1/ Medical Case
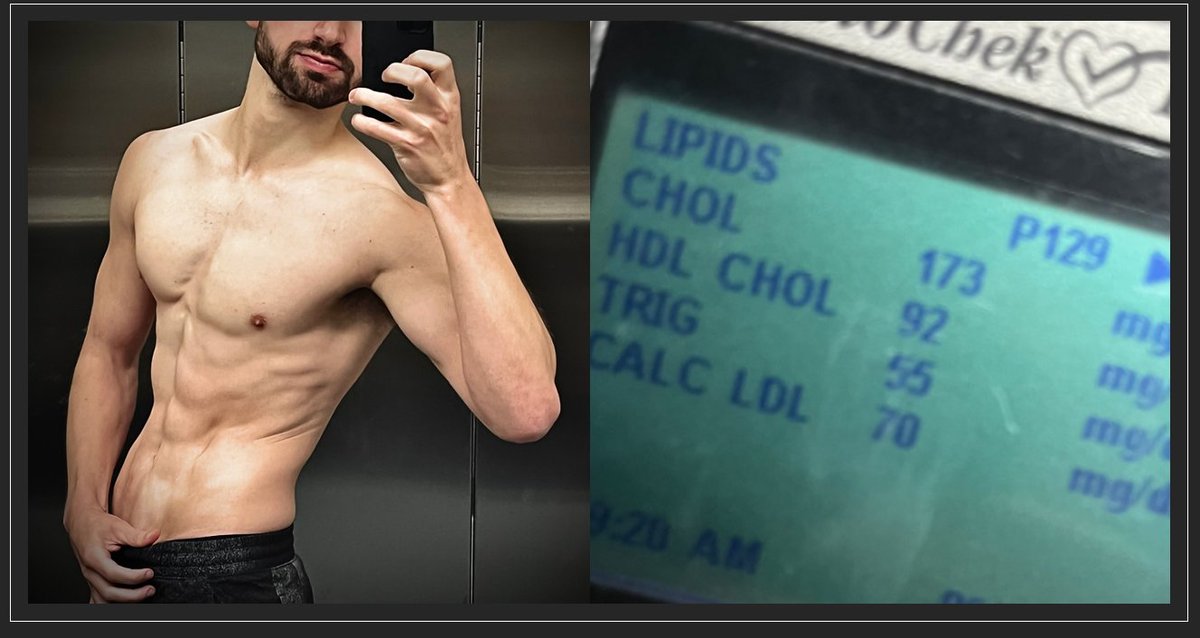
👉53y M, #LMHR w LDL 394, HDL 111, TG 40 for 4y on #keto diet
👉BMI 21.6
👉Prior to keto LDL was 98 mg/dl
👉CCTA shows no plaque, CAD-RADS = 0
👉Parents both lived to >80y w/o cardiac events Family hx of neurodegenerative diseases, including 2x of 👉Parkinson’s
👉53y M, #LMHR w LDL 394, HDL 111, TG 40 for 4y on #keto diet
👉BMI 21.6
👉Prior to keto LDL was 98 mg/dl
👉CCTA shows no plaque, CAD-RADS = 0
👉Parents both lived to >80y w/o cardiac events Family hx of neurodegenerative diseases, including 2x of 👉Parkinson’s

2/ Patient doesn’t want to abandon diet because it makes them “feel my best.”
You’ll notice, there’s no poll associated with this case. Medicine isn’t a democracy and not all medical opinions on Twitter are equally informed. However, I wanted to share this case ...
You’ll notice, there’s no poll associated with this case. Medicine isn’t a democracy and not all medical opinions on Twitter are equally informed. However, I wanted to share this case ...
3/ ...as a juxtaposition to the extremism I’m seeing ON BOTH SIDES: LDL/ApoB is benign v. lower is better (period). Neither is the case. A bit of nuance…
With respect to “LDL/ApoB is benign,” all things being equal, the data don’t support this view. It’s a risk factor...
With respect to “LDL/ApoB is benign,” all things being equal, the data don’t support this view. It’s a risk factor...
4/ ... part of a causal pathway. Are there potentially more important risk factors? I think so, personally.
And should it Always be lowered medically. Well, if this were the case, everyone should be on meds to get levels to as close to 0 as possible. Which brings us to…
And should it Always be lowered medically. Well, if this were the case, everyone should be on meds to get levels to as close to 0 as possible. Which brings us to…
5/ “lower [ApoB] is better”
My issue with this catchphrase is that it is a blanket statement that discards competing medical considerations. I like this case as it highlights the fault of oversimplifications. Is having LDL in the basement, like 40, 30, or even 20 mg/dl, good?...
My issue with this catchphrase is that it is a blanket statement that discards competing medical considerations. I like this case as it highlights the fault of oversimplifications. Is having LDL in the basement, like 40, 30, or even 20 mg/dl, good?...
6/ For ASCVD let’s assume yes. But this patient has a clean CCTA and no fam hx of heart disease. By contrast, he has a family hx of PD for which low ApoB might increase risk (2019 data from Circulation Research, IF 17 AHA-associated journal: pubmed.ncbi.nlm.nih.gov/31382822/). 



7/ So, is medicating down the LDL with a statin the best path, even were the patient agreeable? Open question without a clear answer.
IMHO "we" need to feel more conformable saying, honestly, “I don’t know, but here are the factors…”
IMHO "we" need to feel more conformable saying, honestly, “I don’t know, but here are the factors…”
8/Then the patient decides, which is always the case anyway
… “and let’s pursue more research that will help us cover clinical gray zones in future.”
This summarizes why I’m interested in studying #LMHR #LMHRstudy @realDaveFeldman
… “and let’s pursue more research that will help us cover clinical gray zones in future.”
This summarizes why I’m interested in studying #LMHR #LMHRstudy @realDaveFeldman
• • •
Missing some Tweet in this thread? You can try to
force a refresh