🩸🧠What’s new in Cerebral Amyloid Angiopathy?
🚀Updates from the 8th International CAA Conference
#iCAAPerth2022 🌏🇦🇺
..and my take (denoted by:🧔🏻)
*Focus of 🧵 will be on clinical/translational aspects*
#AmyloidAngiopathy #neurotwitter #stroke #Neurology #dementia #NeuroRad
🚀Updates from the 8th International CAA Conference
#iCAAPerth2022 🌏🇦🇺
..and my take (denoted by:🧔🏻)
*Focus of 🧵 will be on clinical/translational aspects*
#AmyloidAngiopathy #neurotwitter #stroke #Neurology #dementia #NeuroRad

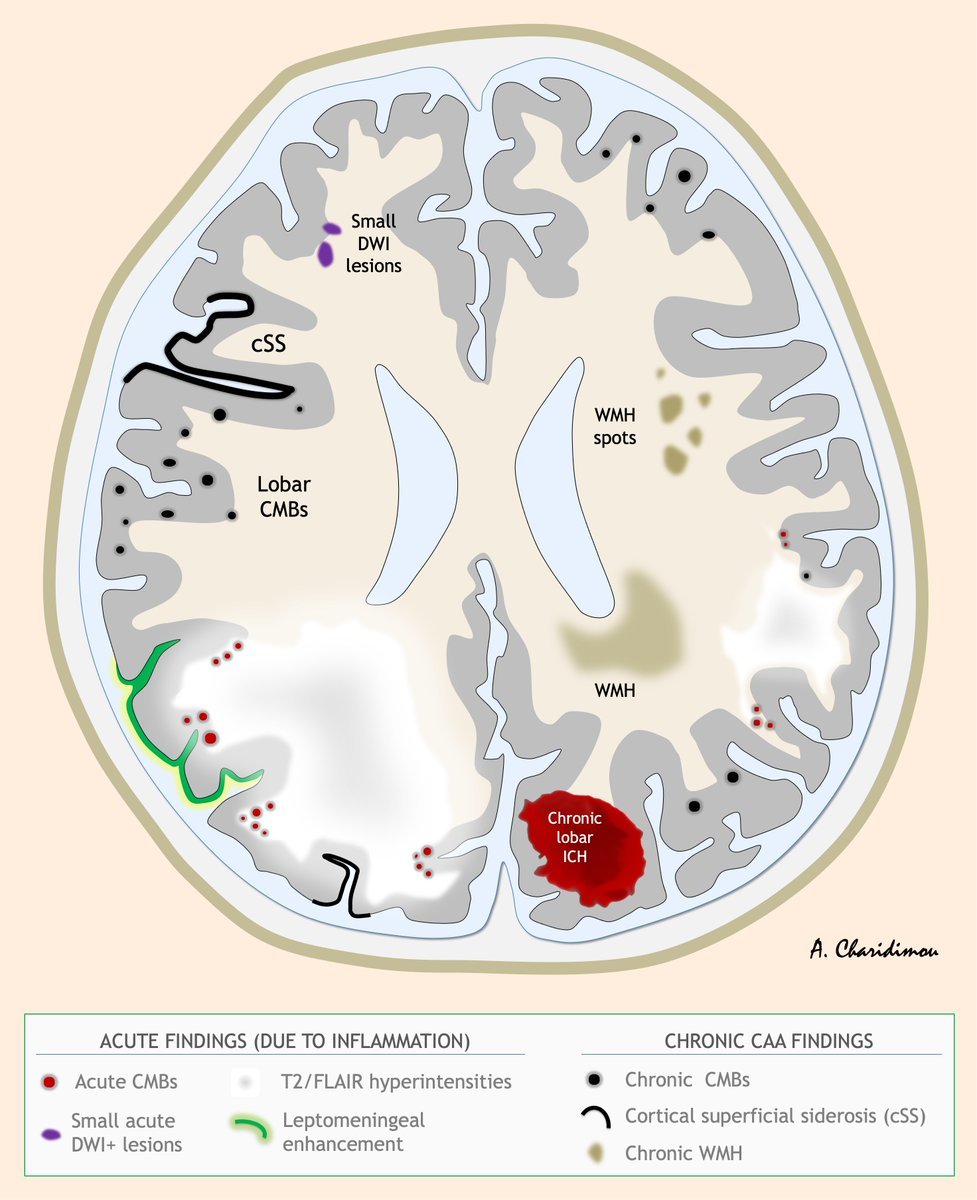
🔥🧠CAA-ri (CAA-related inflammation)
@Ellis_van_Etten provided a clinical update on CAA-ri
-Key need for improving diagnostic tools and clarifying best 🧯treatment options
🧔🏻: Subclinical, non-fulminant CAA-ri forms are beginning to be appreciated!
/2
@Ellis_van_Etten provided a clinical update on CAA-ri
-Key need for improving diagnostic tools and clarifying best 🧯treatment options
🧔🏻: Subclinical, non-fulminant CAA-ri forms are beginning to be appreciated!
/2

🔥🧠CAA-ri
Focal microglial activation found in areas of edema, also correlating with anti-Aβ autoAbs CSF levels
via: @iCABNetwork @Prof_Piazza
🧔🏻: we urgently need validation of 🧪CSF anti-Aβ Abs for clinical use-will be a game changer in CAA-ri
n.neurology.org/content/99/12/…
/3
Focal microglial activation found in areas of edema, also correlating with anti-Aβ autoAbs CSF levels
via: @iCABNetwork @Prof_Piazza
🧔🏻: we urgently need validation of 🧪CSF anti-Aβ Abs for clinical use-will be a game changer in CAA-ri
n.neurology.org/content/99/12/…
/3

🔥🧠CAA-ri
Draft recommendations for CAA-ri diagnosis and treatment were discussed (@UCLStrokeRes @Ellis_van_Etten @MGHNeurology)
🧔🏻: Nice clarification on nomenclature, when to perform 🧠biopsy and timing of MRI f/up - stay tuned #neurotwitter!
/4
Draft recommendations for CAA-ri diagnosis and treatment were discussed (@UCLStrokeRes @Ellis_van_Etten @MGHNeurology)
🧔🏻: Nice clarification on nomenclature, when to perform 🧠biopsy and timing of MRI f/up - stay tuned #neurotwitter!
https://twitter.com/a_charidimou/status/1529817256670048257?s=20&t=n5ai759fEDbx5On0-wNDTA
/4
🩺CAA diagnostics
🏥I talked about diagnostic perspectives, approach for Boston Criteria v2.0 @TheLancetNeuro, role of 🌈amyloid-PET and core 🧪CSF markers
Clinical recommendations underway @VCI_EricSmith
@ReiniervdZwet great abstract on the Boston Criteria v2 in D-CAA!
/5
🏥I talked about diagnostic perspectives, approach for Boston Criteria v2.0 @TheLancetNeuro, role of 🌈amyloid-PET and core 🧪CSF markers
Clinical recommendations underway @VCI_EricSmith
@ReiniervdZwet great abstract on the Boston Criteria v2 in D-CAA!
/5
🩺CAA diagnostics
@CSF_Tweet provided a comprehensive update on fluid biomarkers in CAA
@RalphNMartins1 gave a tour-de-force talk on blood biomarkers
🧔🏻: a specific CSF/serum panel to differentiate CAA from AD will be neat
/6
@CSF_Tweet provided a comprehensive update on fluid biomarkers in CAA
@RalphNMartins1 gave a tour-de-force talk on blood biomarkers
🧔🏻: a specific CSF/serum panel to differentiate CAA from AD will be neat
/6
🦩CAA biomarkers
@SMGreenbergNeur presented a cool pathophysiological model based on presumed CAA stages (which evolve over 3-4 decades of life) as a framework for interpreting and incorporating the range of biomarkers linked to CAA--->selecting outcomes markers for RCTs
/7
@SMGreenbergNeur presented a cool pathophysiological model based on presumed CAA stages (which evolve over 3-4 decades of life) as a framework for interpreting and incorporating the range of biomarkers linked to CAA--->selecting outcomes markers for RCTs
/7

🦩CAA biomarkers
Really enjoyed data presented on subarachnoid CSF hyperintensities at 7T FLAIR, which seem to be strongly associated with cSS @MariekeWermer @SabineV159
🧔🏻: suspect these are sub-acute sulcal SAHs🩸 - we sometimes see them on clinical scans, @gboulouis?
/8
Really enjoyed data presented on subarachnoid CSF hyperintensities at 7T FLAIR, which seem to be strongly associated with cSS @MariekeWermer @SabineV159
🧔🏻: suspect these are sub-acute sulcal SAHs🩸 - we sometimes see them on clinical scans, @gboulouis?
/8

🦩CAA biomarkers
Within the cSS theme, @MarielKozberg presented extremely interesting preliminary data on mouse models of CAA-related cortical superficial siderosis to study potential secondary injury.
🧔🏻: I'm excited to see what this work reveals! #neuroscience
/9
Within the cSS theme, @MarielKozberg presented extremely interesting preliminary data on mouse models of CAA-related cortical superficial siderosis to study potential secondary injury.
🧔🏻: I'm excited to see what this work reveals! #neuroscience
/9

🦩CAA biomarkers
@ValentinaPerosa convised us about the usefulness of
Quantitative Susceptibility Mapping (QSM) on @microbleeds assessment and classification of the participants in subgroups. @JohannaRotta
🧔🏻: together with automated methods, QSM is the way forth!
/10
@ValentinaPerosa convised us about the usefulness of
Quantitative Susceptibility Mapping (QSM) on @microbleeds assessment and classification of the participants in subgroups. @JohannaRotta
🧔🏻: together with automated methods, QSM is the way forth!
/10

🦩CAA biomarkers
Developments in MRI biomarkers in Dutch-CAA continue to lead to many observations and translation in sporadic CAA patients. EDAN, TRACK D-CAA study @MariekeWermer
🧔🏻: pave the way for a future proof-of-concept trial in this population
/11
Developments in MRI biomarkers in Dutch-CAA continue to lead to many observations and translation in sporadic CAA patients. EDAN, TRACK D-CAA study @MariekeWermer
🧔🏻: pave the way for a future proof-of-concept trial in this population
/11
🦩CAA biomarkers
@BeaudinAE @VCI_EricSmith showed elegant data on 🧠structural connectome~cerebrovascular reactivity. CAA patients have disrupted brain structural network, associated with ⬇️ 🧠ability to ⬆️blood flow when needed.
🧔🏻: novel link to neurological dysfunction
/12
@BeaudinAE @VCI_EricSmith showed elegant data on 🧠structural connectome~cerebrovascular reactivity. CAA patients have disrupted brain structural network, associated with ⬇️ 🧠ability to ⬆️blood flow when needed.
🧔🏻: novel link to neurological dysfunction
/12
🦚Clinical spectrum
@DrGargiBanerjee gave an excellent update on the emerging phenomenon of iatrogenic CAA (development of CAA in young adults after transmission via #Neurosurgery)
🧔🏻: ⬆️awareness and recognition, is leading to more cases popping 🌎
jnnp.bmj.com/content/93/7/6…
/13
@DrGargiBanerjee gave an excellent update on the emerging phenomenon of iatrogenic CAA (development of CAA in young adults after transmission via #Neurosurgery)
🧔🏻: ⬆️awareness and recognition, is leading to more cases popping 🌎
jnnp.bmj.com/content/93/7/6…
/13
🦚Clinical spectrum
On the same intriguing iatrogenic CAA topic, @KKaushikMD presented a new case series from🇳🇱, increasing significantly the total number of reported cases!
🧔🏻: harmonization, registries, awareness will be key! @UCLStrokeRes
/14
On the same intriguing iatrogenic CAA topic, @KKaushikMD presented a new case series from🇳🇱, increasing significantly the total number of reported cases!
🧔🏻: harmonization, registries, awareness will be key! @UCLStrokeRes
/14
🦚Clinical spectrum
Studies to date primarily focused on #stroke CAA manifestations, we now recognise that CAA is consistently linked to progressive neurocognitive, neurobehavioral, and neuropsychiatric symptoms!
@KKaushikMD, @VCI_EricSmith showed new data on these symptoms
/15
Studies to date primarily focused on #stroke CAA manifestations, we now recognise that CAA is consistently linked to progressive neurocognitive, neurobehavioral, and neuropsychiatric symptoms!
@KKaushikMD, @VCI_EricSmith showed new data on these symptoms
/15
🦚Clinical spectrum
New data @UCLStrokeRes on neuropsychological investigation of CAA: verbal IQ and non-verbal IQ most frequently impaired cognitive domains, followed by executive functions and processing speed.
🧔🏻: CAA cognitive impairment profile~more global than thought
/16
New data @UCLStrokeRes on neuropsychological investigation of CAA: verbal IQ and non-verbal IQ most frequently impaired cognitive domains, followed by executive functions and processing speed.
🧔🏻: CAA cognitive impairment profile~more global than thought
/16
🦚Clinical spectrum
Huge differences on prevalence of CAA pathology and CAA-related🩸🧠 in Eastern⬇️ vs Western countries.
🧔🏻: differences in genetic/environmental risk factors?
wonder what the implications are for CAA diagnosis and #BostonCriteria
/17
Huge differences on prevalence of CAA pathology and CAA-related🩸🧠 in Eastern⬇️ vs Western countries.
🧔🏻: differences in genetic/environmental risk factors?
wonder what the implications are for CAA diagnosis and #BostonCriteria
/17
🦚Clinical spectrum
@ClaireMullerCCL is collecting a growing cohort of
sporadic CAA in Queensland, via her role in a comprehensive stroke centre and quaternary referral service
🧔🏻: Claire, I am looking forward for novel observations and potential collaborations!!
/18
@ClaireMullerCCL is collecting a growing cohort of
sporadic CAA in Queensland, via her role in a comprehensive stroke centre and quaternary referral service
🧔🏻: Claire, I am looking forward for novel observations and potential collaborations!!
/18
💊 CAA management
Recommendations underway for the thorny dilemma of CAA and AFib management @BleedingStroke @Ash_Shoamanesh
🧔🏻: no surprised there - randomise pts! My approach when this is not an option ⬇️ @WorldStrokeEd @interneurona #neurotwitter
/19
Recommendations underway for the thorny dilemma of CAA and AFib management @BleedingStroke @Ash_Shoamanesh
🧔🏻: no surprised there - randomise pts! My approach when this is not an option ⬇️ @WorldStrokeEd @interneurona #neurotwitter
/19
https://twitter.com/a_charidimou/status/1573152654997524481?s=20&t=D55kJk_qIkE2psM7SOMHLA
💊 CAA management
Recommendations underway also for blood pressure & other meds in CAA @PrCCordonnier
Excellent talk @lsveikata on Long-term Blood Pressure Variability ~ White Matter Microstructural Integrity in CAA
/20
Recommendations underway also for blood pressure & other meds in CAA @PrCCordonnier
Excellent talk @lsveikata on Long-term Blood Pressure Variability ~ White Matter Microstructural Integrity in CAA
/20

🤯Disease-modifying treatments in CAA
-Proteomics to find molecular targets
-Anti-ApoE approaches promising
-Fibrinolytic system, is plasmin a therapeutic target?
🧔🏻: the holy grail in the field!⛪️
/21
-Proteomics to find molecular targets
-Anti-ApoE approaches promising
-Fibrinolytic system, is plasmin a therapeutic target?
🧔🏻: the holy grail in the field!⛪️
/21
Other:
- many new exciting data on the role of perivascular drainage in CAA pathogenesis
-amazing preclinical work on prevascular fibroblasts by
@AndyShih_Lab and a dissection of the perivascular compartment
/22
- many new exciting data on the role of perivascular drainage in CAA pathogenesis
-amazing preclinical work on prevascular fibroblasts by
@AndyShih_Lab and a dissection of the perivascular compartment
/22
🚀🇦🇺Huge thanks to the organizing committee for putting together such a stellar meeting!! 👏🏻👏🏻👏🏻@HamidRSohrabi @RalphNMartins1 @SMGreenbergNeur @iCAAassociation
and team! Apologies that I didn't include all the amazing work that was presented last week #iCAAPerth2022!
and team! Apologies that I didn't include all the amazing work that was presented last week #iCAAPerth2022!
• • •
Missing some Tweet in this thread? You can try to
force a refresh