🚨Exciting results from the #RECOVERY trial #preprint of #Tocalizumab (Toci) in hospitalized people w/ #COVID19
-reduced 28-day mortality (29 vs 33%; NNT)
-decreased likelihood of requiring MV (33% vs 38%)
-shorter hospital stay (median 20 vs >28 days)
medrxiv.org/content/10.110…
1/


-reduced 28-day mortality (29 vs 33%; NNT)
-decreased likelihood of requiring MV (33% vs 38%)
-shorter hospital stay (median 20 vs >28 days)
medrxiv.org/content/10.110…
1/



They randomized 4116 pts to weight-based Toci vs usual care (UC):
-groups were balanced: mostly male (>65%), older (>60 yo), & w/ comorbidities (>55%)
-most patients (82%) also received dexamethasone
-they received Toci early in hospitalization but were 7-14 days after onset
2/


-groups were balanced: mostly male (>65%), older (>60 yo), & w/ comorbidities (>55%)
-most patients (82%) also received dexamethasone
-they received Toci early in hospitalization but were 7-14 days after onset
2/
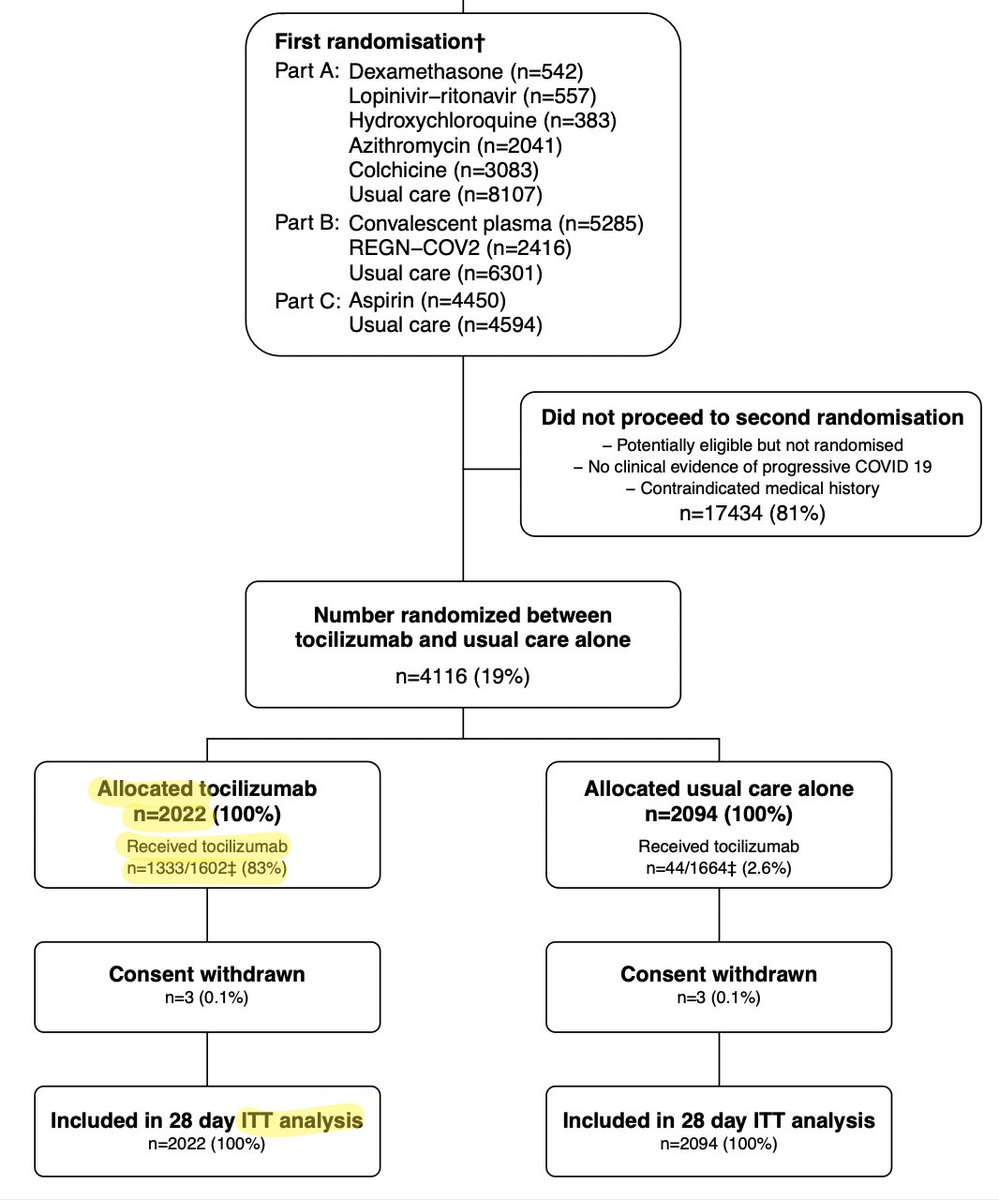


Notably, only 83% of patients in the Toci group actually received Toci (plus 2.6% randomized to the UC group got Toci); this would decrease the effect size and bias the towards null.
This means their ITT analysis is probably *underestimating* the true effect size somewhat.
3/
This means their ITT analysis is probably *underestimating* the true effect size somewhat.
3/

To their credit, despite the fact that intention-to-treat (ITT) underestimates the effect they don't waste even 1 second of my time with an "as treated analysis."
Even in the supplement. This is a mark of legit science.
Statistically speaking this is a "nothing but net" shot
4/
Even in the supplement. This is a mark of legit science.
Statistically speaking this is a "nothing but net" shot
4/
In terms of outcomes, pts randomized to Toci had clinically meaningful Δ:
-decreased 28 day mortality (29 vs 33%; NNT 25)
-lower likelihood of requiring IMV (12 vs 15%; NNT 33)
-lower likelihood of requiring RRT (5 vs 7%; NNT 50)
-shorter hospital LOS (median 20 vs 28 days)
5/

-decreased 28 day mortality (29 vs 33%; NNT 25)
-lower likelihood of requiring IMV (12 vs 15%; NNT 33)
-lower likelihood of requiring RRT (5 vs 7%; NNT 50)
-shorter hospital LOS (median 20 vs 28 days)
5/


One concern is that Toci can cause arrythmias & increase the risk of secondary infections.
Notably there was no increase in cardiac arrythmias, unexplained mortality, or infection related mortality.
This suggests that a single dose of Toci does not have major side effects.
6/

Notably there was no increase in cardiac arrythmias, unexplained mortality, or infection related mortality.
This suggests that a single dose of Toci does not have major side effects.
6/


"BuT wHaT aBoUt AlL tHe NeGaTiVe TrIaLs?"
There's definitely been a back and forth in the Tocilizumab/COVID19 literature. This is a situation where we really need to look closely at the individual studies...
(Shamelessly stole this GIF from my friend @NickJohnsonMD btw)
7/
There's definitely been a back and forth in the Tocilizumab/COVID19 literature. This is a situation where we really need to look closely at the individual studies...
(Shamelessly stole this GIF from my friend @NickJohnsonMD btw)
7/
I will do a blog post on this, but here's the quick version: These studies vary alot!
-Intervention: some gave 1 dose Toci, some ≥2
-Population: some include only ICU/MV patients, some exclude all ICU or MV patients, some gave Dex, some didn't
-Most are underpowered (n<300)
8/
-Intervention: some gave 1 dose Toci, some ≥2
-Population: some include only ICU/MV patients, some exclude all ICU or MV patients, some gave Dex, some didn't
-Most are underpowered (n<300)
8/

The authors do include a Forest plot, but their methodology seems a bit sketchy...
Specifically, they double up the control groups in a couple studies & appear to use a fixed effects model, despite reasonably high heterogeneity.
To illustrate, compare their analysis to mine:
9/


Specifically, they double up the control groups in a couple studies & appear to use a fixed effects model, despite reasonably high heterogeneity.
To illustrate, compare their analysis to mine:
9/



Overall this is a rigorously done study & analysis. I'm curious to see how this section changes in peer review.
I'm also curious to see if they do a cost-effectiveness analysis. My hypothesis would be the big reductions in IMV, RRT, and LOS would more than pay for the Toci.
10/
I'm also curious to see if they do a cost-effectiveness analysis. My hypothesis would be the big reductions in IMV, RRT, and LOS would more than pay for the Toci.
10/
🥡Takehome point: RECOVERY is a large well-done RCT that convincingly shows that #tocilizumab is beneficial given in combination w/ #dexamethasone in severe/critical #COVID19 infxn
Two large RCTs (REMAP-CAP & RECOVERY) replicate this finding. This should change our practice
11/
Two large RCTs (REMAP-CAP & RECOVERY) replicate this finding. This should change our practice
11/
To put this another way; I've gotten on and off the Toci train 🚂 over the last year, but these latest studies are compelling and make me a believer.
If I got very sick with COVID19, I would want to receive #Tocilizumab (along with #dexamethasone of course).
12/
If I got very sick with COVID19, I would want to receive #Tocilizumab (along with #dexamethasone of course).
12/
Disclosures: Sadly I receive no 💰 from the makers of Tocilzumab...
13/13
13/13
• • •
Missing some Tweet in this thread? You can try to
force a refresh