1/7 Let’s go over the evidence-based physical exam for lower extremity deep vein thrombosis (LE DVT). In the spirit of quantifying clinical concern, here is a question - besides inspection (and #POCUS), which tool will help you the most?
#MedTwitter #FOAMed #MedEd
#MedTwitter #FOAMed #MedEd
2/7 The answer is a ruler! Let’s look at the LRs.
Quick review of LRs:
- The (+) and (-) indicate the LR if a finding is present or absent, respectively
- The more the LR deviates from 1, the more useful it is
Quick review of LRs:
- The (+) and (-) indicate the LR if a finding is present or absent, respectively
- The more the LR deviates from 1, the more useful it is

3/7 For this particular set of exam findings, it may be more helpful to see how much the LRs change your post-test probability (assuming a pre-test probability of 50%). The presence of absence of asymmetric calf swelling seems to be the most helpful.
Graphic from McGee
Graphic from McGee
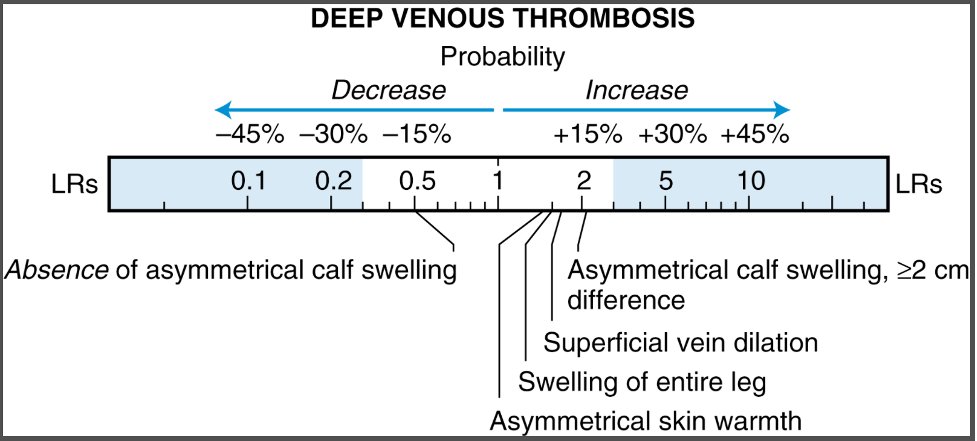
4/7 The change in probability for the presence of absence of these findings is not great (they are all close to 1). Ultimately, your history (and that ruler) are going to help the most to decide whether or not you need to do a lower extremity ultrasound to assess for LE DVT.
5/7 An often-used calculator is the Well’s score, which stratifies patients into pre-test probability of LE DVT.
2 things worth noting:
1⃣Meant for outpatient diagnosis
2⃣Up to 2 points go into the clinician deciding if an alternative diagnosis to DVT is likely or more likely.
2 things worth noting:
1⃣Meant for outpatient diagnosis
2⃣Up to 2 points go into the clinician deciding if an alternative diagnosis to DVT is likely or more likely.
6/7 Here is another way to see how your probability changes (assuming a pre-test probability of 50%). The impact of the 2 points going into “clinical gestalt” is tremendous (you can go from low to intermediate pre-test or from intermediate to high pre-test) 

7/7 We RARELY use clinical calculators when our pre-test probability is intermediate (something is making you invoke the use of the calculator, right?). The LRs are still helpful and you can use a calculator like this to quantify your suspicion: sample-size.net/post-probabili…
• • •
Missing some Tweet in this thread? You can try to
force a refresh