1) Welcome to our #accredited #tweetorial on clinical trial results and emerging data for treatment of Diabetes and CKD #DM in #CKD. I am Brian Rifkin MD, @brian_rifkin, from the Hattiesburg Clinic. #Nephtwitter #Medtwitter #FOAMed 

2) This #accredited #tweetorial series on #kidneydisease #CKD is supported by an independent educational grant from the Boehringer Ingelheim/Lilly Alliance. It is not intended for US- or UK-based HCPs. Accreditation statement & faculty disclosures at ckd-ce.com/disclosures/.
3) This activity is accredited for #physicians #physicianassociates #nurses #NPs #pharmacists. Prior programs in this series, still eligible for CE/#CME, can be accessed at ckd-ce.com. FOLLOW US to learn from expert faculty!
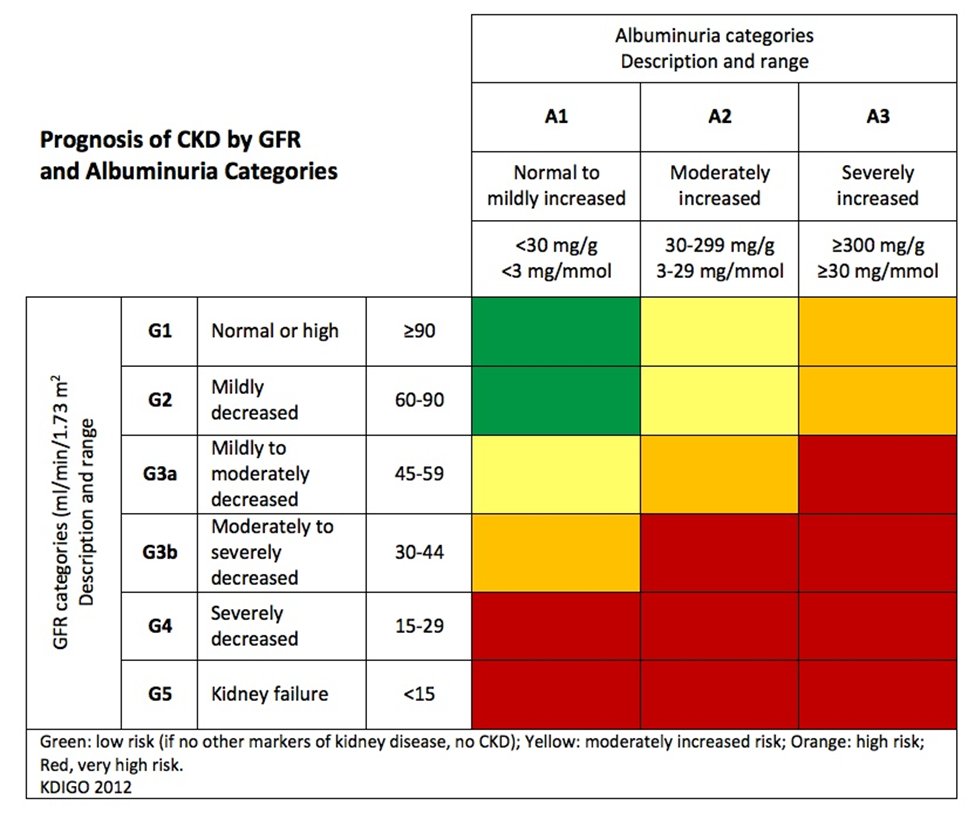
4) Today we are specifically going to look at the evidence for a multi-disciplinary approach to protection of the patient with #diabetes and #CKD (G1A1-G2A3), but first a quiz! 
5) Poll: What do you recommend to slow the progression of diabetic #nephropathy in patients with CKD 1-2?
a. RAS blockers
b. SGLT2i
c. Weight loss
d. Blood pressure control
a. RAS blockers
b. SGLT2i
c. Weight loss
d. Blood pressure control
6) Doing studies in pts with an #eGFR > 60 is difficult. It might take decades to get the number of events to prove benefit in renal/cardiac/mortality endpoints. Some recommendations are therefore extrapolated from studies of more severe CKD, with an eye on risks/benefits. 

7) Given the complexity of #diabetes and #CKD management, it is best to take a multidisciplinary approach. Diabetes in CKD requires medication, dietary and often lifestyle modification. 

8) For the 1st half of this tweetorial we are going to focus on lifestyle and monitoring of patients with #diabetes and early CKD (G1-2). In the 2nd half we will examine the benefits of specific medication classes. 

9) Smoking Cessation
850M w/#CKD in the world, only about 2M on #dialysis.
Risk of death >>> risk of ESKD, usually #CV death prior to dialysis need.
Although no direct evidence in ↓CKD, quitting 🚬 is recommended by all medical societies, & is linked to CV mortality.
850M w/#CKD in the world, only about 2M on #dialysis.
Risk of death >>> risk of ESKD, usually #CV death prior to dialysis need.
Although no direct evidence in ↓CKD, quitting 🚬 is recommended by all medical societies, & is linked to CV mortality.

10) Physical Activity
Rec light-moderate intensity as tolerated.
Few studies in #DM & #CKD, rec's derived from general pop studies.
Meta-analysis of #RCTs in #nondialysis CKD actually showed no effect on kidney function, but time & intensity may matter.
🔓pubmed.ncbi.nlm.nih.gov/33097801/
Rec light-moderate intensity as tolerated.
Few studies in #DM & #CKD, rec's derived from general pop studies.
Meta-analysis of #RCTs in #nondialysis CKD actually showed no effect on kidney function, but time & intensity may matter.
🔓pubmed.ncbi.nlm.nih.gov/33097801/

11) Education Programs
Systematic review supported the efficacy of a well-structured self-management program.
Improves surrogate outcomes including #BP and glucose control.
Should be individualized, and is generally considered cost-effective.
Systematic review supported the efficacy of a well-structured self-management program.
Improves surrogate outcomes including #BP and glucose control.
Should be individualized, and is generally considered cost-effective.

12a) Protein Intake
@goKDIGO: 0.8 g/kg/d in adults regardless of #eGFR (not on #dialysis).
@NKF #KDOQI: 0.6-0.8 g/kg/d in CKD 3-5 with #diabetes.
@goKDIGO: 0.8 g/kg/d in adults regardless of #eGFR (not on #dialysis).
@NKF #KDOQI: 0.6-0.8 g/kg/d in CKD 3-5 with #diabetes.
12b) Protein source: plant (base) vs animal (acid) has shown benefits in large cohort studies.
Dietary education should start in diabetics with CKD 1-2.
See 🔓pubmed.ncbi.nlm.nih.gov/26789417/
Dietary education should start in diabetics with CKD 1-2.
See 🔓pubmed.ncbi.nlm.nih.gov/26789417/

13) Weight Loss/ Bariatric Surgery
In observational studies, ↑ BMI is associated with a higher risk of #HTN and #DM, and a modest risk factor for #CKD.
Propensity matched study of 985 pts showed long-term GFR decline attenuated by bariatric surgery: 🔓pubmed.ncbi.nlm.nih.gov/27181999/
In observational studies, ↑ BMI is associated with a higher risk of #HTN and #DM, and a modest risk factor for #CKD.
Propensity matched study of 985 pts showed long-term GFR decline attenuated by bariatric surgery: 🔓pubmed.ncbi.nlm.nih.gov/27181999/

14) Glycemic Target
#HbA1c, glycated albumin, #fructosamine correlation w/ plasma glucose weakens w/advanced #CKD.
Glycated albumin & fructosamine influenced by low albumin. HbA1c influenced by #anemia.
#CGM (continuous glucose monitoring) not known to be influenced by CKD level.
#HbA1c, glycated albumin, #fructosamine correlation w/ plasma glucose weakens w/advanced #CKD.
Glycated albumin & fructosamine influenced by low albumin. HbA1c influenced by #anemia.
#CGM (continuous glucose monitoring) not known to be influenced by CKD level.

15) Glycemic Target
HbA1c goals should be individualized, esp in elderly.
Intensive glucose control is associated with ↑ CV mortality in advanced #CKD.
@goKDIGO recommends lower #HbA1C goals in healthy pts with CKD 1-2 & w/low risk of hypoglycemia & good educational support.
HbA1c goals should be individualized, esp in elderly.
Intensive glucose control is associated with ↑ CV mortality in advanced #CKD.
@goKDIGO recommends lower #HbA1C goals in healthy pts with CKD 1-2 & w/low risk of hypoglycemia & good educational support.

16) Poll: Which one of the following is accurate regarding a systolic BP < 120 versus < 140 mmHg?
a. All cause mortality ↓
b. #CKD slowed with ↓ BP
c. More #ESKD in ↓ BP
a. All cause mortality ↓
b. #CKD slowed with ↓ BP
c. More #ESKD in ↓ BP
17a) BP Control
↓ BP did not prevent worse kidney outcomes in #SPRINT (pts w/o DM). ↓ BP was associated with ↓ all cause mortality (A).
↓ BP did not prevent worse kidney outcomes in #SPRINT (pts w/o DM). ↓ BP was associated with ↓ all cause mortality (A).
17b) Of note in SPRINT, pts with eGFR > 90 had 3.5 X greater risk of ↓ in eGFR to < 60 with intensive control. Might just represent hemodynamic change.
See 🔓pubmed.ncbi.nlm.nih.gov/31983312/
See 🔓pubmed.ncbi.nlm.nih.gov/31983312/

18) BP control
Because pts w/#DM, & especially w/#proteinuria > 1 gram/d, are at risk for accelerated ↓ in eGFR, a BP goal of <130/80 is recommended.
Although control of moderately elevated BP has not been linked to improved #CKD, #BP control is still important in #CV outcomes.
Because pts w/#DM, & especially w/#proteinuria > 1 gram/d, are at risk for accelerated ↓ in eGFR, a BP goal of <130/80 is recommended.
Although control of moderately elevated BP has not been linked to improved #CKD, #BP control is still important in #CV outcomes.
19) Hyperlipidemia
Given ↑ morbidity & mortality associated w/#CV disease in #DM and #CKD, lipid lowering therapy is often rec'd in #nondialysis CKD.
Statins alone or in combination with #ezetimibe.
Small studies suggest ↓ #albuminuria and slower decline in #eGFR w/statins.
Given ↑ morbidity & mortality associated w/#CV disease in #DM and #CKD, lipid lowering therapy is often rec'd in #nondialysis CKD.
Statins alone or in combination with #ezetimibe.
Small studies suggest ↓ #albuminuria and slower decline in #eGFR w/statins.

20) That’s all for part 1. Be sure to come back TOMORROW for part 2 and our discussion of medication use in #diabetes with #CKD G1-2.
21) Welcome back to our #accredited #tweetorial on emerging data for treatment of Diabetes and CKD #DM in #CKD. Today we are going to look at medication classes. I am Brian Rifkin MD, @brian_rifkin, from the Hattiesburg Clinic. #Nephtwitter #Medtwitter #FOAMed
22) So let’s pick up where we left off. which medications are considered first-line therapy in #diabetes with #CKD 1-2?
a. ACEi/ARB
b. MRAs
c. Metformin/SGLT2i
d. GLP1RA/sulfonylureas
a. ACEi/ARB
b. MRAs
c. Metformin/SGLT2i
d. GLP1RA/sulfonylureas
23a) Renin-Angiotensin System Blockade (#RASI)
Recommended to titrate to max tolerated dose.
Goal to reduce #proteinuria by at least 30%.
Recommended to titrate to max tolerated dose.
Goal to reduce #proteinuria by at least 30%.
23b) Interesting #RCT compared with placebo show the evidence behind this recommendation is only “moderate” in terms of mortality and doubling of SCr.
See 🔓pubmed.ncbi.nlm.nih.gov/17054288/
See 🔓pubmed.ncbi.nlm.nih.gov/17054288/

24a) RAS Blockade
Evidence for preservation of #eGFR in pts with #CKD 1-2 is limited.
#ACEi/#ARB in pts with eGFR < 60 & HTN WITHOUT ALBUMINURIA showed little benefit over other meds.
Evidence for preservation of #eGFR in pts with #CKD 1-2 is limited.
#ACEi/#ARB in pts with eGFR < 60 & HTN WITHOUT ALBUMINURIA showed little benefit over other meds.
24b) @goKDIGO/@ @AmDiabetesAssn discourage #RASi in normoalbuminuric, normotensive patients with diabetes. The answer to the ? in tweet 22 is C. 

25) RAS Blockade
#Hyperkalemia is less of a concern when used in CKD 1-2.
Increase of SCr < 30% from baseline with stabilization at 2-months is associated with long-term preservation of kidney function.
#Hyperkalemia is less of a concern when used in CKD 1-2.
Increase of SCr < 30% from baseline with stabilization at 2-months is associated with long-term preservation of kidney function.

26a) RAS Blockade
#MRAs are used in resistant #HTN & are shown to ↓ #proteinuria in CKD 1-4 in pts on ACEi/ARB.
Lack of long-term trials demonstrating cardiac/renal outcomes.
#MRAs are used in resistant #HTN & are shown to ↓ #proteinuria in CKD 1-4 in pts on ACEi/ARB.
Lack of long-term trials demonstrating cardiac/renal outcomes.
26b) #FIDELIO_DKD (#SGLT2i & #finerenone) included pts with CKD G1A3 & G2, but didn’t analyze this small subgroup.
See 🔓pubmed.ncbi.nlm.nih.gov/33264825/
See 🔓pubmed.ncbi.nlm.nih.gov/33264825/

27) #Metformin
Low cost, safe and has CV & CKD progression benefits.
Use may also be associated with weight loss.
No risk of #hypoglycemia as a single agent.
Can be considered as first-line therapy, minimal risk of lactic acidosis and no dosage adjustment needed CKD 1-2.
Low cost, safe and has CV & CKD progression benefits.
Use may also be associated with weight loss.
No risk of #hypoglycemia as a single agent.
Can be considered as first-line therapy, minimal risk of lactic acidosis and no dosage adjustment needed CKD 1-2.

28) #SGLT2 Inhibitor
Consistently shown to ↓ doubling SCr, ESKD, death from CV/kidney causes.
Benefits seen even in pts with #CV disease without CKD or proteinuria.
#EMPA_REG and #CANVAS: greatest benefit in ↑ risk pts, cardiac & kidney outcomes less pronounced in CKD 1-2.
Consistently shown to ↓ doubling SCr, ESKD, death from CV/kidney causes.
Benefits seen even in pts with #CV disease without CKD or proteinuria.
#EMPA_REG and #CANVAS: greatest benefit in ↑ risk pts, cardiac & kidney outcomes less pronounced in CKD 1-2.

29) SGLT2 Inhibitor
EMPA-KIDNEY: showed benefits in patients with eGFR < 90 ml/min, tho less so in the group w/ < 300 mg/g proteinuria at 2-years.
May be appropriate first-line for CKD 1-2 w/ #UACR > 1000 mg/g & high risk of rapid declining eGFR.
See 🔓pubmed.ncbi.nlm.nih.gov/36331190/
EMPA-KIDNEY: showed benefits in patients with eGFR < 90 ml/min, tho less so in the group w/ < 300 mg/g proteinuria at 2-years.
May be appropriate first-line for CKD 1-2 w/ #UACR > 1000 mg/g & high risk of rapid declining eGFR.
See 🔓pubmed.ncbi.nlm.nih.gov/36331190/

30) SGLT2 Inhibitor #SGLT2i
High cost currently with no generic available in the US.
Other side effects:
High cost currently with no generic available in the US.
Other side effects:

31) GLP1 Receptor Agonist #GLP1_RA
Use if glucose above goal on metformin & SGLT2i
CV benefits, but not a universal class effect.
No proven preservation of eGFR except w/ dulaglutide.
No hypoglycemia, may promote weight loss.
Side effects: GI irritation & injection site reaction.
Use if glucose above goal on metformin & SGLT2i
CV benefits, but not a universal class effect.
No proven preservation of eGFR except w/ dulaglutide.
No hypoglycemia, may promote weight loss.
Side effects: GI irritation & injection site reaction.
33) Summary
Preventing #ESKD and #dialysis are critical to patients’ longevity and quality of life.
Early screening and treatment may have significant effects on the trajectory of CKD.
Focusing on #CV health often also benefits kidney health.
Preventing #ESKD and #dialysis are critical to patients’ longevity and quality of life.
Early screening and treatment may have significant effects on the trajectory of CKD.
Focusing on #CV health often also benefits kidney health.
34) Summary
Lifestyle modification is important but difficult. ↑ activity, quit smoking & weight loss require a multidisciplinary approach. Goals should be individualized.
Medications are useful, especially in pts with > 1 g/day proteinuria and at ↑ risk of disease progression.
Lifestyle modification is important but difficult. ↑ activity, quit smoking & weight loss require a multidisciplinary approach. Goals should be individualized.
Medications are useful, especially in pts with > 1 g/day proteinuria and at ↑ risk of disease progression.
35) Summary
#SGLT2i & #metformin are appropriate 1st line meds in #DM & #CKD 1-2.
#RAS inhibitors should be used cautiously in early CKD w/o #proteinuria.
Treatment with RASi/SGLT2i/statins may be indicated in CKD pts with & without DM, but with other #CV disease risk factors.
#SGLT2i & #metformin are appropriate 1st line meds in #DM & #CKD 1-2.
#RAS inhibitors should be used cautiously in early CKD w/o #proteinuria.
Treatment with RASi/SGLT2i/statins may be indicated in CKD pts with & without DM, but with other #CV disease risk factors.
36) This has been @brian_rifkin with another educational #tweetorial from @ckd_ce. Claim your 🆓CE/#CME at ckd-ce.com/dkd19/. Come back to learn more nephrology!
👏@sophia_kidney @hellokidneyMD @ChristosArgyrop @edgarvlermamd @NephRodby @kidneymo @kdjhaveri @VelezNephHepato
👏@sophia_kidney @hellokidneyMD @ChristosArgyrop @edgarvlermamd @NephRodby @kidneymo @kdjhaveri @VelezNephHepato
• • •
Missing some Tweet in this thread? You can try to
force a refresh