1/4
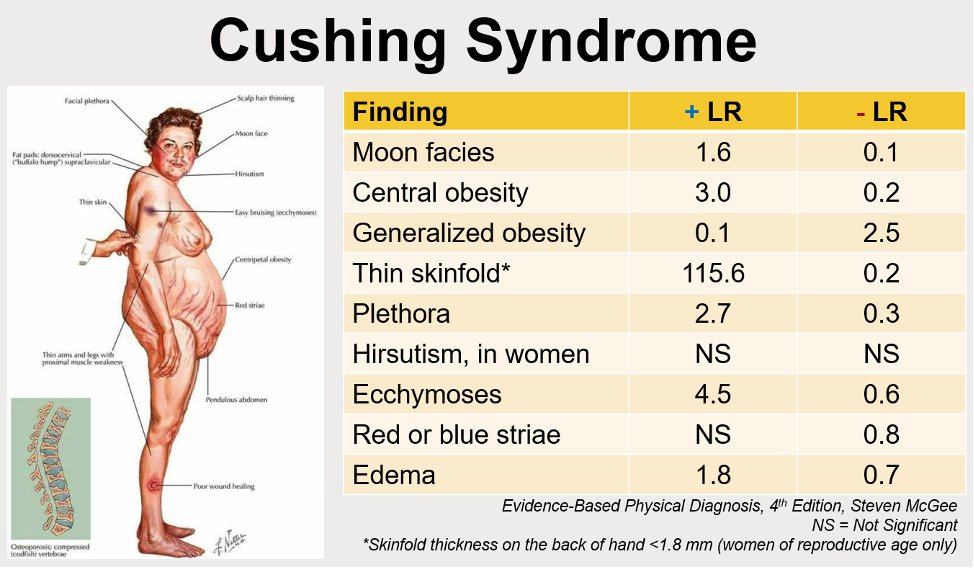
Let's review the evidence-based physical exam for Cushing syndrome!
Quick review of LRs:
- The (+) and (-) indicate the LR if a finding is present or absent, respectively
- The more the LR deviates from 1, the more useful it is
#MedTwitter #MedEd #EndoTwitter #FOAMed
Let's review the evidence-based physical exam for Cushing syndrome!
Quick review of LRs:
- The (+) and (-) indicate the LR if a finding is present or absent, respectively
- The more the LR deviates from 1, the more useful it is
#MedTwitter #MedEd #EndoTwitter #FOAMed
2/4
Things that stand out to me
- "Buffalo hump" doesn't have a defined LRs despite being taught as a "classic" finding (occurs in 34-75% of patients)
- The presence of moon facies has a lower LR than I expected (1.6)
Things that stand out to me
- "Buffalo hump" doesn't have a defined LRs despite being taught as a "classic" finding (occurs in 34-75% of patients)
- The presence of moon facies has a lower LR than I expected (1.6)
3/4
- The absence (or presence) of abdominal striae is not particularly helpful
- The presence of a thin skinfold (thickness on the back of the hand <1.8 mm in women of reproductive age) can be VERY telling
- The absence (or presence) of abdominal striae is not particularly helpful
- The presence of a thin skinfold (thickness on the back of the hand <1.8 mm in women of reproductive age) can be VERY telling
4/4
Those who are interested in seeing clinical images should check out the following link on Physical Diagnosis PDX! physicaldiagnosispdx.com/endocrinology-…
Those who are interested in seeing clinical images should check out the following link on Physical Diagnosis PDX! physicaldiagnosispdx.com/endocrinology-…

• • •
Missing some Tweet in this thread? You can try to
force a refresh