LFD studies are not great (small n, high bias, heterogeneity), but all the studies do suggest that the LFD is a good treatment option for #IBS and can improve global symptoms, pain, and bloating 

App-based low-FODMAP #diet was found to be more effective (71%) than antispasmodic therapy (61%) in #IBS, even 6 months out 

⚠️Remember that the LFD is a 3⃣ phase diet (elimination, reintroduction, personalization).
⚠️ If phase 1⃣ isn't working, then STOP the #diet; don't leave these patients on a therapy that isn't working for them!
⚠️ If phase 1⃣ isn't working, then STOP the #diet; don't leave these patients on a therapy that isn't working for them!
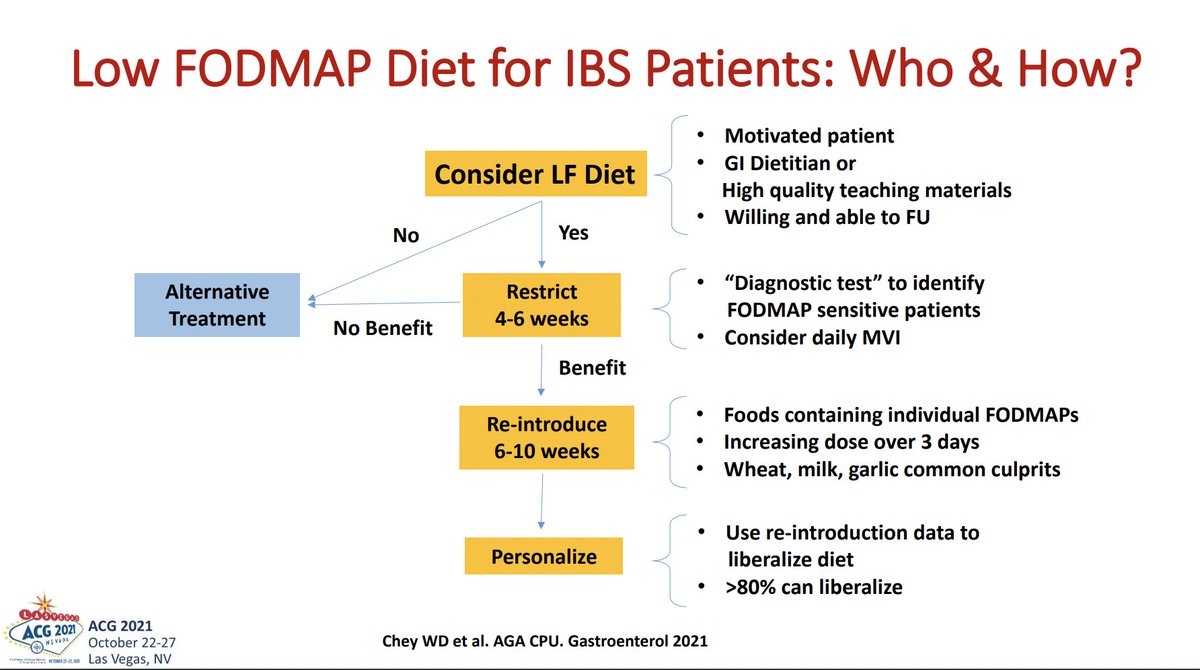
🤔 Do we really have to do the full out LFD, or can we go with a FODMAP-lite approach?
🔹fructans, galactans, and mannitol may disproportionately drive symptoms in #IBS
🔹fructans, galactans, and mannitol may disproportionately drive symptoms in #IBS

Durable long term clinical response to low-FODMAP #diet. >75% do end up on less restrictive personalized diet (as they should be!) 

About 50% of #IBS patients respond to LFD. But that means 50% don't. Can we predict who may not respond? 

Gene variants for sucrase-isomaltase deficiency are less likely to respond to low-FODMAP diet (which does not exclude sucrose)
⚠️ In patients with meal related #IBS symptoms who do not respond to LFD, consider the diagnosis of SID
⚠️ In patients with meal related #IBS symptoms who do not respond to LFD, consider the diagnosis of SID

The #Mediterranean #diet ⬇️ cardiometabolic risk, and this is mediated by the #microbiome.
MD ⬆️ SCFAs and improves bile acid metabolism
MD may be as effective as LFD. It also seems to. be preferred by #IBS patients!
More research needed!



MD ⬆️ SCFAs and improves bile acid metabolism
MD may be as effective as LFD. It also seems to. be preferred by #IBS patients!
More research needed!




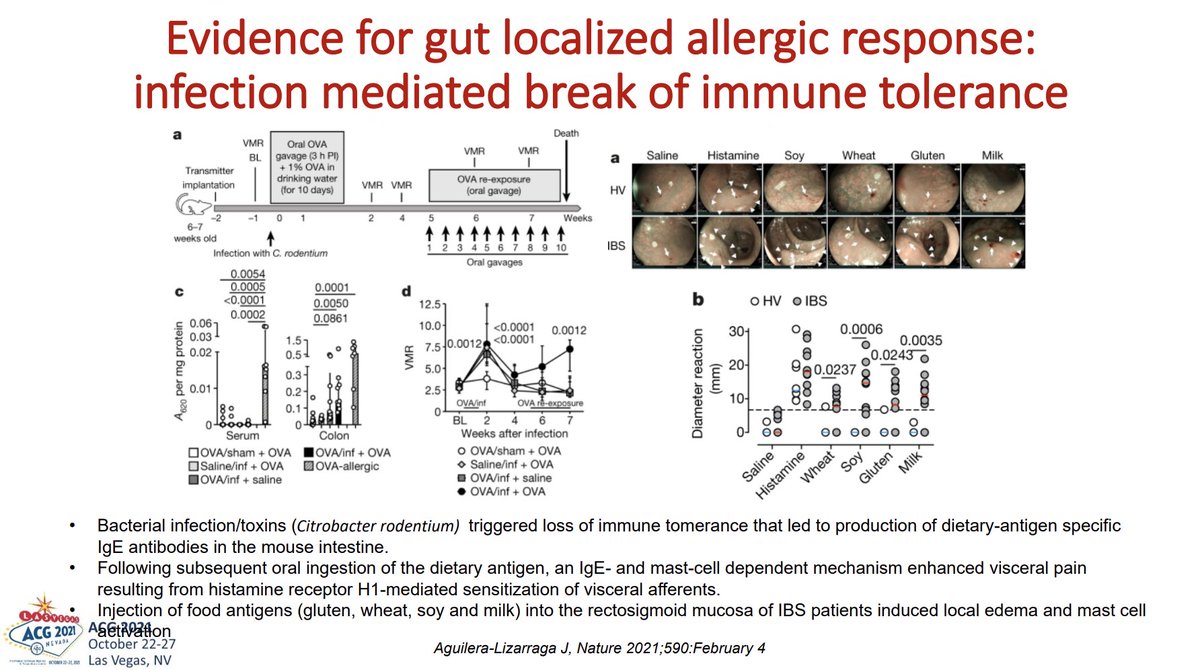
2/3 of #IBS patients have mucosal injury when exposed to certain food antigens (milk, wheat, yeast, soy). Elimination #diet based on CLE had significant symptom improvement. 

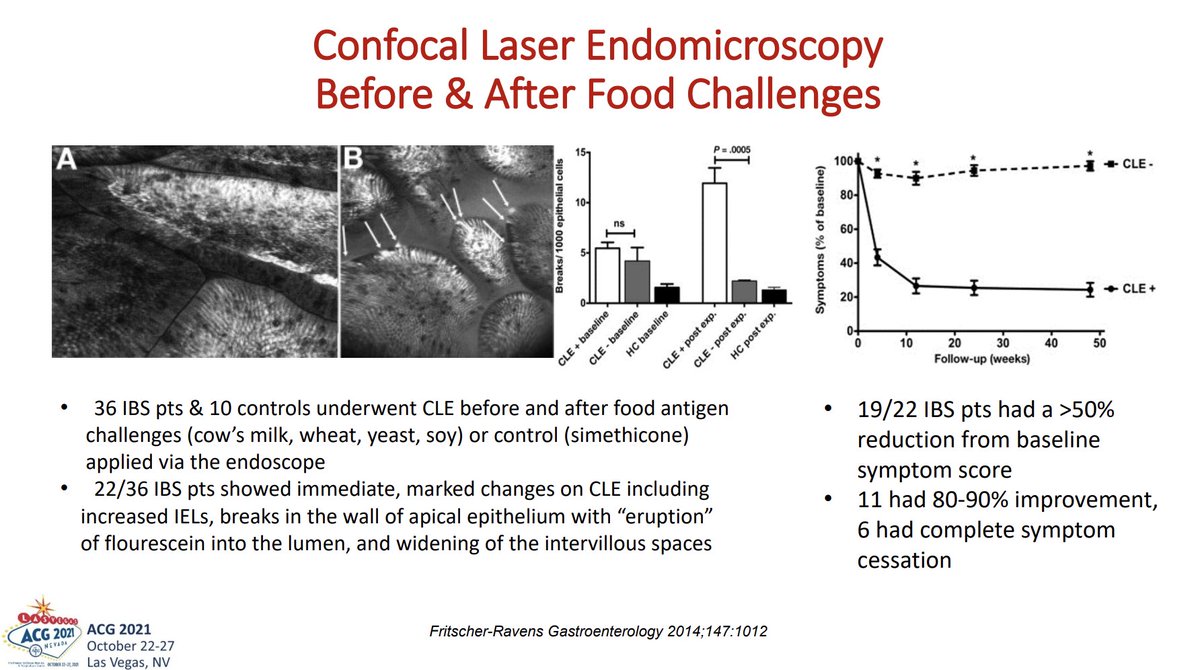

Enteric infection may break mucosal immune tolerance. Dietary antigens may then cause inflammation, leading to visceral hypersensitivity. Injecting food antigens into rectosigmoid of #IBS patients causes edema and mast cell degranulation 
• • •
Missing some Tweet in this thread? You can try to
force a refresh