1) Welcome to Part 1 of a new #accredited #tweetorial in our series of educational programs on #hypertrophic #cardiomyopathy #HCM. Previous programs, still available for 🆓CE/#CME, are at cardiometabolic-ce.com/category/hcm/.
Now you can earn another 1.5hr credit by following ALL of this 🧵!
Now you can earn another 1.5hr credit by following ALL of this 🧵!
2) Our expert author is Sergio Kaiser MD PhD FACC FESC 🇧🇷🇮🇱 @pabeda1, cardiologist 🫀, Professor 🎓 of #InternalMedicine, Rio de Janeiro State University. He brings the general cardiologist's perspective to our #HCM discussions. Read and learn!
#FOAMed #CardioTwitter
#FOAMed #CardioTwitter

3) This program is supported by an unrestricted educational grant from Bristol Myers Squibb. Statement of accreditation and faculty disclosures at cardiometabolic-ce.com/disclosures/. Credit for #physicians #nursepractitioners #physicianassociates #nurses #pharmacists from @academiccme.
4a) 1st description of #HCM in modern era was 1958. Dr Donald Teare named its obstructive phenotype “assimetrical septal hypertrophy”.
He discussed 8 young pts; 7 died suddenly. Autopsies showed #septal #hypertrophy, disarray of muscle fibers & clefts between muscle bundles

He discussed 8 young pts; 7 died suddenly. Autopsies showed #septal #hypertrophy, disarray of muscle fibers & clefts between muscle bundles


4b) We now know these to be hallmarks of the more severe forms of obstructive hypertrophic cardiomyopathy #oHCM.
See 🔓ncbi.nlm.nih.gov/pmc/articles/P….
See 🔓ncbi.nlm.nih.gov/pmc/articles/P….
5a) 1964: seminal paper from #EugeneBraunwald et al ➡️ 64 pts w/ "Idiopathic hypertrophic subaortic stenosis" #IHSS, showing the dynamic nature of subaortic obstruction.
Same article documented their initial efforts to perform #septal #myectomy
Same article documented their initial efforts to perform #septal #myectomy

5b) Their #myectomy ➡️significant symptomatic relief for some patients but by modern standards, the surgical fatality rate was prohibitively high.
See 🔓pubmed.ncbi.nlm.nih.gov/14227306/.
See 🔓pubmed.ncbi.nlm.nih.gov/14227306/.
6a) Called #HCM since 1979, then considered a rare inherited 🫀disease w/ almost no tx options & often ☠️⚰️.
Now recognized as a much more common & treatable dz, often compatible with longevity and distributed worldwide.
Now recognized as a much more common & treatable dz, often compatible with longevity and distributed worldwide.
6b) It affects about one in every 200 or 500 people, although a much smaller proportion ever gets to be clinically diagnosed.
See 🔓pubmed.ncbi.nlm.nih.gov/35086660/
See 🔓pubmed.ncbi.nlm.nih.gov/35086660/

7a) Presently, numerous tx options are available ➡️significant ⤵️in #HCM #morbidity & #mortality. However, as many pts may remain asx for a long time--even a lifetime--a high level of clinical suspicion is required.
7b) Only with accurate dx can appropriate risk strat & ensuing family screening be max'd. #HCM clinical presentation has many nuances & it is paramount to distinguish it from #phenocopies e.g. #Noonan syndrome #Fabry dz #TTR cardiac #amyloidosis & other presentations...
7c) ..assoc'd w/ 🫀 hypertrophy eg arterial #hypertension & characteristic physiologic #hypertrophy of #athlete’s 🫀. Each of these pathologies carries specific tx recs: another imp't reason to pursue correct dx.
See @cardiomet author @IacopoOlivotto et al pubmed.ncbi.nlm.nih.gov/36582184/
See @cardiomet author @IacopoOlivotto et al pubmed.ncbi.nlm.nih.gov/36582184/
8) Before discussing clinical features, dx, & tx, let’s go back to basics: How does 🫀 muscle contract? Let's look specifically at excitation-contraction coupling and how left ventricular #contractile proteins interact in order to generate pumping of 🩸throughout the body.
9) 🫀 muscle work is energy-consuming & is regulated by an active mechanism of Ca ion handling in & out of contractile proteins of the #sarcomere (basic contractile unit of the cadiomyocyte) to cyclically generate force & relaxation. This req's adenosine triphosphate #ATP.
10a) Among ~ 20 #sarcomere proteins, the essentials are the thin filament #actin & the thick filament #myosin. The sarcomere itself consists of roughly 20 proteins. The plasma membrane #sarcolemma bounds each myocyte & invaginates to form a complex tubular network (T tubules)...
10b) ... from where #actionpotential-triggered Ca currents are transmitted to the #sarcoplasmic reticulum & amplified along the myofibrils.
Thin actin filaments are anchored at the Z line & form transient sliding interactions w/ thick myosin filaments.
Thin actin filaments are anchored at the Z line & form transient sliding interactions w/ thick myosin filaments.

10c) Actin filaments slide past myosin filaments, so during contraction Z lines & actin filaments converge toward the center of the #sarcomere (M line) and move away from it during relaxation.
Let's look at a microscopic image of the #sarcomere in polarized light:
Let's look at a microscopic image of the #sarcomere in polarized light:
10d)
👉M Line (center)
👉I Band contains only #actin filaments
👉H zone contains only myosin filaments & is where sliding actin filaments from both sides approach each other
👉A band contains the mass of myosin filaments
👉M Line (center)
👉I Band contains only #actin filaments
👉H zone contains only myosin filaments & is where sliding actin filaments from both sides approach each other
👉A band contains the mass of myosin filaments

10e) #Titin, the largest #protein found in the human body, connects the Z lines & contributes both to the elastic properties of the #sarcomere during relaxation, & to force generation during contraction, when it reexpands like a compressed spring.
From physio-pedia.com/File:Sarcomere…
From physio-pedia.com/File:Sarcomere…
11a) #Actin filaments are intertwined w/ helical protein #tropomyosin ➡️ major role in coordinating the sliding process. Actin cross-bridging sites to myosin are “hidden” by tropomyosin & can only be exposed when a “gate keeper” – the troponin complex - is activated by Ca ions.
11b) #Myosin heads are projections from the core protein composed of heavy & light chains. The heavy chain has a major domain that interacts with actin and has also a pocket for #ATP binding. Myosin is actually an #ATPase & acts like a propeller.
11c) Energy liberated from ATP hydrolysis ➡️ flexing of the myosin head & the strong binding (power stroke) to the nearest actin site. The power stroke is reversed once the resulting molecule of ADP is released and a new ATP binds to the myosin head pocket, ➡️ relaxation. 



12a) Now that we have reviewed some basic features of cardiac muscle contraction, we can discuss more deeply the subject of this #tweetorial. And we begin by asking: What is hypertrophic cardiomyopathy #HCM? Let's make sure you are ready.
12b) What molecule provides fuel to accomplish myocardial contraction?
12c) Mark your best response & tune in here TOMORROW for the next installment of this #tweetorial. You are earning 🆓CE/#CME!
👏 @FudimMarat @BiykemB @AndreasGevaert @SubodhVermaMD @ArgaizR @jpcostabel @NMerke @lynchsantiago @lilianigromaia @alexariasmx20 @luisbeckdasilva
👏 @FudimMarat @BiykemB @AndreasGevaert @SubodhVermaMD @ArgaizR @jpcostabel @NMerke @lynchsantiago @lilianigromaia @alexariasmx20 @luisbeckdasilva
13) Welcome back! We are talking all about #HCM from the general #cardiologyperspective with expert author @pabeda1 🇧🇷🇮🇱 and you are earning LOTS of 🆓CE/#CME by following this 🧵
#CardioTwitter #MedTwitter #MedEd @MedTweetorials @PreMedTweets @4hcm
#CardioTwitter #MedTwitter #MedEd @MedTweetorials @PreMedTweets @4hcm
14) Yesterday's quiz? The correct answer is B: #ATP, which regulates calcium ion handling in & out of contractile proteins of the #sarcomere to cyclically generate force & relaxation. 

15a) So, as promised, let's move on to #HCM. What is hypertrophic cardiomyopathy? It is a primary disorder of the #myocardium, mainly characterized by unexplained #LV hypertrophy when no pressure or volume overload or no infiltrative or storage disorders can be deemed causative.
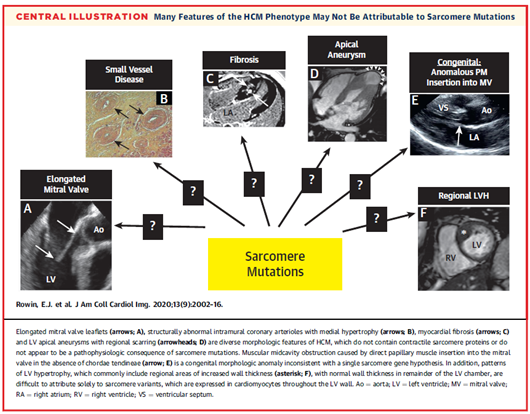
15b) Other features contribute to the phenotypic expression of #HCM
🫀 myocardial fiber disarray
🫀 fibrosis
🫀 apical aneurysm
🫀 microvascular ischemia
🫀 (often) obstruction to LV outflow due to massively hypertrophied LV septum or anterior systolic motion of an elongated MV
🫀 myocardial fiber disarray
🫀 fibrosis
🫀 apical aneurysm
🫀 microvascular ischemia
🫀 (often) obstruction to LV outflow due to massively hypertrophied LV septum or anterior systolic motion of an elongated MV
15c) Bonus pic: Anterior systolic motion of the mitral valve seen by M-mode echocardiography, leading to left ventricular outflow obstruction. Note the hypertrophied interventricular septum. 

16) For a long time #HCM has been seen as #sarcomeric disease caused by an autosomal dominant #mutation of the #myosin filament ➡️hypercontractile state. Below see at least 11 mutations associated with the development of HCM, from pubmed.ncbi.nlm.nih.gov/22874472/: 

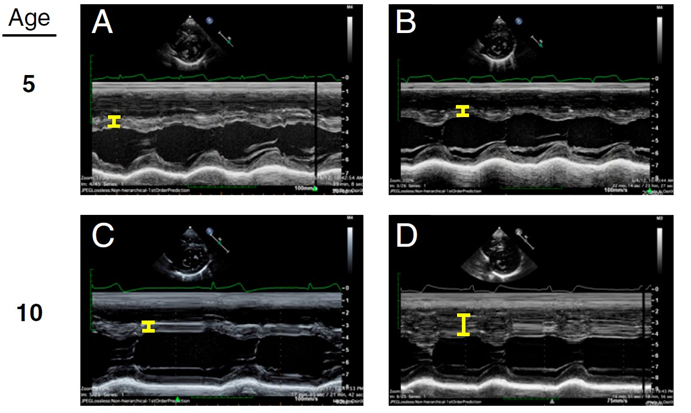
17a) Alas, the clinical presentation of #HCM does not fit into a simplified vision of a monogenic inheritable disease. There is a wide range of phenotypic expressions w/o detectable mutations & also incomplete penetrance of a pathogenic mutation within the same family cluster. 


17b) For example: identical twins with a positive genetic diagnosis of #HCM underwent #echocardiography at the age of 5 years. Septal thickness was normal in both, but five years later, one--& only one--of them developed septal hypertrophy.
See 🔓pubmed.ncbi.nlm.nih.gov/33658374/
See 🔓pubmed.ncbi.nlm.nih.gov/33658374/
17c) Another: Variable phenotypic expression in the offspring of a ♂️w/ #HCM + for #MYBPC3 mutation. 3 of 4 siblings are also carriers. ♂️ B develops massive septal hypertrophy, ♀️ C shows limited hypertrophy, & ♀️ D has normal LV.
🔓 pubmed.ncbi.nlm.nih.gov/31864978/
🔓 pubmed.ncbi.nlm.nih.gov/31864978/

18a) So #HCM must be dx'd on clinical grounds & imaging, not by genetic tests. Imaging:
👉#echocardiography #CMR or #CT showing max end-diastolic thickness of #LV > 15mm in adults in the absence of an identifiable cause.
👉13-14mm ➡️suspicion for HCM if + FamHx or + genetic tests
👉#echocardiography #CMR or #CT showing max end-diastolic thickness of #LV > 15mm in adults in the absence of an identifiable cause.
👉13-14mm ➡️suspicion for HCM if + FamHx or + genetic tests
18b) In children, the clinical expression of #HCM is much less frequent. Dx requires #LV wall thickness more than two standard deviations greater than the predicted mean (z-score 2, where a z-score is defined as the number of standard deviations from the population mean).
18c) So imaging confirms clinical suspicion. Genetics helpful, but instead of thinking of #HCM purely as a mutation, the interplay among biological, environmental, & social influences will ultimately determine the phenotypic expression of this disease.
🔓 ncbi.nlm.nih.gov/pmc/articles/P…
🔓 ncbi.nlm.nih.gov/pmc/articles/P…

19) As a general cardiologist, I see #HCM in 3⃣ hemodynamic categories: non-obstructive, obstructive, and latent-obstructive. In latent-obstructive, #LV outflow gradient <30 mmHg at rest but exceeds this threshold on exertion.
🔓 ncbi.nlm.nih.gov/pmc/articles/P…
🔓 ncbi.nlm.nih.gov/pmc/articles/P…

20a) Clinical evaluation for #HCM may be triggered by ID of + FamHx, symptoms like fatigue, dyspnea on exertion, syncope or pre-syncope, by detecting a murmur, by abnormal #ECG, or w/ #echocardiogram performed for other indications.
20b) Not infrequently, a diagnostic suspicion is raised by the finding, in an otherwise normal person, of deep, inverted symmetrical T waves on the electrocardiogram, mistakenly interpreted as myocardial ischemia
(Figure from ecg-interpretation.blogspot.com/2013/01/ecg-in…)
(Figure from ecg-interpretation.blogspot.com/2013/01/ecg-in…)

21a) Once suspicion for #HCM is raised, 2020 @ACCinTouch/ @American_Heart #guidelinesrecommend a comprehensive H&P & complete 3⃣-generation #FamHx. Some clinical features can distinguish #phenocopies from true HCM:
🔓 pubmed.ncbi.nlm.nih.gov/33215931/

🔓 pubmed.ncbi.nlm.nih.gov/33215931/


21b) Per guidelines, echo at rest & w/ valsalva are usu first imaging. Then Class I recommendation for #CMR if echo is inconclusive, if there is suspicion of alternative dx, or when a decision to proceed to #ICD for sudden death prevention is still uncertain.
21c) A very practical algorithm for assessment & follow-up of patients with suspected #HCM has recently been proposed by Maron et al (🔓 pubmed.ncbi.nlm.nih.gov/35086660/): 

22a) It's essential to reassure patients & families that #HCM is treatable & is compatible w/ longevity, but periodic reassessment is req'd ad infinitum. Its evolution is not uniform & there are different pathways it can follow, from no progression at all to significant dis.
22b) Below see guidance for periodic clinical and non-invasive testing in HCM.
Next to that see possible #HCM pathways a pt may follow. Only 10% progress along >1 pathway (🔓 pubmed.ncbi.nlm.nih.gov/25446045/).

Next to that see possible #HCM pathways a pt may follow. Only 10% progress along >1 pathway (🔓 pubmed.ncbi.nlm.nih.gov/25446045/).

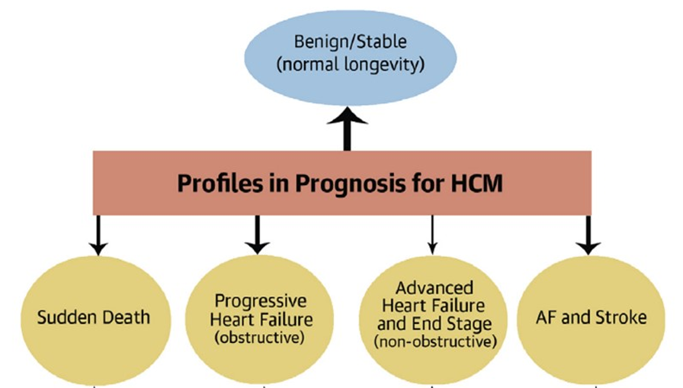
22c) #HCM exerts its most significant clinical effect in midlife:
🫀 avg age 1st #ICD to prevent #SCD = 45
🫀 first #mymectomy for #HF = 52
🫀 onset of #AFib = 54,
per 🔓
pubmed.ncbi.nlm.nih.gov/35084989/
🫀 avg age 1st #ICD to prevent #SCD = 45
🫀 first #mymectomy for #HF = 52
🫀 onset of #AFib = 54,
per 🔓
pubmed.ncbi.nlm.nih.gov/35084989/
22d) Among 1000 consecutive adult pts, mean age 52±17 at dx, followed 9.3±8 y, 4 distinct pathways:
1⃣ ~50% no progression
2⃣ 43% developed #HF from #LVOTO
3⃣ 17% developed atrial fibrillation
4⃣6% experienced sudden death
🔓 pubmed.ncbi.nlm.nih.gov/35084989/
1⃣ ~50% no progression
2⃣ 43% developed #HF from #LVOTO
3⃣ 17% developed atrial fibrillation
4⃣6% experienced sudden death
🔓 pubmed.ncbi.nlm.nih.gov/35084989/

23) Thanks to advances in risk stratification, medical and interventional therapy for #HCM, mortality has sharply ⬇️from 3 – 6% per year in early referral cohorts ➡️ only 0.5% per year in contemporary referral cohorts
🔓pubmed.ncbi.nlm.nih.gov/35084989/
🔓pubmed.ncbi.nlm.nih.gov/35084989/

24a) One can never overlook though the possibility of (and pt concern over) sudden cardiac death #SCD with #HCM. We have multiple tools: for example, #CMR w/ late #gadolinium enhancement (#LGE) can predict risk of sudden death (and thus referral to #ICD implant).
24b) When LGE occupies >15% of the LV wall, adverse remodeling ensues and the risk of sudden death increases two-fold. See 🔓pubmed.ncbi.nlm.nih.gov/25092278/ 



24c) Even w/o #CMR, pts at risk of #SCD can be ID'd w/ clinical & echocardiographic variables. See validated ACC/AHA algorithm at professional.heart.org/en/guidelines-…, with C-statistic 0.81 (95% CI, 0.77-0.85) for discrimination between patients who did or did not experience #SCD.
24d) Here are potential risk factors for sudden death according to ACC/AHA guidelines (🔓 pubmed.ncbi.nlm.nih.gov/33215931/): 

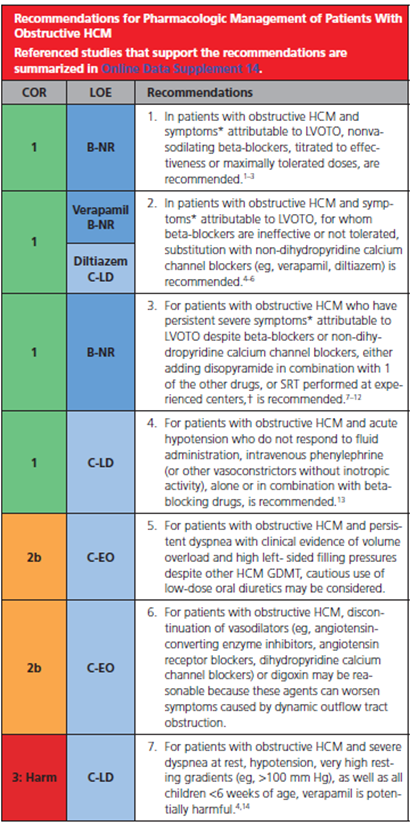
25a) So what about tx of #HCM? For many yrs we were limited to very few pharm options for sx control & scant resources to predict/prevent #SCD.
💊Beta-blockers, non-dihydropyridine #CCBs, disopyramide & cautious diuretic use may help sx, but do not modify disease course.
💊Beta-blockers, non-dihydropyridine #CCBs, disopyramide & cautious diuretic use may help sx, but do not modify disease course.
25b) New approaches to tx #LVOTO--surgical #myectomy & alcohol septal #ablation were introduced and addressed many sx, while #SCD episodes were largely ⬇️ after introduction of #ICD’s.
25c) More recently, intro of #myosin inhibitors allows for 1st time a pharmacological approach with disease-modifying potential, though its long term resilience remains to be proven. We will address the data on this in Part 2.
25d) Meanwhile, 2020 ACC/AHA #guidelines for classical pharmacological therapy of patients with #oHCM are summarized here:
🔓 pubmed.ncbi.nlm.nih.gov/33215931/
🔓 pubmed.ncbi.nlm.nih.gov/33215931/
25e) Regarding those with non-obstructive forms of HCM and preserved ejection fraction, a summary of recommendations for pharmacological therapy is depicted here:
🔓 pubmed.ncbi.nlm.nih.gov/33215931/
🔓 pubmed.ncbi.nlm.nih.gov/33215931/

25f) Notably, there are no recommendations for pharmacological treatment in asymptomatic patients with proven non-obstructive #HCM.
26a) Re #HeartFailure in #HCM: Data from a large registry of pts #SHARE enrolled 1960-2019 ➡️over 15y, new #LV systolic dysfunction #LVSSD developed 7.5%/y (🔓pubmed.ncbi.nlm.nih.gov/32228044/).
26b) Among those w/ #LVSD, sig predictors of composite all-cause death, cardiac transplantation & #LVAD implantation were
🫀multiple pathogenic/likely pathogenic sarcomeric variants: HR 5.6 [95% CI, 2.3–13.5]
🫀 #Afib: HR 2.6 [1.7–3.5]
🫀 #LVEF < 35% HR 2.0 [1.3–2.8]
🫀multiple pathogenic/likely pathogenic sarcomeric variants: HR 5.6 [95% CI, 2.3–13.5]
🫀 #Afib: HR 2.6 [1.7–3.5]
🫀 #LVEF < 35% HR 2.0 [1.3–2.8]
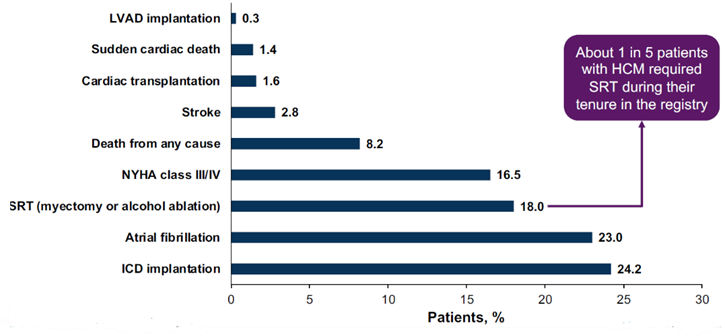
26c) Pts w/ pathogenic sarcomeric variants, ⬆️#LV wall thickness, #LV dilation, & borderline low #LVEF (50%–59%) were at higher risk for developing #HCM with #LVSD. Here is the overall incidence of several events reported in the registry: 
26d) 1/4 pts dev'd #AFib. Recently, ablation techniques & septal myectomy+/- #Cox_Maze surgery ➡️ 50% ⬇️in recurrent episodes over the short term (pubmed.ncbi.nlm.nih.gov/31727261/).
🫀 BTW, mortality attrib'd to #AF in contemp cohorts of #HCM pts is <1%/y (🔓pubmed.ncbi.nlm.nih.gov/28916640/).
🫀 BTW, mortality attrib'd to #AF in contemp cohorts of #HCM pts is <1%/y (🔓pubmed.ncbi.nlm.nih.gov/28916640/).
27a) Surgical #myectomy (or alcohol septal ablation in pts at high surg risk) is now assoc'd with high success rates & only 0.5% 30d operative mortality when performed at a center of excellence.
See 🔓pubmed.ncbi.nlm.nih.gov/26361164/.
See 🔓pubmed.ncbi.nlm.nih.gov/26361164/.
27b) In such centers, myectomy ➡️survival benefit w/ 99%, 98%, & 95% free from HCM-related mortality at 1, 5, & 10 yrs, respectively. See 🔓pubmed.ncbi.nlm.nih.gov/16053960/. Lower-volume centers don't perform as well: 🔓pubmed.ncbi.nlm.nih.gov/36631204/ 

28) So what if we could improve #HCM outcomes and treat underlying pathology WITHOUT a need for surgery? That's where the new #myosin inhibitors come in, and that will be the subject of Part 2 of this tweetorial, to follow next week. Meanwhile . . .
29) Which of the following is NOT a #riskfactor for #SCD in a patient with #HCM?
a. unexplained recent syncope
b. recent acute coronary syndrome
c. diffuse and extensive late gadolinium enhancement
d. LV apical aneurysm
Mark your answer!
a. unexplained recent syncope
b. recent acute coronary syndrome
c. diffuse and extensive late gadolinium enhancement
d. LV apical aneurysm
Mark your answer!
30) So you don't wish an #ACS on anyone, but in the setting of #HCM, ACS has not been found to ⬆️risk of #SCD. Need a refresher on that? See the table in tweet 24d ⤴️
31) For now, you have earned 0.75h 🆓CE/#CME and you can claim it with a few clicks of the 🖱️at cardiometabolic-ce.com/hcm5a/. I am @pabeda1 and I hope you'll join me next week for Part 2 of this tweetorial!
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter













