In this opinion paper @RMedzhitov went back to drawing board to update his views on #allergy and how it could develop.
#immunology
I read this paper and here is my take on it
1/
#immunology
I read this paper and here is my take on it
1/
https://twitter.com/RMedzhitov/status/1349815141982986242
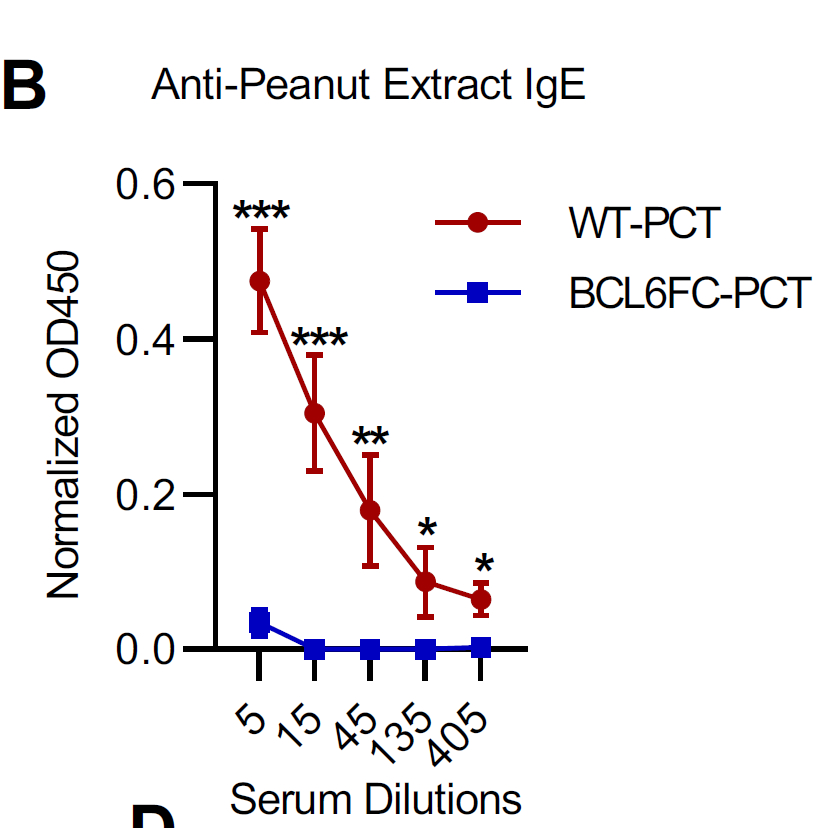
@RMedzhitov Why focus on allergy? b/c allergy is a paradox. The allergy we recognize is a completely maladaptive response and has no protective role whatsoever. It is not clear why do we even need IgE
2/
2/
@RMedzhitov So, some 10 years ago or so, @RMedzhitov started to suggest that #allergy is an intrinsic property of a certain type of #antigens, many of them with enzymatic function (enzymes). 3/
@RMedzhitov @RMedzhitov used the enzyme, papain, to test his hypothesis. And it kind of worked in mice.
But people are eating papaya (which contains papain) or pineapple (which contains bromelain), another enzyme used for these experiments, and not many reports some allergies, right?
4/
But people are eating papaya (which contains papain) or pineapple (which contains bromelain), another enzyme used for these experiments, and not many reports some allergies, right?
4/
@RMedzhitov Now, @RMedzhitov is correct to focus on enzymes b/c many known #allergens are indeed #enzymes. However, there is another problem with enzyme model 5/
@RMedzhitov allergy (as well as autoimmune diseases) are increasing in the world but #food enzymes are the same. Nothing change about them. So, how to explain the rise of allergies then?
5/
5/
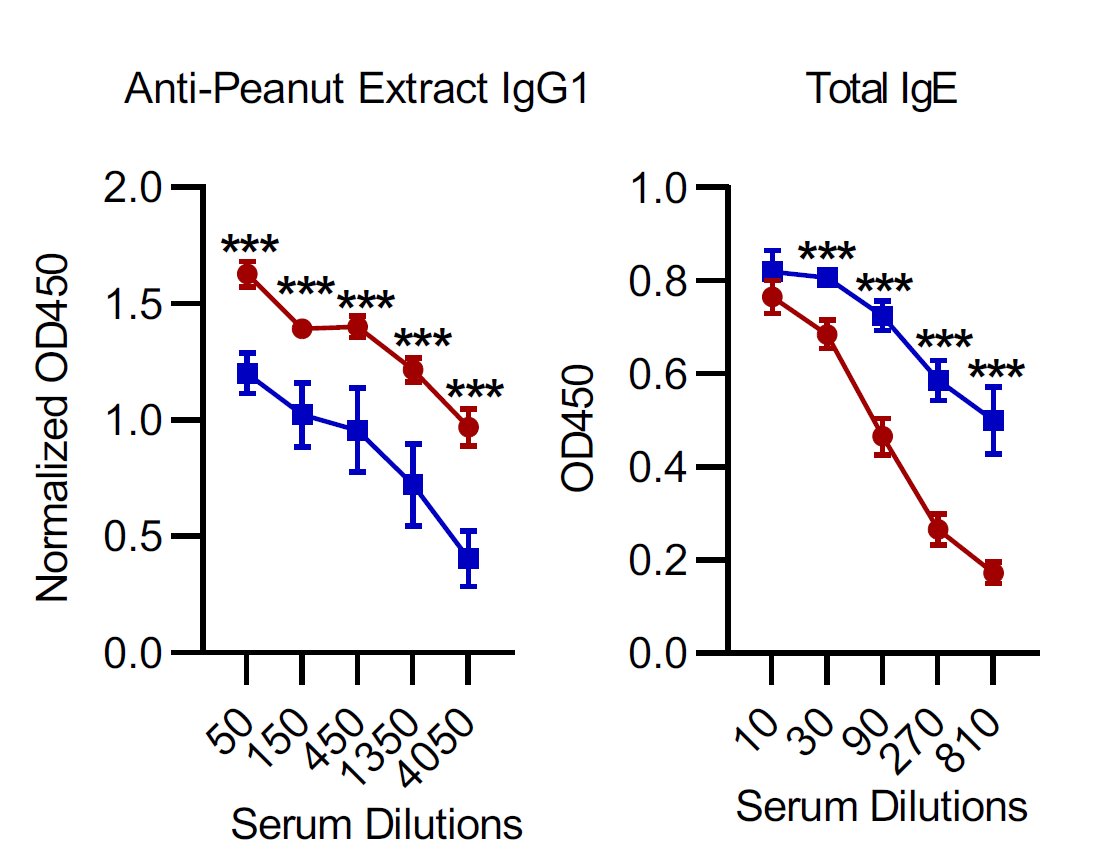
@RMedzhitov In this new paper @RMedzhitov come up with an alternative model to fit the current situation with allergies: in addition to an intrinsic property of allergenicity in some antigens, he now added that any antigens if co-occurring with some toxic substance could cause allergy
7/
7/
@RMedzhitov so, those toxic substances are all those new chemicals industries developed over the one century and are part of our daily life and food we eat. Nicely, @RMedzhitov new model can explain the rise of allergy as the consequence of the use of toxic (Th2-promoting) agents in food
8/
8/
@RMedzhitov However, even with this modification, the allergy model @RMedzhitov suggests still has the same original weakness:
most of us eat the same food and are exposed to the same toxic chemicals but far, far fewer of us getting any given #allergy.
#immunology
9/
most of us eat the same food and are exposed to the same toxic chemicals but far, far fewer of us getting any given #allergy.
#immunology
9/
@RMedzhitov I think when something is difficult to solve we need to turn to mother Nature for guidance. This is the reason why the works of @casanova_lab on natural inborn errors of immunity are so important than all mouse experiments combined
#immunology #allergy
10/
#immunology #allergy
10/
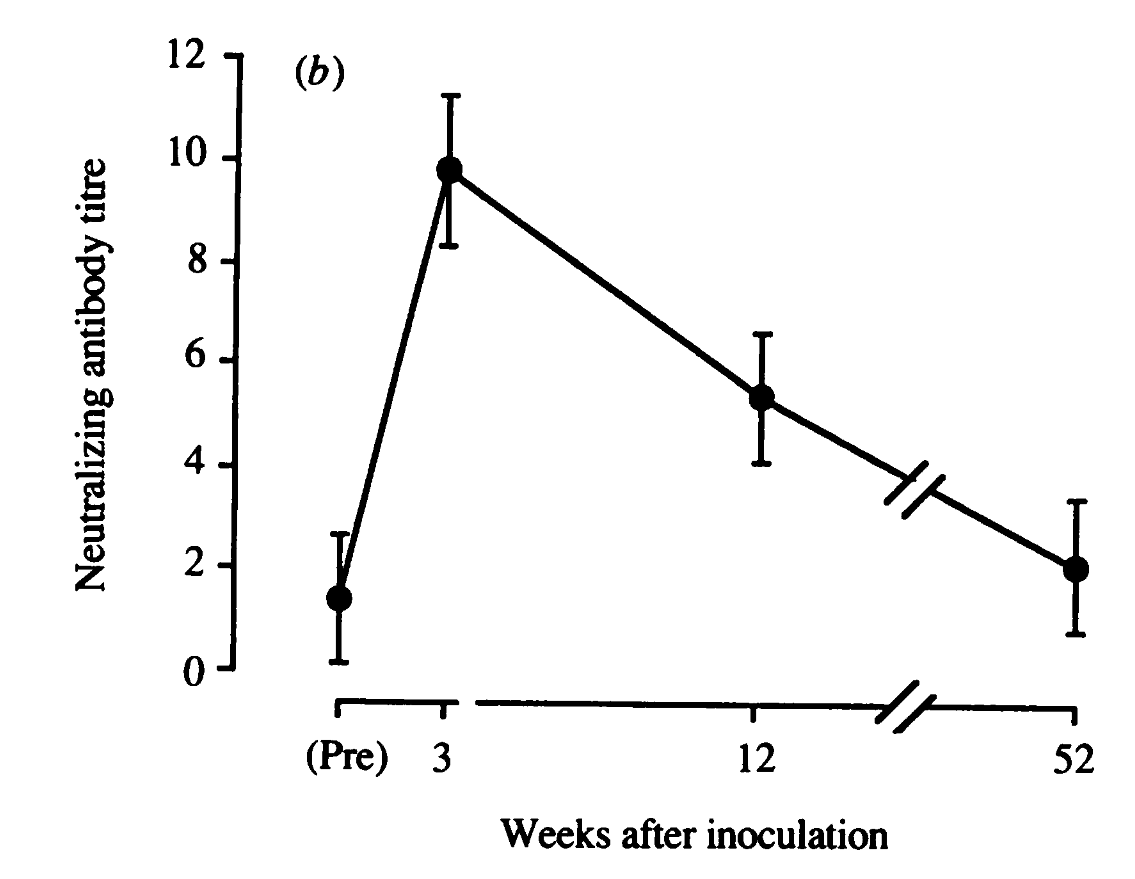
@RMedzhitov @casanova_lab and we have at least one natural experiment on allergy that shows that the way allergy develops is a completely host-specific event rather than an exogenous antigen intrinsic/toxicity mechanism
11/
11/
@RMedzhitov @casanova_lab and this natural model is a #meat #allergy that develops in some people bitten by ticks. Here we have a perfect experiment: before a tick attack, one can eat meat, no problem. After a tick attack, the same individual develops an allergy to the same meat he/she ate the whole time.
@RMedzhitov @casanova_lab what changed? meat is the same. so, intrinsic allergenicity there. in addition, meat and tick were not eaten together to create a co-occurrence of the Th2-promoting environment. Meat and tick saliva are not together, not even close and still one gets allergy.
13/
13/
@RMedzhitov @casanova_lab the model proposed by @RMedzhitov cannot explain meat allergy after a tick attack. Then what changed to develop an #allergy? The host changed, not antigen or toxic material.
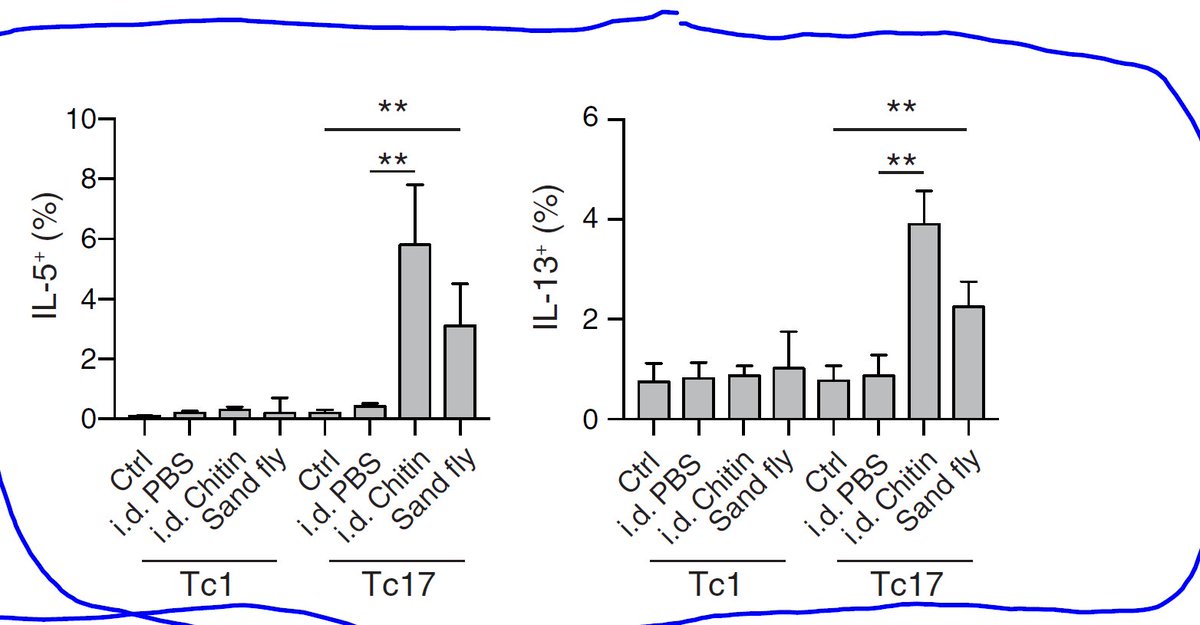
@RMedzhitov @casanova_lab tick attack modified the host by priming against its antigen. In that particular host, that priming led to the expansion of Th2 cells. Now, if HLA epitope in that host happens to display meat antigen, cross-reactive to that tick priming antigen, one gets an allergy attack. 14/
@RMedzhitov @casanova_lab the question is that why some but not tick bitten individuals getting such unusual meat allergy: first, HLA is different and a few unlucky will carry HLA combination creating cross-reactivity between meat and tick saliva.
15/
15/
@RMedzhitov @casanova_lab 2nd, the host environment does play an additional role in promoting highly polarized TH2 priming: mostly to do with microbiota alteration that produces active metabolites that keeps TH2 polarization in check. When microbiota is altered that brakes are gone too. 16/
@RMedzhitov @casanova_lab it is strange, that @RMedzhitov went in the opposite direction in his analysis of the origin of allergy rather than the host or microbiota. 17/
@RMedzhitov @casanova_lab His lab was one the first who introduced germ-free mice in immunology (recent surge) by showing that IL-2 KO GF mice were still harboring inflammation but not IL-10 KO on GF background.
In my view, specific allergies occur due to piggyback on pre-existing cross-reactive memory-like Th2 cells that are pathologically amplified in the host environment lacking microbiota/or even food-derived metabolites that ordinarily keeps them in check (more balanced)
19/
19/
Furthermore, nothing in the foreign antigen (neither intrinsic allergenicity nor association with chemicals) would allow it to initiate pathological Th2 polarization from naive T cells. Zero. Such a system cannot stand. It must be from pre-existing memory T cells.
20/
20/
@threadreaderapp unroll (lets see)
@pdfmakerapp grab this (testing)
@RMedzhitov Read full thread by @3DiMMUNE:'In this opinion paper @RMedzhitov went back to drawing board…' in single post here mythreadreader.com/3DiMMUNE/13516…
• • •
Missing some Tweet in this thread? You can try to
force a refresh