1a) Welcome to a new #accredited #tweetorial on a very challenging topic: managing #ICH in a patient taking anti-FXa #DOACs! Your expert authors are both #neurointensivists: Richard Choi, DO @rkchoi @christianacare and Casey Albin, MD @caseyalbin @EmoryNeuroCrit 



1b) #Physicians #Nurses #Pharmacists #physicianassociate #NPs earn 0.5h CE/#CME from @academiccme for following this 🧵 

2) This program is supported by an educational grant from AstraZeneca and is intended for #HCPs. Accreditation statement and faculty disclosures at cardiometabolic-ce.com/disclosures/. Prior (& future) programs in this space, available for 🆓CE/#CME credit, at cardiometabolic-ce.com/category/antit….
3) And we start with a case . . . 79♂️ with HTN, Afib on #apixaban, HLD, #DM, in his usual state of health til this am. He develops headache, L-sided weakness. His wife calls EMS. He presents to ED as a pre-🏥 stroke alert. Initial VS 213/110, HR 78, RR 13, satting 100% on NRB.
4a) On exam, he is drowsy, his ❤ is irregularly irregular, 🫁 are coarse on the right side. Neurologically, he is AOX3, dysarthric, can follow commands, name and repeat. He has a left CNVII droop 🤨 with normal sensation and left hemiparesis, 2/5, with intact sensation.
4b) His #NIHSS (mdcalc.com/calc/715/nih-s…) is a 7. He undergoes a #CT which demonstrates the following: 

5) Which of the following takes precedence in this case?
A - Reverse anticoagulation
B - Lower blood pressure
C - Intubate to secure airway
D - Check temperature
A - Reverse anticoagulation
B - Lower blood pressure
C - Intubate to secure airway
D - Check temperature
6) In the acute setting, the focus is always on
A--Airway protection (💨 )
B--Bleeding: here, anticoagulation reversal (🩸🤚)
C--Circ: here, lowering the blood pressure (👇BP)
Fortunately, the patient has a GCS 15. Our focus then is initially on B&C
A--Airway protection (💨 )
B--Bleeding: here, anticoagulation reversal (🩸🤚)
C--Circ: here, lowering the blood pressure (👇BP)
Fortunately, the patient has a GCS 15. Our focus then is initially on B&C
7) What about D (disability--🧠)? Maintenance of homeostasis is also critical! Including
🤒Normothermia
🍬Normoglycemia
💨Normocapnia and oxygenation
Continue frequent neurological assessments, preferably in a Neuro ICU
For full guidelines, see: ahajournals.org/doi/10.1161/ST…
🤒Normothermia
🍬Normoglycemia
💨Normocapnia and oxygenation
Continue frequent neurological assessments, preferably in a Neuro ICU
For full guidelines, see: ahajournals.org/doi/10.1161/ST…
8) The newest spontaneous ICH #sICH guidelines place focus on
1⃣ Organizing systems of care to rapidly triage pts w/ #sICH
2⃣ Preventing secondary injury
3⃣ Understanding underlying etiology with a focus on the small vessel disease that results in many ICH cases.
1⃣ Organizing systems of care to rapidly triage pts w/ #sICH
2⃣ Preventing secondary injury
3⃣ Understanding underlying etiology with a focus on the small vessel disease that results in many ICH cases.

9) To prevent secondary injury, it is critical to appreciate which patients may be at high risk of #HematomExpansion. Several features evident on non-contrast CT imaging have been associated with hematoma expansion. See 
https://twitter.com/neurocritcarej/status/1409859200885444617?s=42&t=9O0CB6V1azKIx4jt9NKMIw

10) Additionally, the CT #angiogram can provide valuable information by ruling out large vessel etiologies (#aneurysm, #AVM) or by identifying a #spot_sign, another marker than may portend early hemorrhage expansion.
See pubmed.ncbi.nlm.nih.gov/23859836/
See pubmed.ncbi.nlm.nih.gov/23859836/

11a) With #sICH confirmed, the focus shifts to #BP management and anticoagulant reversal.
1️⃣ BP control:
✨Cerebral perfusion pressure (CPP) = MAP – ICP ✨
Historically there was a concern that lowering BP might worsen 🧠 ischemia by perfusion to the peri-hematomal tissue.
1️⃣ BP control:
✨Cerebral perfusion pressure (CPP) = MAP – ICP ✨
Historically there was a concern that lowering BP might worsen 🧠 ischemia by perfusion to the peri-hematomal tissue.
11b) However, even though acute perihematomal oligemia was demonstrated using #MRI and #CTP, we also learned from #PET and nuclear studies that this oligemia reverses thanks to #autoregulation.
👉n.neurology.org/content/57/1/1…
👉n.neurology.org/content/53/9/2…
👉🔓ahajournals.org/doi/10.1161/01…
👉n.neurology.org/content/57/1/1…
👉n.neurology.org/content/53/9/2…
👉🔓ahajournals.org/doi/10.1161/01…

12) OK, so then what are the benefits of lowering the #bloodpressure?
🧠 ⬇ risk of hematoma expansion
🧠 ⬇ risk of peri-hematomal edema.
🧠 No causation proven, but patients with higher BP historically had worse outcomes and mortality.
🧠 ⬇ risk of hematoma expansion
🧠 ⬇ risk of peri-hematomal edema.
🧠 No causation proven, but patients with higher BP historically had worse outcomes and mortality.
13) If these benefits outweigh potential risks of acute BP lowering, then what target should we aim for?
14) Enter #INTERACT2 & #ATACH_2 – two large, randomized trials assessing the benefit of acute intensive #BP lowering in patients with hypertensive #ICH:
🧠 pubmed.ncbi.nlm.nih.gov/27276234/
🧠 pubmed.ncbi.nlm.nih.gov/23713578/
🧠 pubmed.ncbi.nlm.nih.gov/27276234/
🧠 pubmed.ncbi.nlm.nih.gov/23713578/

15) If these two trials tested the same thing, why were the differences so disparate? Well, if you compare the actual BP’s between the 2⃣ trials, it’s almost as if 3⃣ groups existed:
👉the INTERACT control
👉the INTERACT intervention/ATACH control
👉the ATACH intervention:
👉the INTERACT control
👉the INTERACT intervention/ATACH control
👉the ATACH intervention:

16) It appears that #BP with outcomes in #ICH is a U-shaped curve, with optimal outcomes at a SBP range 130-150. This is the current recommendation from the most recent guidelines. See 🔓pubmed.ncbi.nlm.nih.gov/35579034/ : 



17) ⚠ Remember individual patient characteristics take preference & there can be no blanket treatment for all. If someone has truly ⬆️ICP (massive hemorrhage, cerebellar hemorrhage with hydro) & is in extremis, acute BP ⬇️may still lead to 🧠⤵️perfusion & make things worse. ⚠
18) ⚠ Also remember that this only applies to patients presenting with SBP <220. If they present with BP >220, consider a higher goal for these patients ⚠
19) Similarly, aggressively lowering the #BP too fast and too hard can also lead to worsened outcomes as demonstrated in an #ATACH sub-study: (🔓ahajournals.org/doi/10.1161/ST… ) 

20) So now we have our 🎯. How do we get there? 🤔
A. IV pushes
B. #Nitropaste
C. #Nicardipine gtt
D. Anything, but with an a-line
A. IV pushes
B. #Nitropaste
C. #Nicardipine gtt
D. Anything, but with an a-line
21) While an #INTERACT pre-planned analysis demonstrated that patients with less #BP variability had better outcomes (pubmed.ncbi.nlm.nih.gov/31397290/), we still don’t know what agents are best (gtt vs. IV push) but the goal is limiting variability🏆. 

22) Recap:
1️⃣ Acute #BP lowering may help to reduce perihematomal edema, #hematoma_expansion & possibly improve outcomes
2️⃣ The goal should be 130-150mmHg unless concerns exist for ⬆️ ICP or presenting SBP >220mmHg
1️⃣ Acute #BP lowering may help to reduce perihematomal edema, #hematoma_expansion & possibly improve outcomes
2️⃣ The goal should be 130-150mmHg unless concerns exist for ⬆️ ICP or presenting SBP >220mmHg
23) Remember B (bleeding) back in our ABCD priorities for this pt? We must move on to #anticoagulation reversal. He takes apixaban! Remember Factor Xa Inhibitors (FXa 🛑) act by binding to the active site of FXa, thus preventing the conversion of #prothrombin to #thrombin: 

24) So how do we reverse the effects of this FXa🛑?
25) Mark your response and RETURN TOMORROW for the correct answer, more education and your link to 🆓CE/#CME! 👋@stephanamayer @CritCareMed @alimkakeng @MiddeldorpS @connors_md @walinjom @CDernigo @MicieliA_MD @MayaHolsen @johnfanikos @beaverspharmd @SnayCardsPharmD
26a) WELCOME BACK! You are learning about the management of #ICH in the #DOAC-#anticoagulated pt, from expert #neurointensivists @rkchoi from @christianacare & @caseyalbin from @EmoryNeuroCrit. 🆓0.5h CE/#CME at the end of this 🧵!
#FOAMed #neurotwitter @MedTweetorials
#FOAMed #neurotwitter @MedTweetorials
26b) So did you answer the question in tweet 24 above? If not, scroll back ⤴️and commit!
27) You get credit for either B or C. Because FXa🛑 are largely protein bound, dialysis is not a feasible means of removal from the blood stream. Dabigatran, however, can be successfully dialyzed & this was common prior to the introduction of #idarucizumab in 2015.
28) aPCC/4F-PCC contain coagulation factors and likely increase thrombin generation through the replenishment of these factors, but do not change FXa activity.
👉4F-#PCC (KCentra specifically) is dosed at 25-50 units/Kg (up to 100kg; max dose = 5000 units)
👉4F-#PCC (KCentra specifically) is dosed at 25-50 units/Kg (up to 100kg; max dose = 5000 units)
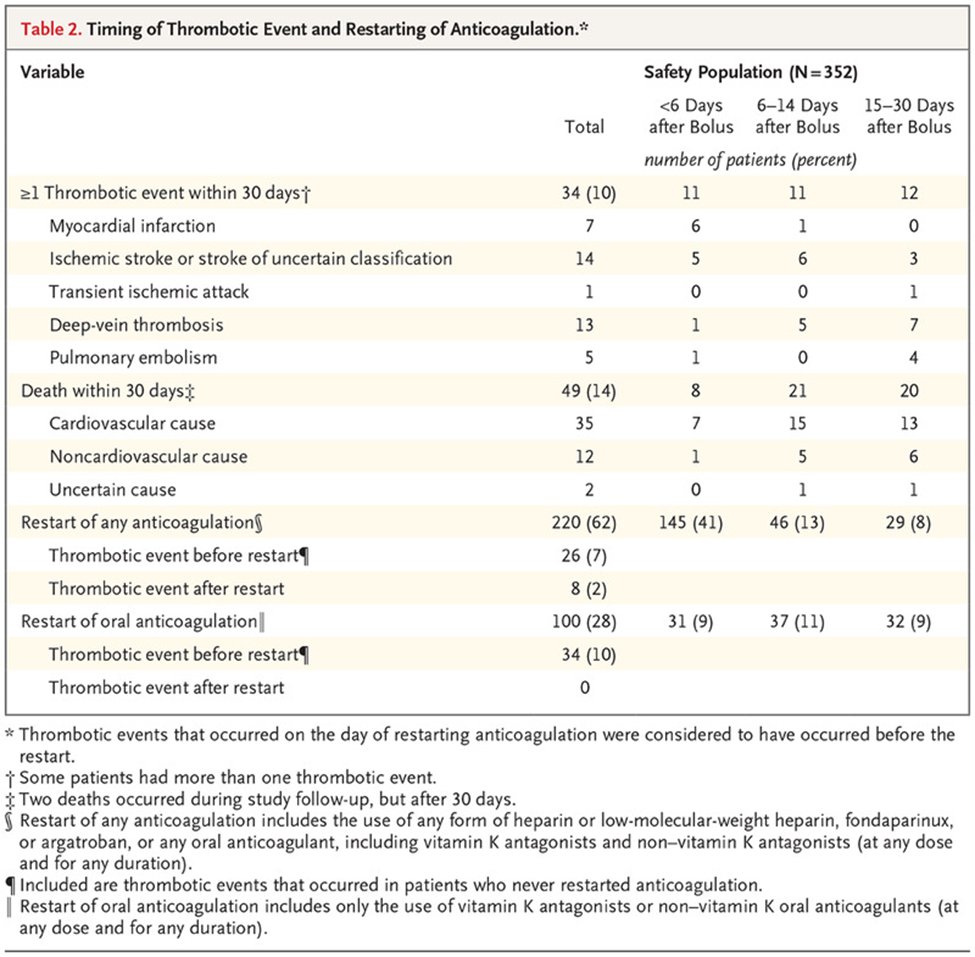
29) Multi-center, observational cohort studies have demonstrated high rates of #hemostasis and low risk of #thrombotic events
👉(5.5% w/ aPCC, 3.3% with 4-F PCC)
pubmed.ncbi.nlm.nih.gov/32264698/
👉(5.5% w/ aPCC, 3.3% with 4-F PCC)
pubmed.ncbi.nlm.nih.gov/32264698/
30) Andexanet is a FXa imitator molecule with ⬆️ affinity for FXa🛑, thus displacing the FXa🛑. This means that FXa interacts with #thrombin again!
Dosage (low= 880mg, high = 1760mg) depends on FxA 🛑 dosage and timing of last dose: (andexxa.com/dosing-adminis…)
Dosage (low= 880mg, high = 1760mg) depends on FxA 🛑 dosage and timing of last dose: (andexxa.com/dosing-adminis…)

31) Sometimes, patients may be unable to tell us when they last took FXa🛑. PT is most typically abnormal in someone taking FXa🛑, anti-FXa levels can also be calibrated by the lab to estimate the drug level, but this is not always available.
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…

32) #Andexanet was granted temporary @US_FDA approval for reversal of FXa🛑 after ANNEXA-4 was released: 🔓nejm.org/doi/full/10.10…. The reason for temporary approval? Patients were excluded if: GCS<7, ICH vol >60cc, or patient needed surgery (EVD or evacuation).
34) Whether #andexanet_alfa receives final FDA approval for reversal will depend on the results of the extension study (see: clinicaltrials.gov/ct2/show/NCT02…), which will include a surgical arm. Ideally, there will also be a RCT to directly determine which reversal strategy is best.
35) So how do you decide which agent to give when none have great data to support their use (2a vs. 2b #LOE)? It really comes down to availability and institutional policy. The @American_Heart guidelines recommend the following: 





36) Practically speaking, time to reversal is critically important #timeisbrain (🧠 = ⏰)!
Whichever approved agent is most rapidly available should be administered.
Whichever approved agent is most rapidly available should be administered.
37a) Because the patient could confirm that he had taken his #apixaban within the last 12 hours, and because #andexanet_alfa was available, this patient received andexanet and was then admitted to the Neuro ICU.
37b) Family reported a 5mg BID dose which he had last taken 10 hours prior. This is low dose reversal.
👉5 vials reconstituted and given as bolus + infusion
👉Bolus: 400mg IV administered at 30mg/min (~14 mins)
👉Infusion: 480mg IV given @ 4mg/min x 120 mins
👉5 vials reconstituted and given as bolus + infusion
👉Bolus: 400mg IV administered at 30mg/min (~14 mins)
👉Infusion: 480mg IV given @ 4mg/min x 120 mins

37c) Regardless of #reversal strategy, patients should be closely monitored with freq neuro exams & continuous BP monitoring or at least q15 min vital signs. ⚠️Note that current, commercially available anti-Xa levels do not accurately reflect the degree of FXa reversal after tx.
38) Pt underwent repeat CT head at 6h to assess for hematoma expansion & the hemorrhage appeared unchanged (phew!😥).
An interval study btwn 6 and/or at 24 hours is recommended in guidelines to assess for the possibility of 🩸 expansion & to determine the final hematoma volume.
An interval study btwn 6 and/or at 24 hours is recommended in guidelines to assess for the possibility of 🩸 expansion & to determine the final hematoma volume.

39) A quick way of assessing hematoma volume involves using the formula ABC/2, where A is biggest 🩸 diameter, B is diameter 90O to A and C is the approx # of CT slices with 🩸 X the slice thickness (🔓pubmed.ncbi.nlm.nih.gov/8711791/ ); image from jscimedcentral.com/NeurologicalDi… 

40) #ICH care in the ICU should then focus on
🤔Diagnostic workup, often with MRI to look for evidence of microbleeds in the deep territory (chronic hypertension) or cortex (associated with CAA).
💥Management of elevated #ICP as needed
🚶Early rehabilitation
🤔Diagnostic workup, often with MRI to look for evidence of microbleeds in the deep territory (chronic hypertension) or cortex (associated with CAA).
💥Management of elevated #ICP as needed
🚶Early rehabilitation
41) Quick Reminder 1:
👉ICH is an emergency, especially if pt is anticoagulated.
👉Addressing the #anticoagulation with #reversal (#andexanet) or repletion (#PCC) is a🔑component of care
👉@American_Heart gives preference to #andexanet if available, but 🗣️2🗣️studies are underway
👉ICH is an emergency, especially if pt is anticoagulated.
👉Addressing the #anticoagulation with #reversal (#andexanet) or repletion (#PCC) is a🔑component of care
👉@American_Heart gives preference to #andexanet if available, but 🗣️2🗣️studies are underway

42) Quick #ICH Reminder 2:
👉Currently, Seizure PPX is 🛑
👉cEEG can be used to detect sz in pts with unexplained AMS
👉PEACH demonstrated ⬇ in EEG sz with levetiracetam; this small trial was terminated early, underpowered, & no clinical sz were detected.
👉Further study needed!
👉Currently, Seizure PPX is 🛑
👉cEEG can be used to detect sz in pts with unexplained AMS
👉PEACH demonstrated ⬇ in EEG sz with levetiracetam; this small trial was terminated early, underpowered, & no clinical sz were detected.
👉Further study needed!

43) Quick #ICH Reminder 3:
👉Chemical DVT #prophylaxis should be started on these patients once the hemorrhage has stabilized. Pneumoboots are not enough!
👉Chemical DVT #prophylaxis should be started on these patients once the hemorrhage has stabilized. Pneumoboots are not enough!

44) Closing points:
🧠 #ICH can be life-threatening and devastating and rapid action is required
🧠 🔎 on airway management, #BP control, and anticoagulation reversal
👉 #Andexanet or #aPCC/4F#PCC are reasonable for DOAC reversal – but give tx fast!
🧠 #ICH can be life-threatening and devastating and rapid action is required
🧠 🔎 on airway management, #BP control, and anticoagulation reversal
👉 #Andexanet or #aPCC/4F#PCC are reasonable for DOAC reversal – but give tx fast!
45) More closing points:
🧠 Transfer these patients, if needed, to a hospital with a Neuro ICU
🧠 No seizure prophylaxis unless you suspect seizures
🧠 Start DVT prophylaxis once bleed stable (24-48 hours)
🧠 Transfer these patients, if needed, to a hospital with a Neuro ICU
🧠 No seizure prophylaxis unless you suspect seizures
🧠 Start DVT prophylaxis once bleed stable (24-48 hours)
46) @rkchoi & @caseyalbin & @academiccme thank you for joining & learning with us! Now go to cardiometabolic-ce.com/antithrombotic… and claim your 0.5h 🆓CE/#CME . . . and FOLLOW US for more education by #cardiometabolic experts!
• • •
Missing some Tweet in this thread? You can try to
force a refresh