited by its side effects, especially hyperkalemia.
52) Use in this setting would require diet review, ACE inhibitor/ARB use monitoring, possible potassium binder use, regular serum potassium and renal function monitoring….maybe highlighting where a non-steroidal MRA may have its benefits…😊
53) So what do you think? What is the main concern with use of MRAs in those with diabetes?
54) Bet you got it right. Diabetes or not, hyperkaelemia if your biggest concern with #MRA therapy! Don't miss the opportunity for more education and CE/#CME credit on management of #hyperkalemia at cardiometabolic-ce.com/category/hyper…
55) And there you have it! Congratulations on completing your epic journey through #cardiorenal disease to MRAs in #DKD! Go forth & claim your 0.75h credit 🇬🇧🇨🇦🇪🇺🇺🇸at ckd-ce.com/mra3/! This is your friendly twitterhood GoggleDoc signing off! FOLLOW US for more education!
• • •
Missing some Tweet in this thread? You can try to
force a refresh