THREAD: Can #simulation be used to improve patient care? Can it impact & improve our healthcare systems?
Short answer = yes.
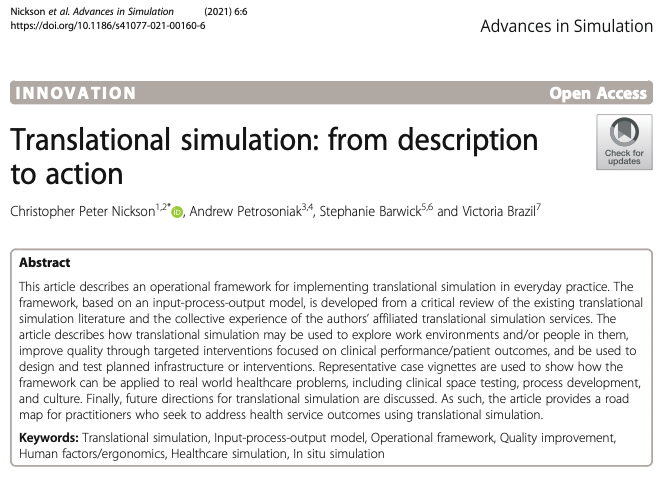
Some thoughts on the practical & operational framework we just published led by @precordialthump @InSituSteph @SocraticEM
bit.ly/3t6wivl
1/
Short answer = yes.
Some thoughts on the practical & operational framework we just published led by @precordialthump @InSituSteph @SocraticEM
bit.ly/3t6wivl
1/
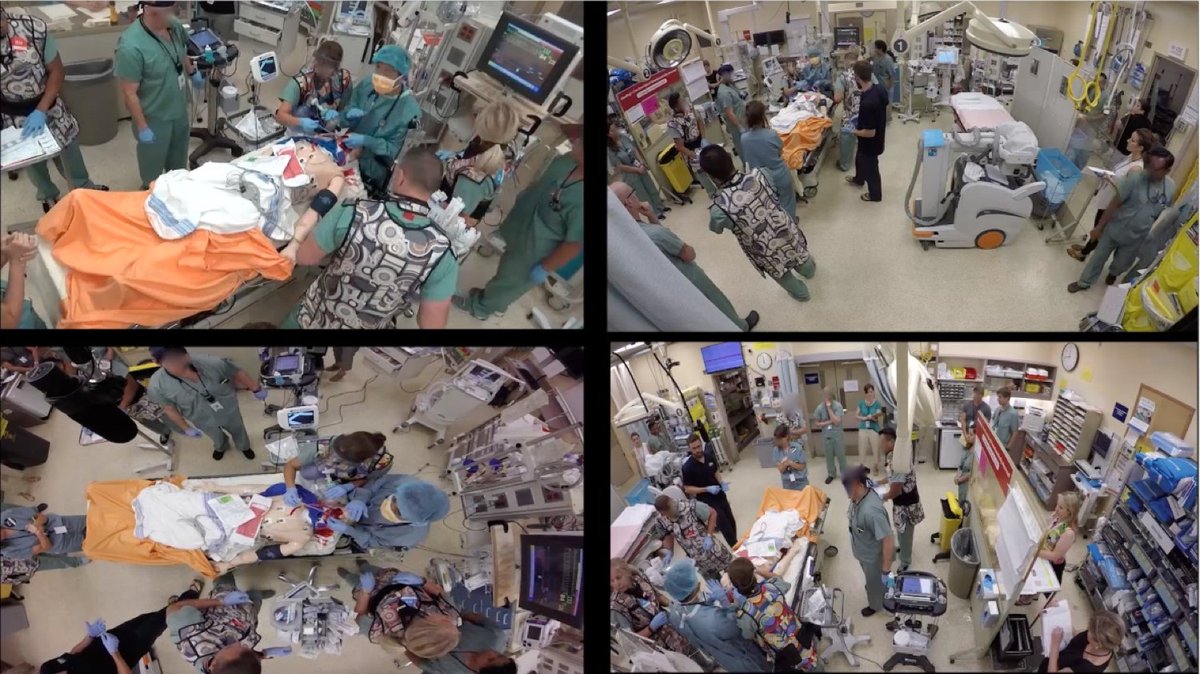
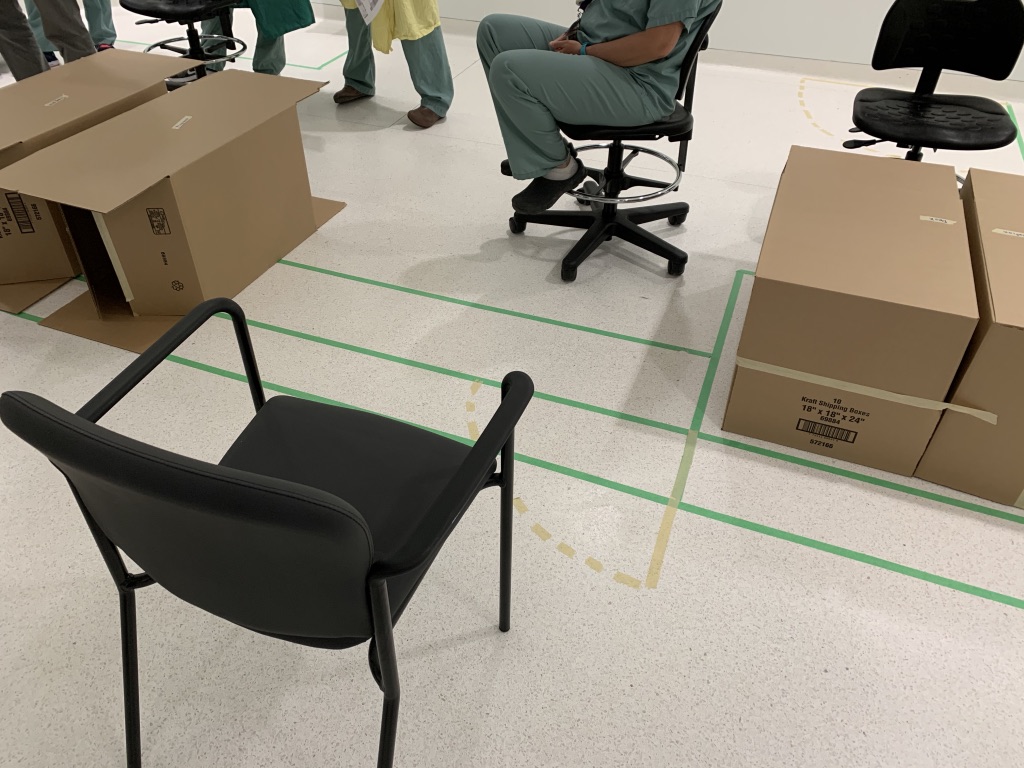
2/ Many of us have experienced it firsthand
during #COVID19 as we piloted & refined new protected intubations/code blue…but how can we make this type of sim happen?
Lots of places now using sim regularly to identify problems & improve processes...here's a bit of a guide


during #COVID19 as we piloted & refined new protected intubations/code blue…but how can we make this type of sim happen?
Lots of places now using sim regularly to identify problems & improve processes...here's a bit of a guide



3/ But first, what exactly is translational simulation? Here’s the defn from @socraticEM who first described this term.
ref: bit.ly/3t2qXFf
ref: bit.ly/3t2qXFf

4/ What’s key is that it emphasizes function of the sim…what’s it INTENDED to do…not where it occurs or how its done. E.g. in situ sim can be used as a regular training session but it becomes translational when it focuses on improving healthcare systems (or direct patient care)
5/ Briefly, translational sim has 3 broad use cases
1. Better understanding of differences between “work-as-imagined” and “work-as done” along w/ impact of team/institutional culture
2. Integration within QI initiatives to improve performance/outcomes
1. Better understanding of differences between “work-as-imagined” and “work-as done” along w/ impact of team/institutional culture
2. Integration within QI initiatives to improve performance/outcomes
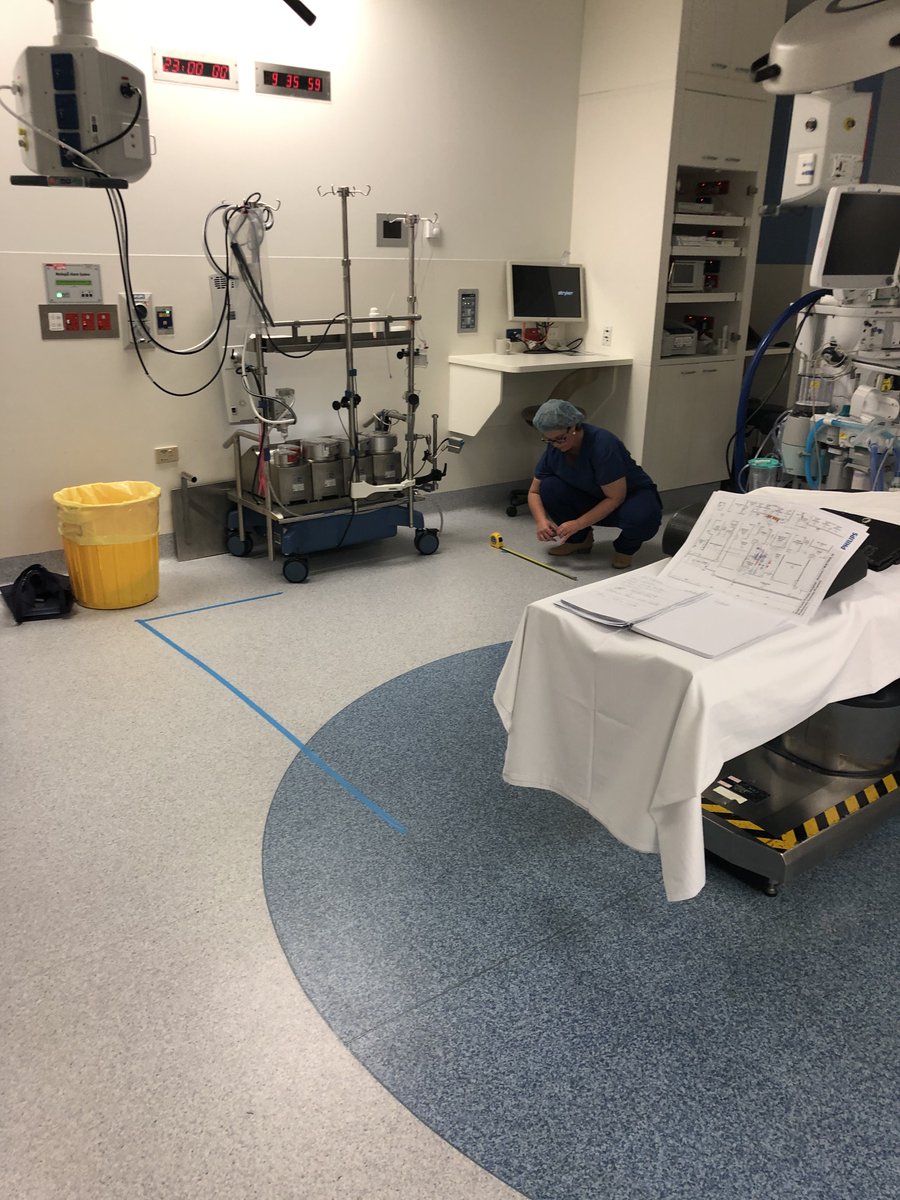
6/ And my favorite...
3. “Crash test” new spaces, equipment or processes
So if any of these 3 use cases are something you’re undertaking then strongly consider integrating translational simulation into your process…but how?
Well, we got you.


3. “Crash test” new spaces, equipment or processes
So if any of these 3 use cases are something you’re undertaking then strongly consider integrating translational simulation into your process…but how?
Well, we got you.

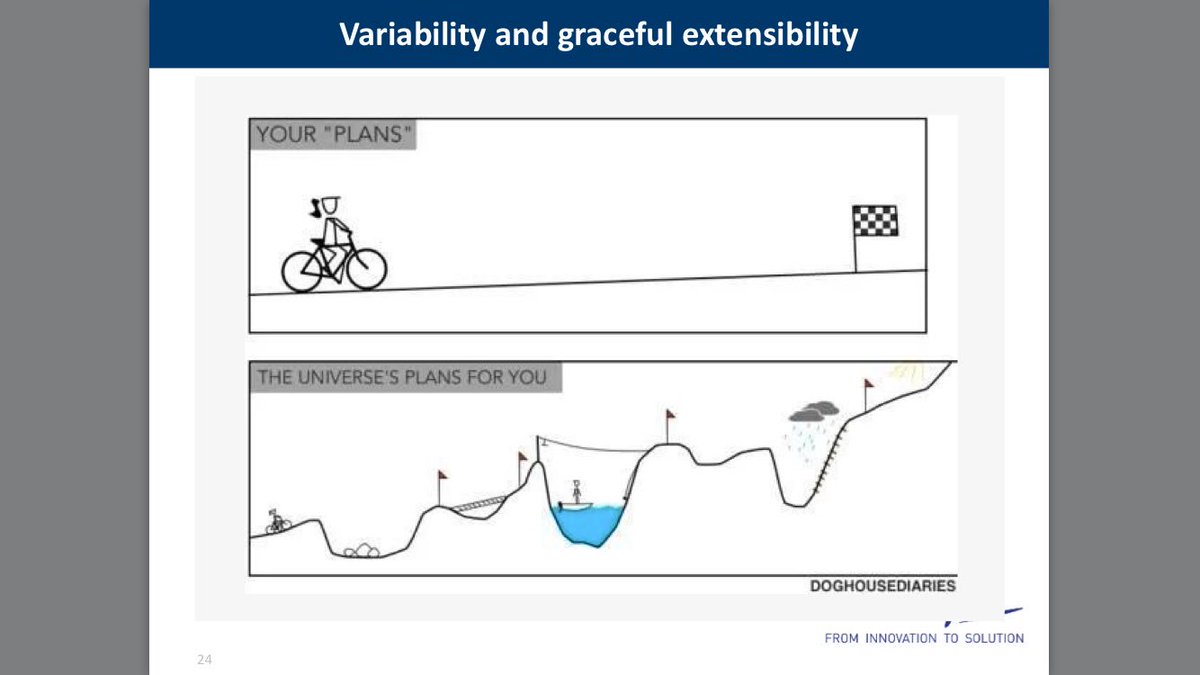
7/ We’ve applied the Input-Process-Output framework to help operationalize this. Illustrated below that I’ll describe in more detail.
Critical is that this is a non-linear (and iterative) process. You might move back/forth between input & process while figuring out the project
Critical is that this is a non-linear (and iterative) process. You might move back/forth between input & process while figuring out the project
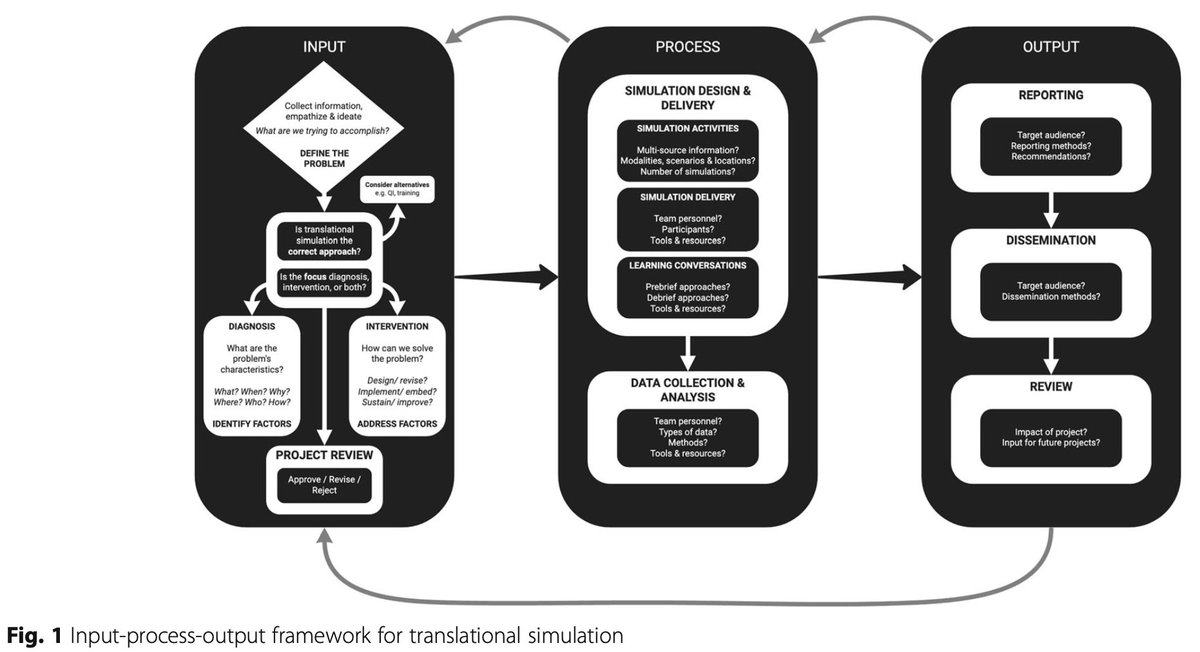
8/ INPUT: There’s nothing worse than “solving” something that isn’t actually a problem (or one that doesn't actually exist!) 
9/ Conversely defining & clarifying the problem is a critical step and can occur thru multiple ways…
- design thinking,
- participatory ergonomics,
- direct observation,
- observations during simulation…etc
- design thinking,
- participatory ergonomics,
- direct observation,
- observations during simulation…etc
10/ However the problem is defined… it has to involve people on the frontlines, patients and those in leadership roles. A participatory design process is ideal involving clinical/non-clinical team members, patients, leadership.
11/ Make sure during this process, you ask yourself if simulation is right for the job. It’s a tool and like anything when used appropriately, its very powerful, but when used incorrectly, it may not get the job done. 

12/ Also, consider whether you’re going to use simulation to “diagnose” the problem or as the “intervention” to solve the problem? Or, it might be both, which is how we used it at our institution
1) figure out problems w/ our MHP
2) to test solutions
link.springer.com/article/10.100…
1) figure out problems w/ our MHP
2) to test solutions
link.springer.com/article/10.100…
13/ There’s a list of further considerations that can/should be applied during the input phase, too much for twitter but summarized here 
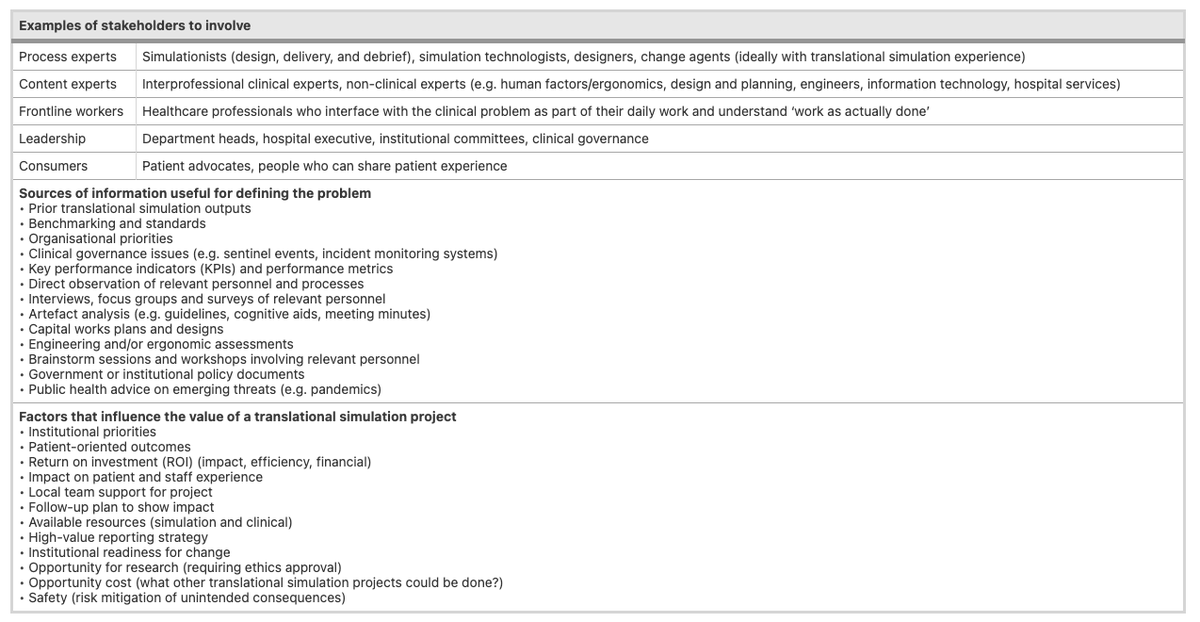
13/ PROCESS – once you’ve designed on the approach, its time to make it happen. This involves designing and delivering the session(s), collecting data and analyzing it.
14/ There’s an entire literature space emerging on systems-based or translational thinking which I recommend esp if you’re planning a session (including debriefing tools and creating psychologically safety)
Links: stel.bmj.com/content/6/3/132 & pubmed.ncbi.nlm.nih.gov/31135684/
Links: stel.bmj.com/content/6/3/132 & pubmed.ncbi.nlm.nih.gov/31135684/
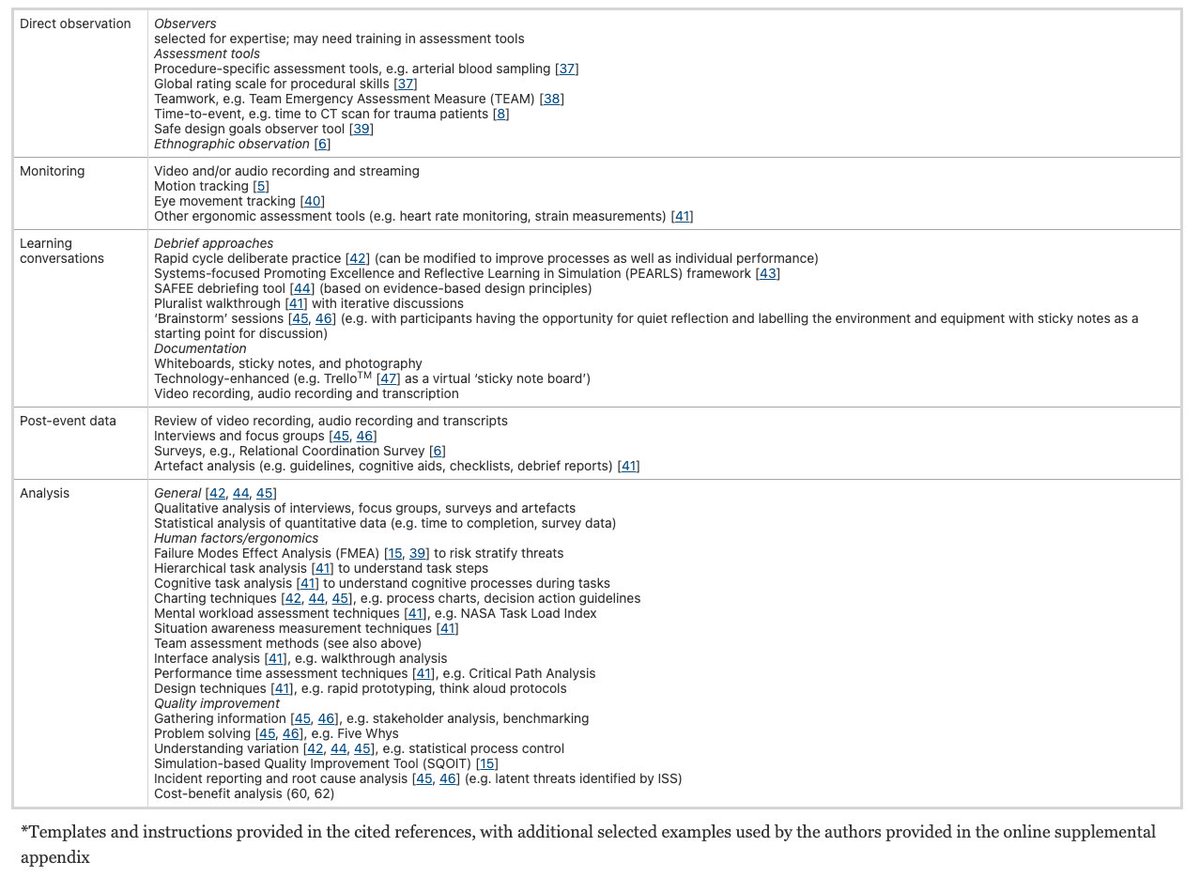
15/ The data collection often includes qualitative and quantitative elements…with a growing number of options 
16/ And these simulations should (when possible) link to existing ACTUAL datasets! Think big here! To quote @SocraticEM "its a strategy, not an event".
All those AI people, we're talking to you! Imagine regular simulations integrated and analyzable in institutional databases.
All those AI people, we're talking to you! Imagine regular simulations integrated and analyzable in institutional databases.
17/ Without the data, however whatever that looks like, its hard to demonstrate the need for change or to show proof that interventions actually work. But don’t let this be a barrier to making it happen either. The data doesn’t need to be worthy of publication...
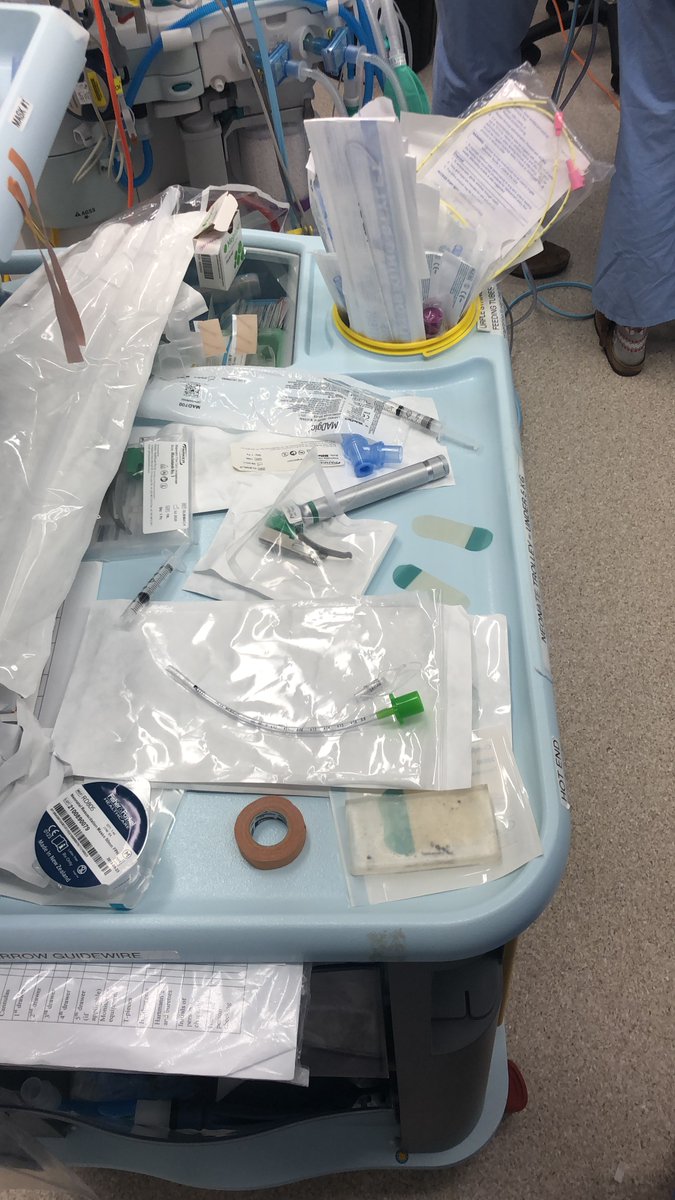
18/ Maybe all you needed to show was feedback from multiple team members that the “Covid intubation box” is non functional in your clinical environment.
…-publications.onlinelibrary.wiley.com/doi/full/10.11… &
pubmed.ncbi.nlm.nih.gov/32397008/
…-publications.onlinelibrary.wiley.com/doi/full/10.11… &
pubmed.ncbi.nlm.nih.gov/32397008/
19/ OUTPUT: Once you’ve run the simulations, collected & analyzed your data, its time to share it! This might be within your institution or more outward facing initiatives (e.g. publications).
20/ Practically, pictures or video clips from simulations are highly useful and (I think) under utilized. We regularly include them in our reports and its far more impactful than any words on the page. 




21/ In my opinion, the future of translational simulation lies in how we articulate the return on investment. Maybe its as straightforward as saving the institution money? But let’s think outside the box?
22/ If it takes 100 people hours to make a typical high stakes decision in a hospital, maybe translational simulation can help you do that in only 20 people hours (e.g. 2hr simulation with 10 people…clearly highlighting the likely issue or answer).
23/ Some would suggest that simulation should be mandatory when designing hospitals or healthcare spaces publish.csiro.au/AH/AH19114 by @InSituSteph
ping @AdvPerformHD @HumanFact0rz @NORR_AEP
ping @AdvPerformHD @HumanFact0rz @NORR_AEP
24/ This is when it gets really interesting, when we think about translational simulation as an advanced decision making tool. How can it be used to make better decisions, more frequently and with greater certainty. That’s when the impact gains traction. 

25/ If you can reliably, accurately and repeatedly predict patient harms before they happen? Well that’s pretty epic.
And if translational simulation can be fully integrated into hospital/healthcare systems...well, that's the future!
And if translational simulation can be fully integrated into hospital/healthcare systems...well, that's the future!
26/ There you have it. Some reflections on this paper and how translational simulation can be operationalized…moving beyond theory and into practice.
I just happen author this...but many of these ideas from @precordialthump @SocraticEM @InSituSteph
I just happen author this...but many of these ideas from @precordialthump @SocraticEM @InSituSteph
• • •
Missing some Tweet in this thread? You can try to
force a refresh