Now we get to another area of particular interest for me: circadian rhythms and #fatigue. Elizabeth Klerman presenting. (1/5) #sleep 
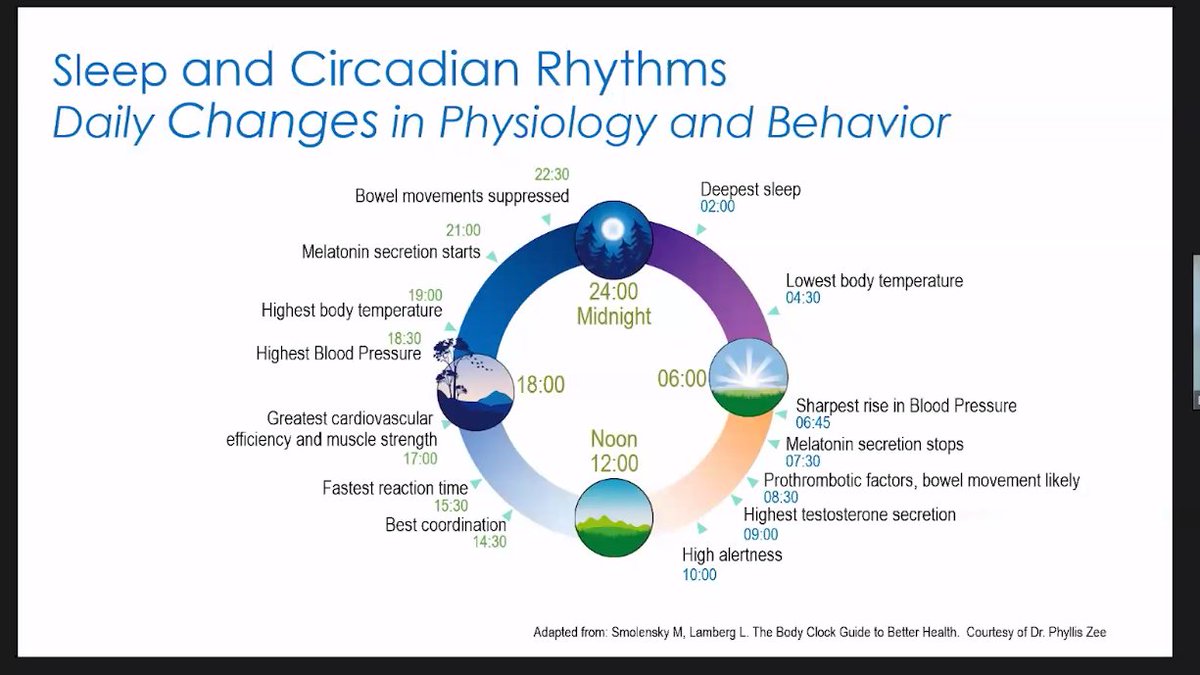
How does sleep/circadian rhythms affect various body systems and ultimate effects?
First I've heard of health disparities, here; well done, Klerman. #fatigue #sleep
First I've heard of health disparities, here; well done, Klerman. #fatigue #sleep

Circadian rhythms WILL affect results in studies. Researchers, take note!
Record time of events, blood draws, etc.!
Include sleep metrics in subjects!
Circadian =/ diurnal.
Most studies that say they're talking about circadian rhythms are actually referencing diurnal rhythms.
Record time of events, blood draws, etc.!
Include sleep metrics in subjects!
Circadian =/ diurnal.
Most studies that say they're talking about circadian rhythms are actually referencing diurnal rhythms.

Unfortunately, most of this is about HCs, rather than people who experience pathological fatigue. But the notes for researchers are truly important for researchers in the #LongCOVID & #MECFS space. #fatigue #sleep 

Finally, just as in that one actimeter study that showed you really can't ask people "how active were you?" and expect it to correlate, you can't expect people's reported sleepiness to correlate to their sleep patterns. You need objective data! #fatigue #sleep #studydesign
Want to see the rest of the talks at this conference? Go here:
https://twitter.com/exceedhergrasp1/status/1442524343221698560.
• • •
Missing some Tweet in this thread? You can try to
force a refresh