
1) Welcome to our new #accredited #tweetorial which is Part 2 of a 2-part "highlights" program on new #SGLT2i & #DKD data presented at @ERAkidney #ERA22. #Physicians #nurses #pharmacists #PAs and #NPs can all earn 0.5h CE/#CME by following this 🧵!
2a) @ERAkidney #ERA22 is a primary international scientific symposium for interaction and exchange among basic scientists and clinicians working in #Nephrology. Our expert author is Dr. Clara García Carro (@ClaraGCarro) from San Carlos Clinical Hospital (Madrid, Spain). 

2b) Be sure to check out the first half of this #ERA22 recap from my colleague @shbermejo, and get MORE 🆓CE/#CME at ckd-ce.com/dkd12_ERA22a/. Join me in following @ckd_ce for the BEST in #cardiorenal education delivered entirely by #tweetorial!
3) This program is #accredited for CE/#CME & is supported by an independent educational grant from the Boehringer Ingelheim/Lilly Alliance. It is not intended for US- or UK-based based HCPs. Accreditation statement & faculty disclosures at ckd-ce.com/disclosures/.
4) Let's start with some interesting data and novelties for our #flozinators! Are you ready?
5) As you know, #canagliflozin was associated, in the #CANVAS program, to a higher risk of lower-extremity #amputation, so ... are #SGLT2i as effective in terms of #CV #morbidity and #mortality in patients with #CKD and #PVD as in CKD patients without PVD?
6) Adeera Levin 🇨🇦 answered this question at #ERA22! She presented a post hoc analysis with data from #CANVAS and #CREDENCE trials with the aim to investigate the effects of canagliflozin on CV and kidney outcomes in CKD patients with and without PVD.
7) 3514 patients with #CKD and without #PVD and 1156 had CKD + PVD were submitted to propensity-score matched #canagliflozin and placebo to balance differences between groups.
8) After matching, #canagliflozin was associated with a ⬇️risk of #MACE, #HHF/CV death, doubling serum creatinine, #ESKD, and the composite of ESKD or dSCr compared with placebo in patients with CKD with and without PVD.
9) Beneficial effects of #canagliflozin on CV and kidney outcomes are consistent and can be seen in patients regardless of these comorbidities. 

10a) Let’s continue with #flozinators! Are #SGLT2i effective and safe in kidney transplant recipients? @ClaraGCarro (myself!) presented data about the larger multicenter retrospective study investigating if SGLT2i are safe and well tolerated in #kidneytransplant recipients
10b) Here is the Nephrology team from Clinico San Carlos Hospital that produced this work on #SGLT2i and #kidneytransplant recipients! 

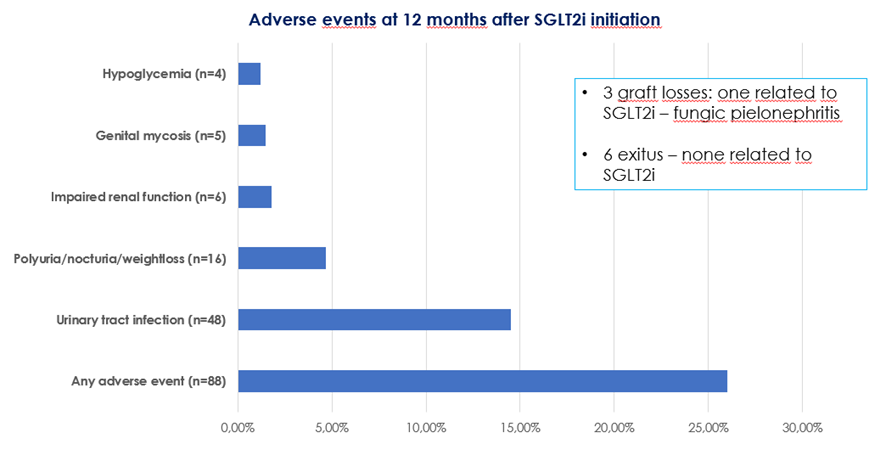
11) Data from 339 KT recipients receiving #SGLT2i with #T2D or post-transplant DM were analyzed. We found a significant reduction in body weight, a better blood pressure and glycemic control, and a reduction in #proteinuria at 6 months after SGLT2i.
12) We also saw ⬇️ uric acid & cholesterol levels, & ⬆️ magnesium levels. 48 patients presented #UTI at 12 months and only one lost the graft. Incidence of UTI was higher in patients with previous episodes. There were no other major adverse events. 




13) More #flozination data at #ERA22 came from by Prof Kanbay 🇹🇷. Osmotic nephrosis, an emerging cause of #SGLT2i-related AKI was reviewed: it is generally associated with hyperosmotic agents, severe hyperglycemia & glycosuria. Mild to severe AKI appears days after drug exposure.
14) The hypothesis is that the renal injury is due to #pinocytosis with uptake into lysosomes. Two very interesting papers about #osmotic #nephrosis after #SGLT2i were reviewed:
🔓pubmed.ncbi.nlm.nih.gov/33855322/
🔓pubmed.ncbi.nlm.nih.gov/32387022/
(see photo)
🔓pubmed.ncbi.nlm.nih.gov/33855322/
🔓pubmed.ncbi.nlm.nih.gov/32387022/
(see photo)

15a) In the same talk, Prof Kanbay proposed #AKI high risk situations for patients on #SGLT2i and measures for reducing AKI risk:
👉hypovolemia/hypotension – restoration of volume depletion
👉 #RAAS blockers- close renal function and volume status follow up
👉hypovolemia/hypotension – restoration of volume depletion
👉 #RAAS blockers- close renal function and volume status follow up
15b)
👉diuretics – dose adjustment, close renal function and volume status follow up
👉 NSAIDs, cyclosporine, mannitol, amphotericin – avoid use together with #SGLT2i
👉 radiocontrast agents- stop SGLT2i before radiocontrast studies
👉 advanced age warrants close follow-up
👉diuretics – dose adjustment, close renal function and volume status follow up
👉 NSAIDs, cyclosporine, mannitol, amphotericin – avoid use together with #SGLT2i
👉 radiocontrast agents- stop SGLT2i before radiocontrast studies
👉 advanced age warrants close follow-up
16) More and more data about #SGTL2i! Are they as effective regardless of the use or non-use of target doses of ACEi/ARBs? Prof Hiddo Lambers Heerspink 🇳🇱 presented a post hoc analysis of #DAPA_CKD to answer this question!
17) Patients with #CKD with or without #T2D were randomized to dapagliflozin or placebo. Included subjects were treated with target or stable dose of #ACEi/ARBs. Primary composite outcome: sustained ≥50% #eGFR decline, #ESKD, or ☠️from a kidney/CV cause.
18) This post hoc analysis including 4296 patients with available data of ACEi/ARBs use, showed that in patients on placebo the event rate for the primary outcome was highest among participants not using ACEi/ARBs.
19) However, the benefit of dapagliflozin on the primary outcome was consistent regardless of use or non-use of the target dose of ACEi/ARBs, as shown in this figure. This benefit was also present for a secondary composite #cardiovascular outcome. 

20a) So that's a wrap on the latest #SGLT2i data out of @ERAkidney #ERA22. Let's make sure we are up to date:
In which clinical scenarios are SGLT2i beneficial in terms of cardiorenal protection?
A) no use of ACEi/ARBs
B) kidney transplant
C) concomitant use of diuretics
D) in all of them, but if they are used together with diuretics we should evaluate carefully volume status
A) no use of ACEi/ARBs
B) kidney transplant
C) concomitant use of diuretics
D) in all of them, but if they are used together with diuretics we should evaluate carefully volume status
21) Mark your best response and return tomorrow for the correct answer & MORE from #ERA22, & then a link to your 🆓CE/#CME!
👏@shbermejo @PepaSolerR @JonathanNefro @edgarvlermamd @nephondemand @HecmagsMD @ChristosArgyrop @torra_roser @EmiliSanAlv @jlgorriz #FOAMed @MedTweetorials
👏@shbermejo @PepaSolerR @JonathanNefro @edgarvlermamd @nephondemand @HecmagsMD @ChristosArgyrop @torra_roser @EmiliSanAlv @jlgorriz #FOAMed @MedTweetorials
22a) WELCOME BACK! I am @ClaraGCarro and we are discussing #DKD highlights from the recent #ERA22 congress. Yesterday (scroll ⤴️!) we discussed new data on #SGLT2i (as did my colleague @shbermejo last week--see ckd-ce.com/dkd12_ERA22a) & today we talk #GLPRA #DPP4i & #MRAs.
22b) As to yesterday's poll (tweet #20). If you didn't yet answer, please scroll up and COMMIT!
waiting
waiting
waiting
The correct answer is D. While on #SGLT2i therapy, hypovolemia should be avoided & diuretic use must be monitored.
waiting
waiting
waiting
The correct answer is D. While on #SGLT2i therapy, hypovolemia should be avoided & diuretic use must be monitored.
23) Now we move to #GLP1_RA! GLP1-RA kidney-protective effects (⬇️in proteinuria, preservation of #eGFR) were observed in CV outcomes trials #CVOT. FLOW is the first trial specifically designed to evaluate the effect of #semaglutide on major renal outcomes in #DKD patients 



24) #FLOW is an ongoing trial; 3535 patients were included. Patients baseline characteristics were presented at the congress: mean eGFR 47.0 mL/min/1.73 m2 (79.6% < 60) and mean UACR 567 mg/g (68.5% > 300 mg/g), mean #BMI was 32 kg/m2 and 95.8% were on #RAAS inhibition.
25) Baseline characteristics of #FLOW study confirm that this study will in fact evaluate #semaglutide effect in kidney outcomes in patients at very high risk of renal progression. This study was presented by Vlado Perkovic @VladoPerkovic 

26) Real world data about #semaglutide in patients with #DKD were presented by Gottfried Rudofsky 🇨🇭 in a pooled post hoc analysis of #SURE studies (all of them ~30 weeks’ duration) according to eGFR. 

27) This work included 913 patients on #semaglutide and other anti-hyperglycaemic drugs. Significant changes in #HbA1c and body weight were observed in eGFR>30 ml/min/m2. Rates of serious adverse reactions were low in all eGFR groups. Only 3.8% required drug discontinuation. 

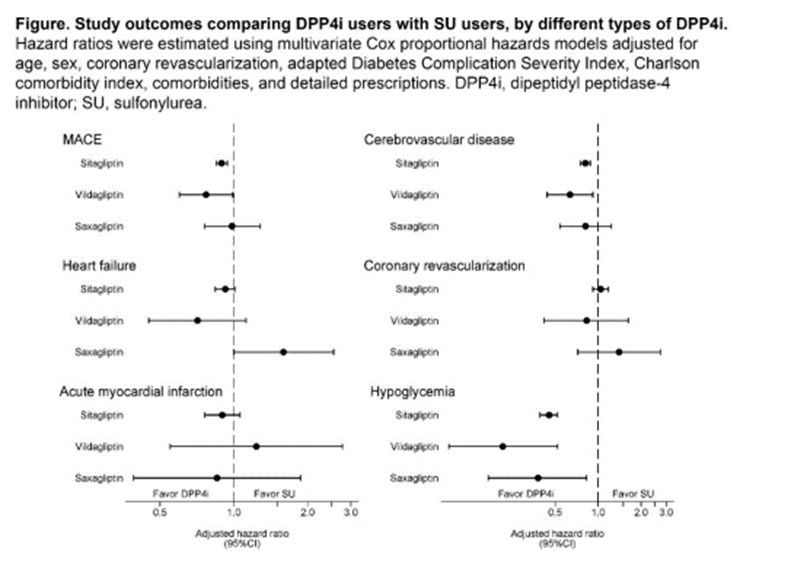
28) Another interesting work was presented by Hon-Yen Wu 🇹🇼 comparing the effectiveness of #DPP4 inhibitors versus sulfonylureas in addition to metformin in a population-based cohort study of 37,317 patients in Taiwan with a mean follow-up of 2.1 years. 

29) This work showed that patients on #DDP4i were at low risk of #MACE, #cerebrovascular disease, & #hypoglycemia when compared with matched pairs on sulfonylureas. Use of #sitagliptin & #vildagliptin were also linked to a lower risk of #heartfailure. 
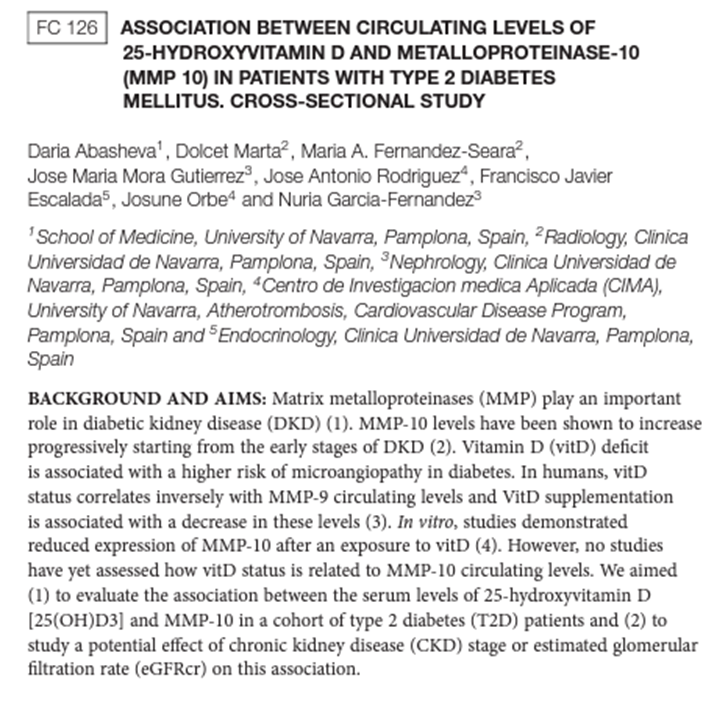
30) Matrix metalloproteinase 10 (#MMP10) is known to be implicated in diabetic #microvascular complications and its levels increase progressively from early stages of #DKD.
31) @nrgarciaunaves1 🇪🇸 group presented a work based on data of 256 #T2D patients that showed serum MMP-10 levels were inversely associated to 25(OH)D3 levels, especially in patients with #CKD, suggesting that higher values of 25(OH)D3 should be targeted in patients with DKD. 


32) Albuminuria as a risk factor for dementia presented by Gaye Hafez 🇹🇷 was a very motivating talk. Prof Hafez linked albuminuria and dementia, being risk factors for both entities the same (hypertension, diabetes…). 



33) She also raised a very interesting question: in primary nephropathies, is the kidney damage responsible for endothelial dysfunction and that causes dementia? Or is it a primary endothelial problem that causes renal impairment and dementia? 

34) Finally, what about #finerenone? #MRA were reviewed in a specific session at the #ERA22 congress on Sunday! First of all, a image to remember cardiorenal benefits of MRA by J Barrera-Chimal @barrera_lab 🇨🇦, pubmed.ncbi.nlm.nih.gov/34675379/ 

35) When compared to steroidal MRAs, finerenone has:
👉a similar potency to MR to spironolactone
👉a higher selectivity to MR than spironolactone/eplerenone
👉absence of CNS penetration
👉absence of sexual side effects
👉lower effect on BP than spironolactone/eplerenone
👉a similar potency to MR to spironolactone
👉a higher selectivity to MR than spironolactone/eplerenone
👉absence of CNS penetration
👉absence of sexual side effects
👉lower effect on BP than spironolactone/eplerenone
36) Prof George Bakris @BakrisGeorge 🇺🇸 reviewed #FIDELITY-DKD data, a pooled analysis of #FIGARO_DKD & #FIDELIO_DKD ➡️ 13171 #T2D pts randomized to finerenone (10 or 20 mg) or placebo, with a median follow up of 3 years. Mean #eGFR was 57 ml/min/1.73m2 and mean #UACR 515 mg/g. 
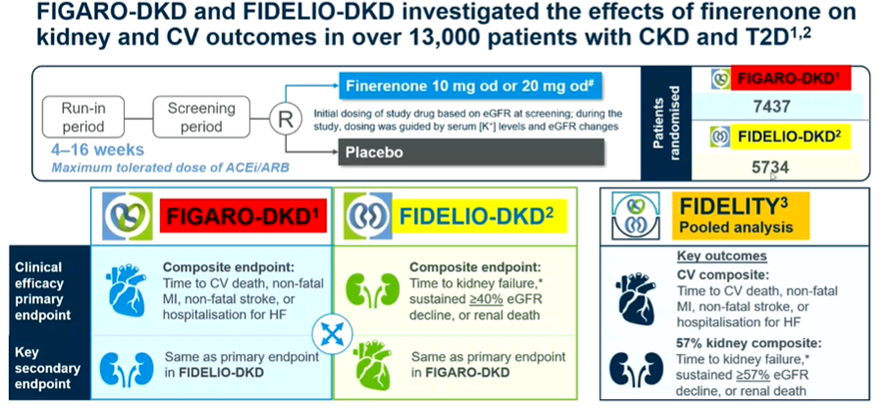
37) In this analysis, finerenone significantly reduced the risk of primary CV outcome by 14%, driven almost exclusively by #heartfailure protection. The benefits were consistent regardless baseline eGFR/UACR and the use of #SGLT2i or #GLP1RA. 

38) In this pooled analysis, finerenone reduced by 23% the risk of the renal composite outcome, and reduced all the components of this kidney composite outcome. Only 1.7% patients required drug discontinuation while 14% presented any grade of hyperkalemia. 

39) So, what are the three strategies to stop #CKD progression in our #DKD patients?
👉ACEi/ARBs
👉SGLTi
👉Nonsteroidal MRAs
And it is necessary to use these three drugs together to an increased benefit!
👉ACEi/ARBs
👉SGLTi
👉Nonsteroidal MRAs
And it is necessary to use these three drugs together to an increased benefit!
40a) Finally, Prof @KatherineTuttl8 🇺🇸 presented a terrific talk about how to start using #finerenone in everyday clinical practice. Main limitation: hyperkalemia. Clue points to start finerenone use:
40b) 👉 Hyperkalemia mitigating factors: concomitant use of diuretics and SGLT2i.
👉 eGFR 60-25 ml/min/1.73m2 25 ml/min/1.73m3 prior to starting treatment: use 10 mg dose
👉 Do not start finerenone if eGFR <25 25 ml/min/1.73m2 and/or serum potassium > 4.5
👉 eGFR 60-25 ml/min/1.73m2 25 ml/min/1.73m3 prior to starting treatment: use 10 mg dose
👉 Do not start finerenone if eGFR <25 25 ml/min/1.73m2 and/or serum potassium > 4.5
41) In summary, presentations at #ERA22 supported the conviction that use of combined treatment with RAAS blockade, SGLT2i, GLP1-RA and NS-MRA is the way we should follow in our clinical practice to stop progression in CKD patients with T2D.
42) And that's it! Now go and claim your 🆓CE/#CME at ckd-ce.com/dkd12_ERA22b/ and FOLLOW US for more #accredited #tweetorials in the #cardiorenal & #cardiometabolic spaces. I am @ClaraGCarro. Thanks for joining us!
• • •
Missing some Tweet in this thread? You can try to
force a refresh









