@IndependentSage 🇬🇧 #covid #longcovid #NHS crisis
@DrGuddiSingh @DrRachelWardGP @mattinadakim @ProfEmer @Dr_D_Robertson @SusanMichie @globalhlthtwit @BinitaKane @Daltmann10 @SGriffin_Lab @sheencr @HelenRSalisbury @DeenanDpillay @martinmckee @Kit_Yates_Maths @ArisKatzourakis
1
@DrGuddiSingh @DrRachelWardGP @mattinadakim @ProfEmer @Dr_D_Robertson @SusanMichie @globalhlthtwit @BinitaKane @Daltmann10 @SGriffin_Lab @sheencr @HelenRSalisbury @DeenanDpillay @martinmckee @Kit_Yates_Maths @ArisKatzourakis
1
https://twitter.com/independentsage/status/1530164358998740992
@DrGuddiSingh #covid
devastating impact on #NHS after years of underfunding & staff shortages: long waits for emergency services, operations postponed, delayed cancer treatment & difficult to secure doctor & dentist appointments.
Why & how can we help?
2/
devastating impact on #NHS after years of underfunding & staff shortages: long waits for emergency services, operations postponed, delayed cancer treatment & difficult to secure doctor & dentist appointments.
Why & how can we help?
2/
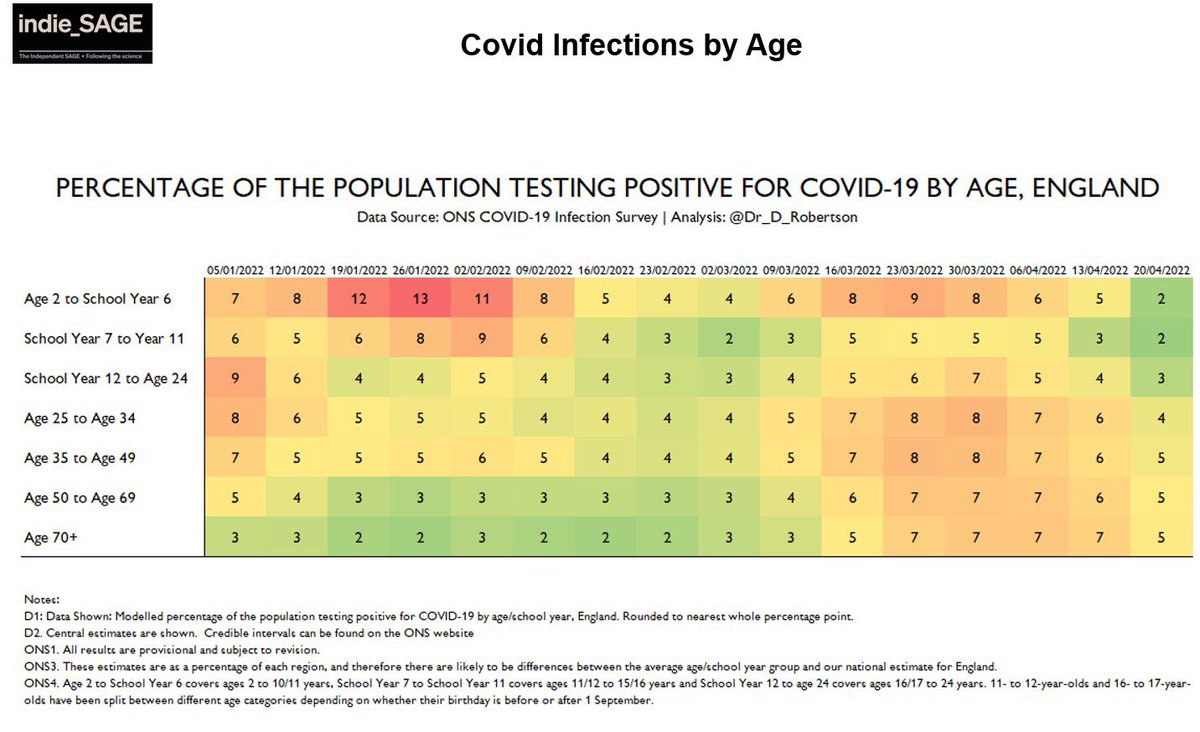
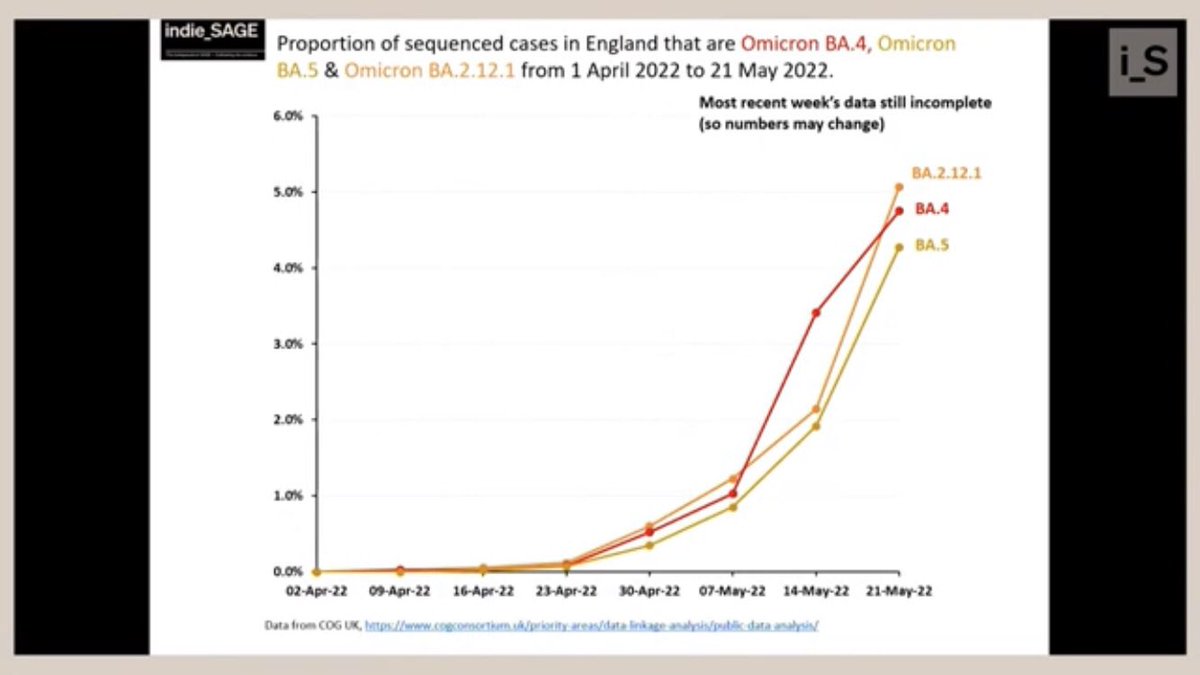
@Dr_D_Robertson sparse data now; dashboard only England 🏴
First thing to watch as it impacts our future is growth of variants:
Three increase fast in 🇬🇧
each at 4-5% of sequenced samples —> watch this space to see what will happen in the weeks & months ahead…
3/
First thing to watch as it impacts our future is growth of variants:
Three increase fast in 🇬🇧
each at 4-5% of sequenced samples —> watch this space to see what will happen in the weeks & months ahead…
3/
@ONS
— cases fall yet still 1 in 50-60 infected. Scotland 🏴 potentially rising but uncertain
—> situation where cases are falling, new variants increasing
so in a plateau period (for all age groups) waiting to see what will happen in the weeks ahead…
4/

— cases fall yet still 1 in 50-60 infected. Scotland 🏴 potentially rising but uncertain
—> situation where cases are falling, new variants increasing
so in a plateau period (for all age groups) waiting to see what will happen in the weeks ahead…
4/


#NHS National Health System
1) *Staff sickness significant*, highest in patient-facing groups, to #covid respiratory & infectious disease as protections lift regardless (note - latest data is until Jan)
5/

1) *Staff sickness significant*, highest in patient-facing groups, to #covid respiratory & infectious disease as protections lift regardless (note - latest data is until Jan)
5/


2) Hospital admissions — primarily for #covid relatively small but still significant
3) 🚑 wait times for several types of patients eg signs of stroke show significant delays
+ after admission, wait times longest in a decade:
28% wait more than 4 hours, 5% more than 12
6/


3) 🚑 wait times for several types of patients eg signs of stroke show significant delays
+ after admission, wait times longest in a decade:
28% wait more than 4 hours, 5% more than 12
6/



4) Waiting to start non-emergency treatment
- 1 in 9 waiting to start is significant & increased in March
- 38% waiting over 16 weeks greatly misses the target
- 4.8% waiting longer than a year is high after low figures pre #covid
7/



- 1 in 9 waiting to start is significant & increased in March
- 38% waiting over 16 weeks greatly misses the target
- 4.8% waiting longer than a year is high after low figures pre #covid
7/




#NHS 💬
@HelenRSalisbury
- 3 guests from frontline help understand #covid impact
- huge task treating acute & #longcovid which also sickens staff —> shortages
- infection controls profoundly alters way we work
- build capacity of systems in community, hospitals, social care
@HelenRSalisbury
- 3 guests from frontline help understand #covid impact
- huge task treating acute & #longcovid which also sickens staff —> shortages
- infection controls profoundly alters way we work
- build capacity of systems in community, hospitals, social care
@mattinadakim
- #covid disrupting prevention has hidden cost —> now see later more severe presentations coupled with the desire for elective care with a background of increasing emergency activity, a perfect storm
—> to survive next 5-10 years need sea change in integrated care



- #covid disrupting prevention has hidden cost —> now see later more severe presentations coupled with the desire for elective care with a background of increasing emergency activity, a perfect storm
—> to survive next 5-10 years need sea change in integrated care




@BinitaKane perfect storm resonates. Staff really hit too —> lost a large number to death, chronic illness, burnout & stress & workload went up. For years consultants cancelled routine care to enter front line —> cumulative effect just peaks now.
- @mattinadakim better systems:
- @mattinadakim better systems:

#covid swamps generalists:
@DrRachelWardGP
- for 17k patients max 500 calls daily. Now >1000 like seeing each 20 times/year instead of 2-3
- England 🏴 GPs see 46 people/day, safe level 25
—> patient safety concern in a background of a reducing workforce, losing GPs every month



@DrRachelWardGP
- for 17k patients max 500 calls daily. Now >1000 like seeing each 20 times/year instead of 2-3
- England 🏴 GPs see 46 people/day, safe level 25
—> patient safety concern in a background of a reducing workforce, losing GPs every month




—> staff exodus at all levels to stress, makes health service even more difficult
⚠️
1600 missing general doctors in the country —> Rebuild GP campaign
Negative press on lack of face contact significantly impacts morale
1 in 4 GPs knows a colleague who ended their own life

⚠️
1600 missing general doctors in the country —> Rebuild GP campaign
Negative press on lack of face contact significantly impacts morale
1 in 4 GPs knows a colleague who ended their own life


@ProfEmer #covid massive staff impact
- more deaths than the greatest previous disaster, as many staff as workers died; for every death 100 people injured
- #longcovid 3-4% workforce incl bad prognosis like strokes, a million lost working days/year
- 30-50% ill health & burnout



- more deaths than the greatest previous disaster, as many staff as workers died; for every death 100 people injured
- #longcovid 3-4% workforce incl bad prognosis like strokes, a million lost working days/year
- 30-50% ill health & burnout




@ProfEmer shocking ~50% of staff not at full capacity
⚠️ must move away from government discourse only deaths/ICU overload matters —> must *prevent* covid from spreading, harming & mutating with unknown long term costs
16/


⚠️ must move away from government discourse only deaths/ICU overload matters —> must *prevent* covid from spreading, harming & mutating with unknown long term costs
16/


@DrGuddiSingh thanks guests for quite shocking testimony
- worrying statistics then first hand accounts of known & hidden costs of #covid & #longcovid responsible for a million lost days/year, history of neglect leads to doctors being swamped now; needs fundamental rethink
17
- worrying statistics then first hand accounts of known & hidden costs of #covid & #longcovid responsible for a million lost days/year, history of neglect leads to doctors being swamped now; needs fundamental rethink
17
(more to come below)
From audience:
- nursing perspective, unions campaign to keep NHS public & for treasury to properly fund enough staffing, sufficient pay to live in expensive cities. Get key people together —> we need some kind of leadership in terms of a workforce strategy
@DrRachelWardGP:
18
- nursing perspective, unions campaign to keep NHS public & for treasury to properly fund enough staffing, sufficient pay to live in expensive cities. Get key people together —> we need some kind of leadership in terms of a workforce strategy
@DrRachelWardGP:
18

- @HelenRSalisbury gov disbanded SAGE as thinks it’s all over but isn’t —> continue losing staff if we don’t act to stop #covid & #longcovid & resource the NHS
- @mattinadakim get what we pay for 🇬🇧 GDP per capita spending is lowest in developed world, affects all services
19

- @mattinadakim get what we pay for 🇬🇧 GDP per capita spending is lowest in developed world, affects all services
19


@martinmckee put in international context:
- 🇬🇧 higher winter mortality & the most deprived areas in W Europe, labour supply issues
—> improve work practices & make investment case for health: higher economic growth, productivity, more secure & safer societies
20

- 🇬🇧 higher winter mortality & the most deprived areas in W Europe, labour supply issues
—> improve work practices & make investment case for health: higher economic growth, productivity, more secure & safer societies
20


Question: how much is current crisis used to hide further privatization of the #NHS either directly or by creating the situation where privatization will be offered as the only solution to ‘save’ it?
@globalhlthtwit worries this would increase costs, reduce access & service
22


@globalhlthtwit worries this would increase costs, reduce access & service
22



@martinmckee thinks any privatisation likely ‘by default’
—> people discouraged by long wait times approaching private care than the NHS being sold off wholesale, hospitals & all
@HelenRSalisbury @DrGuddiSingh — service really fell since 10 years ago, patients leave — shocking


—> people discouraged by long wait times approaching private care than the NHS being sold off wholesale, hospitals & all
@HelenRSalisbury @DrGuddiSingh — service really fell since 10 years ago, patients leave — shocking



Question: the root cause of many NHS problems is the collapse of social care so why is government reluctant to make a substantial intervention here?
@SusanMichie politics & values —> as citizens we should speak up about this political question, demand better service
24
@SusanMichie politics & values —> as citizens we should speak up about this political question, demand better service
24

Question: @DeenanDpillay can integrated care systems help?
@DrRachelWardGP theory is great but practice can be too heavy & crush local initiative
@mattinadakim opportunity to improve care, smooth relations between silos — necessary to meet coming demands
25


@DrRachelWardGP theory is great but practice can be too heavy & crush local initiative
@mattinadakim opportunity to improve care, smooth relations between silos — necessary to meet coming demands
25



@BinitaKane
it’s really important as well to not forget other social determinants of health like where they are born, poverty, good housing, education; have an addiction.
NHS on its own can’t solve all of that, without a wider focus on prevention.
26
it’s really important as well to not forget other social determinants of health like where they are born, poverty, good housing, education; have an addiction.
NHS on its own can’t solve all of that, without a wider focus on prevention.
26
Question: @SGriffin_Lab government proposes to shorten waiting times & get to patients more quickly by dropping #covid restrictions, separation of patients, personal protective equipment (PPE). What do you think of this as a long term solution?
@ProfEmer crazy — risks chaos
27
@ProfEmer crazy — risks chaos
27
@ProfEmer
#NHS should primarily be about stopping disease in the first place. Not mixing everyone in one huge caldron of survival of the fittest
—> If we put this virus through all this mess it will survive it & come back to bite us. And if not this one, it will be another

#NHS should primarily be about stopping disease in the first place. Not mixing everyone in one huge caldron of survival of the fittest
—> If we put this virus through all this mess it will survive it & come back to bite us. And if not this one, it will be another


@ProfEmer
⚠️ engaging in a simplistic zero sum game without understanding the implications of what happens when you drop the control of the source, the pathway & the reception —> the dynamics will turn everything upside down & we could end up at square one like snakes & ladders
⚠️ engaging in a simplistic zero sum game without understanding the implications of what happens when you drop the control of the source, the pathway & the reception —> the dynamics will turn everything upside down & we could end up at square one like snakes & ladders

@mattinadakim extend to everyone —> respect means masking/isolating when ill.
Countries with respectful cultures do better against #covid
30
Countries with respectful cultures do better against #covid
30
(General Q&A to follow below)
Question: will the current pandemic make people more susceptible to other viral infections? Have our immune systems been made weaker or is reduced contact responsible for this?
@Daltmann10 @sheencr lockdown etc only marginal effects but #longcovid can alter immunity in some :


@Daltmann10 @sheencr lockdown etc only marginal effects but #longcovid can alter immunity in some :



@globalhlthtwit measles can depress immunity for nine months
@Daltmann10 like HIV or Epstein Barr —> complex immunology
@sheencr can temporarily damage some tissues’ immune response too
32

@Daltmann10 like HIV or Epstein Barr —> complex immunology
@sheencr can temporarily damage some tissues’ immune response too
32


Question: new studies show vaccination protects less from #longcovid than expected. What implications?
Can vaccines be tweaked to make them more effective or is the only option not to catch #covid in the first place?
33
Can vaccines be tweaked to make them more effective or is the only option not to catch #covid in the first place?
33
@Daltmann10
#Longcovid so much more ghastly than we thought, even in the face of triple vaccination & so-called milder Omicron, gave 380k new cases.
We need the best possible future defenses against covid & long covid and they go hand in hand, we’re still in a very tough place
#Longcovid so much more ghastly than we thought, even in the face of triple vaccination & so-called milder Omicron, gave 380k new cases.
We need the best possible future defenses against covid & long covid and they go hand in hand, we’re still in a very tough place

@SGriffin_Lab
⚠️ as we don’t know the cause of #longcovid we don’t know if vaccines can prevent it. Recent studies seem to show very little protection.
Best is to suppress #covid & use vaccine plus strategy, not vaccines alone.
⚠️ as we don’t know the cause of #longcovid we don’t know if vaccines can prevent it. Recent studies seem to show very little protection.
Best is to suppress #covid & use vaccine plus strategy, not vaccines alone.

Question: as mitigations are abandoned, those who deem them necessary are openly criticized. How do you navigate this?
@SusanMichie some people are averse to social norms, find it hard to mask —> be clear WHY you’re doing it helps to be a role model to protect self & others


@SusanMichie some people are averse to social norms, find it hard to mask —> be clear WHY you’re doing it helps to be a role model to protect self & others



@SGriffin_Lab shifting blame from authorities to individual choice is unlike any other public health issue: driving, smoking, environment contaminations…
⚠️ yet still #longcovid high prevalence & new variants coming…
+ unfair as excludes the vulnerable from ‘freedom day’

⚠️ yet still #longcovid high prevalence & new variants coming…
+ unfair as excludes the vulnerable from ‘freedom day’


@BinitaKane daughters wear FFP2 in class out of choice as educated on the risks —> stood up to someone questioning why wearing despite vaccine, says as they don’t protect from #covid
38/38
38/38

@dgurdasani1 @chrischirp @Zubhaque @ReicherStephen @trishgreenhalgh
@longcovidwork @LongCovidSOS @LCKNIreland @LCKScotland @LongCovidKids @LongCovidCH
#independentsage
@longcovidwork @LongCovidSOS @LCKNIreland @LCKScotland @LongCovidKids @LongCovidCH
#independentsage
To add — @dgurdasani1 warns of high hospital acquired infection already & urgency to stem this to protect patients & staff — #covid can complicate other diseases, contributing to admissions even where it’s not the primary cause.
NHS bed capacity is already under strain
NHS bed capacity is already under strain
https://twitter.com/katiakerswell/status/1525513032734060544
Note — protections reduce other deadly diseases circulating & new ones arising faster in our warming world (incl microbe resistance):
Hospitals should be careful especially when already under strain & full of vulnerable patients & staff
https://twitter.com/susanmichie/status/1529347432659800065?s=21&t=Hv6U0MwxTV-o5kp1ZwvvPg
Hospitals should be careful especially when already under strain & full of vulnerable patients & staff
https://twitter.com/katiakerswell/status/1498678424768069635
Several recent studies show vaccines don’t prevent #longcovid & post acute sequelae as much as we’d hoped
— new variants ‘breakthrough’ more easily
1/2
— new variants ‘breakthrough’ more easily
1/2
https://twitter.com/katiakerswell/status/1523655869996859392
2/2 #Longcovid risk even if vaccinated:
@chrischirp :
@dgurdasani1 :
Several studies in this 🧵
@LongCovidCH @longcovidwork @LongCovidKids @LongCovidSOS @LongCOVIDEurope
@chrischirp :
https://twitter.com/chrischirp/status/1529483703055011841?s=21&t=Hv6U0MwxTV-o5kp1ZwvvPg
@dgurdasani1 :
https://twitter.com/dgurdasani1/status/1529565397040742400?s=21&t=Hv6U0MwxTV-o5kp1ZwvvPg
Several studies in this 🧵
@LongCovidCH @longcovidwork @LongCovidKids @LongCovidSOS @LongCOVIDEurope
https://twitter.com/lauramiers/status/1529516407058219008
@ShaunLintern @NHSEngland @NHSMillion @NHSuk @NHSEnglandLDN @NHSuk @NHSConfed @NHS_HealthEdEng see this IndependentSage 🧵 on challenges to the NHS
(Note — see in thread number 27 replies as it continues the discussion on the importance of continuing protections in hospitals)
Note — return to thread 33 replies to see the rest of it
• • •
Missing some Tweet in this thread? You can try to
force a refresh