Ready for a quick and easy tutorial on how to develop a #strength training treatment plan for your patients - such as those for #EMST, #CTAR, #IOPI? 💪🙋♂️ Check out the below thread along with an accompanying example using #expiratory #muscle #strength training #EMST 

First, measure the patient’s 1-repetition maximum (RM) by determining where they "max" out on a resistance-based exercise💪📈
Second, determine the desired strength training intensity level (i.e., low, moderate, high). For most of our elderly and/or rehab patients, we will use moderate intensity. For neuromuscular diseases (e.g., #ALS), current research suggests to consider a low intensity exercise.
Third, refer to the below table (see reference for more information) to guide how you may consider structuring the intensity of each repetition, the number of repetitions and sets, the length of rest, and the frequency of a strength training treatment. 

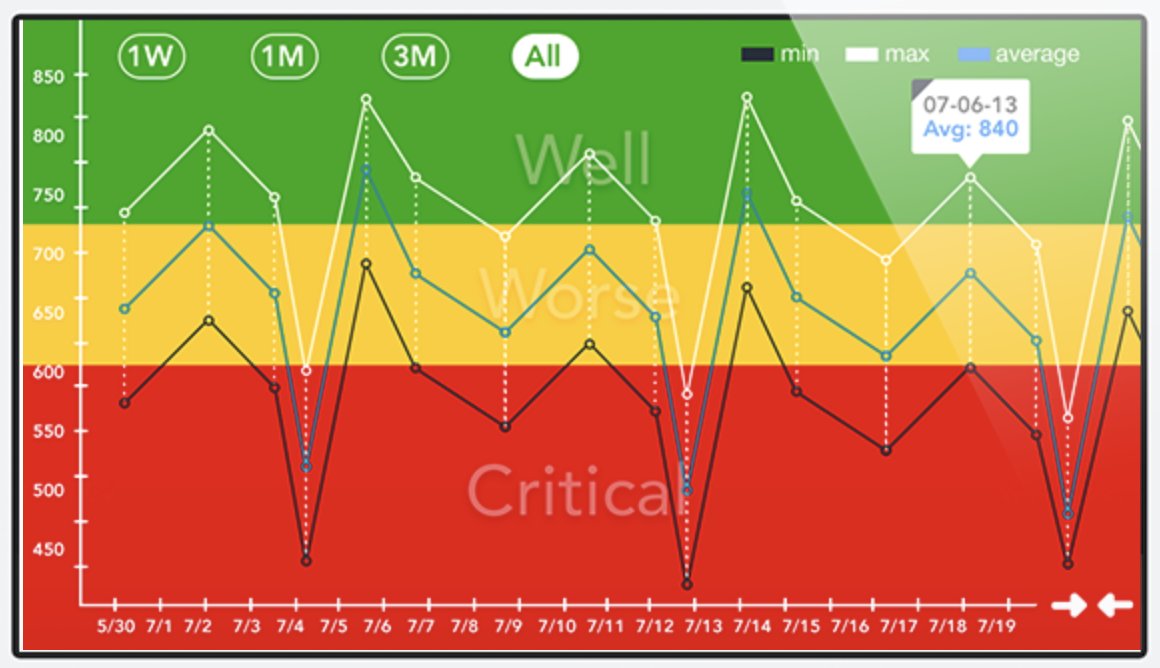
Lastly, re-assess the 1-RM every week to ensure you are maintaining the appropriate intensity level. See below for example of how I may structure a strength training protocol using Expiratory Muscle Strength Training (#EMST)
First, measure the 1-RM using the #EMST #EMST150 device. In this video, I work my way up the resistance levels from 30, to 60, to 90, to 120. I eventually max out at ~150 cmH20. So my 1-RM is 150 (or rather, just below 150).
Second, determine the intensity level for #EMST. I chose to demonstrate moderate intensity since I work with many people with #Parkinson’s disease (#PD) and this is the intensity level I often recommend for them.
Moderate intensity involves practicing each repetition at ~70% RM. 70% of 150 is ~100. So, this means I should practice at ~100 cmH20. Moderate intensity also means practicing ~10 repetitions/set, 2-3 minutes of rest/set, 2-4 sets/session, 2-3 days per week.
Re-assess strength every week 📈📊, and re-adjust intensity level to maintain the 70% RM target as strength begins to increase!💪🥳 See my previous tutorial on #CTAR to see how this applies to that exercise as well!
https://twitter.com/JamesCurtisSLP/status/1205938569908498433
Garber, C. E., et al., (2011). Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. journals.lww.com/acsm-msse/Full…
• • •
Missing some Tweet in this thread? You can try to
force a refresh