1) Welcome to a 🆕accredited tweetorial from @cardiomet_CE! We welcome back expert faculty @ChristosArgyrop to discuss screening for #CKD in pts w/ #T2D & the role of routine assessment for #microalbuminuria as an effective diagnostic, risk stratification, & patient ed tool.
2) Christos Argyropoulos MD, PhD @ChristosArgyrop is Division Chief, Nephrology @UNMHSC. #CKD is chronic #kidneydisease, #ESKD is end-stage kidney disease.
#FOAMed #nephtwitter #cardiotwitter @MedTweetorials @NephUCommunity @ISNkidneycare @KidneyDiseaseFm
#FOAMed #nephtwitter #cardiotwitter @MedTweetorials @NephUCommunity @ISNkidneycare @KidneyDiseaseFm

3) This program is intended for #HCPs and is supported by an unrestricted educational grant from Bayer. Statement of accreditation & faculty disclosures at cardiometabolic-ce.com/disclosures/.
FOLLOW US for more expert-authored #tweetorials and earn #MedEd
FOLLOW US for more expert-authored #tweetorials and earn #MedEd
4) Let’s kick off this program with a case to orient us to the clinical problems. Your next pt in clinic is 60 ♀️ with 10y history of #T2D. She had had “pre-diabetes” for another 10 years prior to that, & her #A1c for the last year had been <7.0%.
5) At this point you should do which of the following:
6) Before exploring the answer, let’s consider the problem(s) we are trying to solve in patients with #T2D. These problems burden individuals, public health and the financial health of healthcare systems & are shown in the infographic ⤵️
cjasn.asnjournals.org/content/clinja…
cjasn.asnjournals.org/content/clinja…

7) While #glycemic control continues to be important in the management of patients, patients in our era continue to suffer the adverse #cardiovascular & kidney effects of #T2D, with the former being quantitatively more prevalent & the latter straining public finances
8) Returning to the vignette, the patient has excellent glycemic control for the current guidelines (diabetesjournals.org/care/article/4…), so the focus should be on reducing the impact of #T2D on the #cardiovascular system and the kidney. 

9) The impact could be reduced by knowing the patient’s risk for cardiovascular and kidney complications, and this risk is VERY HIGH. In a study involving ~ 500k pts from the UK >70% of individuals with #T2D would go on to develop such complications
bmcmedicine.biomedcentral.com/articles/10.11…

bmcmedicine.biomedcentral.com/articles/10.11…


10) Returning to the vignette, pt would benefit from quantifying her #cardiovascular & #kidney disease risk by ✔️:
→cholesterol
→ kidney function (eGFR)
→ kidney damage (proteinuria) labs. The latter 2 are NOT part of the ACC/AHA risk calculator
tools.acc.org/ASCVD-Risk-Est…
→cholesterol
→ kidney function (eGFR)
→ kidney damage (proteinuria) labs. The latter 2 are NOT part of the ACC/AHA risk calculator
tools.acc.org/ASCVD-Risk-Est…
11) A classic study, now part of the data cited by the guidelines, has shown that abnormal #eGFR & proteinuria predict all risks associated with #CKD:
✔️All-cause Death
✔️Cardiovascular Death
✔️Progression of #CKD
✔️ #ESKD
✔️Acute Kidney Injury #AKI
🔓kidney-international.org/article/S0085-…
✔️All-cause Death
✔️Cardiovascular Death
✔️Progression of #CKD
✔️ #ESKD
✔️Acute Kidney Injury #AKI
🔓kidney-international.org/article/S0085-…

12) Current guidelines say that a measurement of both kidney function (#eGFR) and damage (#proteinuria) must be obtained in clinical practice. For the latter we prefer the measurement of #albuminuria (as the ratio of urinary albumin to creatinine ratio #UACR in a morning) sample.
13) These tests should be obtained at least annually in all patients with #diabetes, starting immediately upon diagnosis in patients with #T2D and within 5 years after the diagnosis of patients with Type 1 diabetes #T1D
diabetesjournals.org/care/article/4…
diabetesjournals.org/care/article/4…
14) Per the @AmDiabetesAssn standards of care the frequency of testing & clinical visits (see chart ↓) may be higher in patients with #T2D & #CKD, and the outcome of testing may be used to determine consultations and referrals within the healthcare system. 

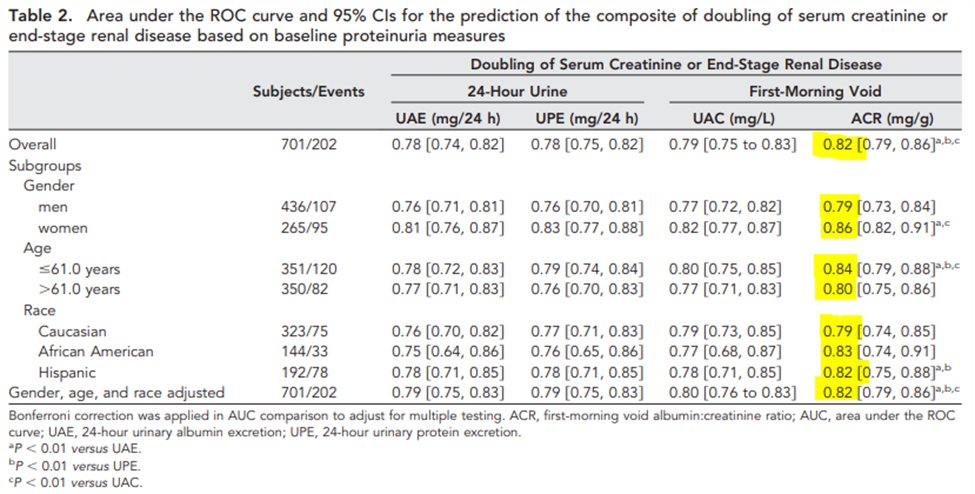
15) Important non-trivial trivia! Why do the guidelines highlight #UACR as the preferred method for kidney damage assessment? As it stands, there is strong evidence about this point that originated nearly 20 years ago from the seminal trials of Angiotensin Receptor Blockers #ARB
16) The #RENAAL study examined various ways to measure kidney damage through:
➡️ 24hr Protein (UPE)
➡️ 24hr Albumin (UAE)
➡️ First Morning Voided (FMV) Albumin/Creatinine
➡️ FMV Protein/Creatinine
jasn.asnjournals.org/content/21/8/1…
While they all predicted #ESKD, #UACR was the best!

➡️ 24hr Protein (UPE)
➡️ 24hr Albumin (UAE)
➡️ First Morning Voided (FMV) Albumin/Creatinine
➡️ FMV Protein/Creatinine
jasn.asnjournals.org/content/21/8/1…
While they all predicted #ESKD, #UACR was the best!

17) #UACR by itself is an established, yet under-appreciated, underutilized risk factor for #cardiovasculardisease in individuals w/out #diabetes (as shown in Framingham study : ahajournals.org/doi/10.1161/ci…, left panel) AND pts with #T2D:
ncbi.nlm.nih.gov/pmc/articles/P… (right panel)

ncbi.nlm.nih.gov/pmc/articles/P… (right panel)


18) Given such data one could use two metaphors inspired by cardiovascular medicine:
Kidney Function ↔️ eGFR ↔️ “Ejection Fraction” of the Kidney
Kidney Damage ↔️ UACR ↔️ Kidney’s “Cholesterol”
Both tests predict cardiovascular & kidney outcomes in #CKD & #T2D
Kidney Function ↔️ eGFR ↔️ “Ejection Fraction” of the Kidney
Kidney Damage ↔️ UACR ↔️ Kidney’s “Cholesterol”
Both tests predict cardiovascular & kidney outcomes in #CKD & #T2D
19) “Knowing the kidney numbers” is the only way for patients (and practitioners!) to know the status of the kidney health & future risk. This is the advice given by both the @CDCChronic & the @nkf
cdc.gov/kidneydisease/…
kidney.org/atoz/content/k…

cdc.gov/kidneydisease/…
kidney.org/atoz/content/k…

20) #UACR & #eGFR are also included in The Kidney Risk Failure Equation (#KRFE) first developed in in Canada by @NavTangri & subsequently validated in more than 700k patients from 30+ countries.
Available in smartphone apps (e.g. @QxMD) and the web kidneyfailurerisk.com
Available in smartphone apps (e.g. @QxMD) and the web kidneyfailurerisk.com
21) The #KRFE quantifies the risk for patients & in conjunction w/ guidelines allows us to navigate the next steps:
✔️referral to #Nephrology if the 5-year risk is > 3%
✔️team-based care (if the 2-year risk > 10%)
✔️preparation for renal replacement (if the 2-year risk > 20%)
✔️referral to #Nephrology if the 5-year risk is > 3%
✔️team-based care (if the 2-year risk > 10%)
✔️preparation for renal replacement (if the 2-year risk > 20%)
22) The patient in our vignette had both these tests performed. Her #eGFR was 45 ml/min/1.73m2 and her #UACR was 500mg/gm creatinine. How does knowing the numbers help manage her risk at this point? Let’s put her on the #KDIGO heat map & the #KRFE and help her & us find out! 

23) Knowing the numbers allows providers to
➡️#diagnose #CKD
➡️ #stage #CKD
➡️ gauge #risk for #heart and #kidneycomplications
➡️establish a monitoring/referral plan
Most importantly they help patients visualize the status of their kidneys & in doing so, empowers them.
➡️#diagnose #CKD
➡️ #stage #CKD
➡️ gauge #risk for #heart and #kidneycomplications
➡️establish a monitoring/referral plan
Most importantly they help patients visualize the status of their kidneys & in doing so, empowers them.
24) In having conversations about the next steps, one can use the #KFREcalculators.
➡️4 Variable: Age, Sex, eGFR, UACR
➡️8 Variable includes the 4 Variable + Calcium, Phosphorus, Bicarbonate, & *Serum* Albumin. This version may discriminate better.
🔓jamanetwork.com/journals/jama/…
➡️4 Variable: Age, Sex, eGFR, UACR
➡️8 Variable includes the 4 Variable + Calcium, Phosphorus, Bicarbonate, & *Serum* Albumin. This version may discriminate better.
🔓jamanetwork.com/journals/jama/…
25) The #KFRE output for outpatient & the next steps is concordant with the #CKD heatmap, but provides further detail about her risk for progression of #KidneyDisease. It is also a great tool for patients to use when discussing their own kidney health with their providers! 







26) According to the heatmap and #KFRE the patient has moderate #CKD but she is at high risk for #cardiovascular and #kidneycomplications. How does one reduce the risk of these complications from #T2D & #CKD ? Enter @AmDiabetesAssn's 4⃣-pillar model:
diabetesjournals.org/care/article/4…
diabetesjournals.org/care/article/4…
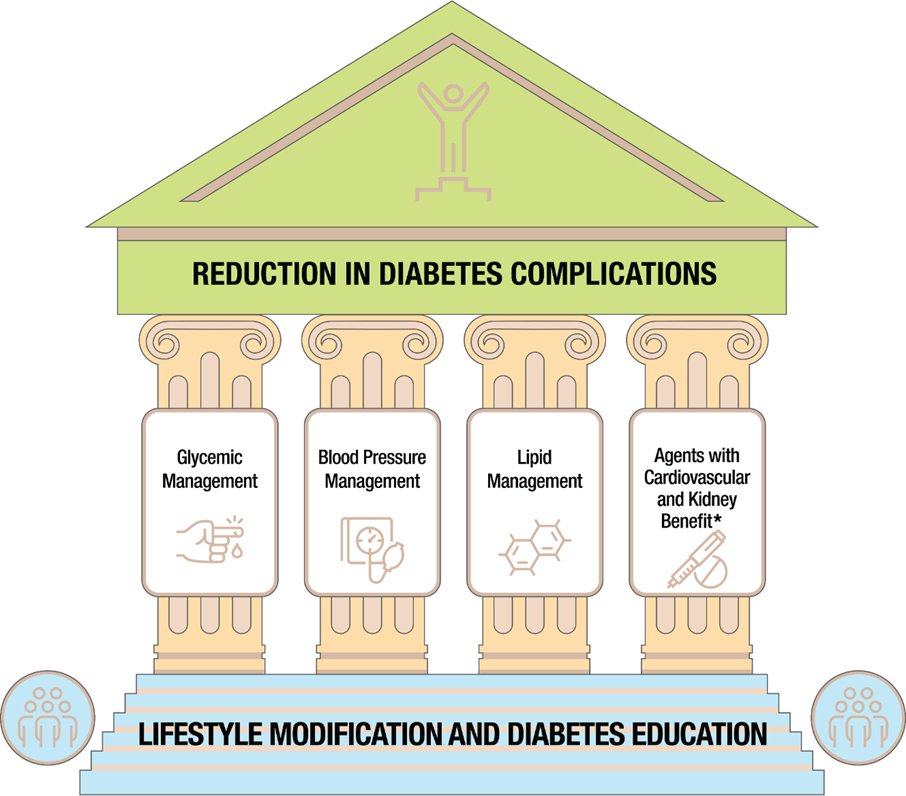
27) Do we have all the data we need to apply this pillar model to our pt? Have we empowered her to assume control of her own kidney health by knowing ALL the numbers?
➡️ #A1c
➡️ #UACR/#eGFR
➡️Lipid panel
➡️Blood pressure
➡️Lifestyle factors
➡️Appropriate medications
➡️ #A1c
➡️ #UACR/#eGFR
➡️Lipid panel
➡️Blood pressure
➡️Lifestyle factors
➡️Appropriate medications
28) We need to do more to help our pts know their numbers.
➡️In many areas in the 🇺🇸, measurement of #UACR lags behind measurement of the #eGFR pubmed.ncbi.nlm.nih.gov/35997775/
➡️There is large variation in obtaining #UACR even inside the same health care system!
ncbi.nlm.nih.gov/pmc/articles/P…


➡️In many areas in the 🇺🇸, measurement of #UACR lags behind measurement of the #eGFR pubmed.ncbi.nlm.nih.gov/35997775/
➡️There is large variation in obtaining #UACR even inside the same health care system!
ncbi.nlm.nih.gov/pmc/articles/P…



29) It is easy to dismiss these findings of large gaps in #UACR testing as metrics without substance. However, #UACR testing matters, & it does quite a bit when caring for patients. How does knowing the #UACR help us manage individuals, & why does it matter ?
30) The evidence- & guideline-based answer to the previous poll is an unequivocal “All of the above”.
➡️#UACR is an important diagnostic criterion for the presence of #CKD & the latter weighs heavily in selecting hypoglycemic agents for pts w/#T2D
diabetesjournals.org/care/article/4…
➡️#UACR is an important diagnostic criterion for the presence of #CKD & the latter weighs heavily in selecting hypoglycemic agents for pts w/#T2D
diabetesjournals.org/care/article/4…

31)⬆️#UACR indicates the presence of #CKD & the latter guides the choice of antihypertensive agents to include inhibitors of the #RAS (#ACEi & #ARBs) according to both the #ADA & the @goKDIGO guidelines
🔓 diabetesjournals.org/care/article/4…
🔓 kdigo.org/wp-content/upl…

🔓 diabetesjournals.org/care/article/4…
🔓 kdigo.org/wp-content/upl…


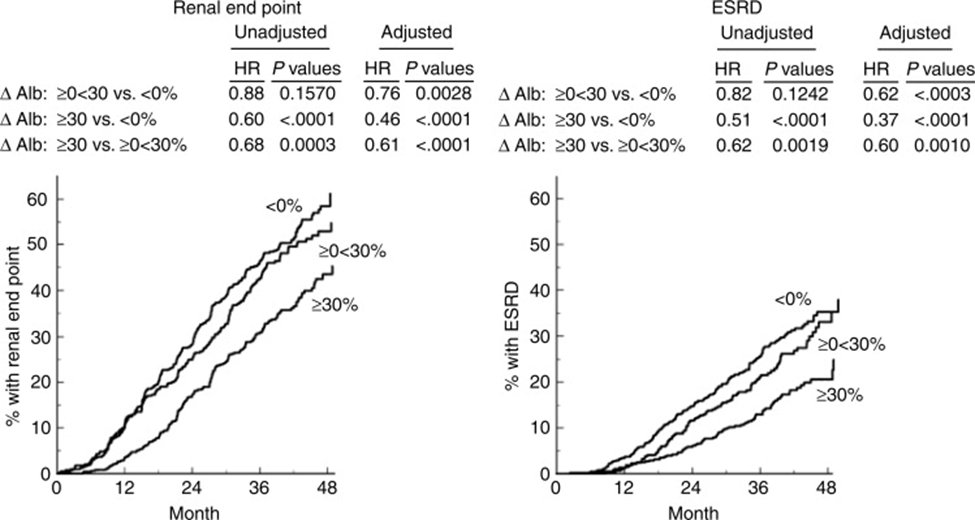
32) The use of #UACR to guide selection of further therapies in patients with #T2D & #CKD is firmly rooted in the concept of “residual risk”, i.e. the risk for the development of worsening kidney function and #cardiovascular risk among patients treated with #ACEi or #ARB.
33) Residual Risk for progression of #CKD was analyzed in the #ARB trials. Relevant papers:
🔓pubmed.ncbi.nlm.nih.gov/23506627/
🔓pubmed.ncbi.nlm.nih.gov/15149345/
👉risk⬇️ was continuously related to albuminuria ⬇️ (the more the better!)
✔️risk highest in those with highest UACR
🔓pubmed.ncbi.nlm.nih.gov/23506627/
🔓pubmed.ncbi.nlm.nih.gov/15149345/
👉risk⬇️ was continuously related to albuminuria ⬇️ (the more the better!)
✔️risk highest in those with highest UACR
34) Residual #UACR has been a major criterion for inclusion in both the #SGLT2i
🔓 ncbi.nlm.nih.gov/pmc/articles/P…
🔓 nephjc.com/news/dapa-ckd (@priti899) &
and the non-steroidal #MRA #finerenone randomized controlled clinical trials #RCTs.
🔓 doi.org/10.1093/eurhea…

🔓 ncbi.nlm.nih.gov/pmc/articles/P…
🔓 nephjc.com/news/dapa-ckd (@priti899) &
and the non-steroidal #MRA #finerenone randomized controlled clinical trials #RCTs.
🔓 doi.org/10.1093/eurhea…


35) In the #SGLT2i and #MRAtrials, pts w/ #T2D who received active treatment had ⬇️ in #UACR:
👉 31% in CREDENCE (#canagliflozin)
🔓nejm.org/doi/10.1056/NE…
👉 35% in DAPA-CKD (#dapagliflozin)
🔓pubmed.ncbi.nlm.nih.gov/34619106/
👉 32% in FIGARO-CKD (#finerenone)
🔓nejm.org/doi/full/10.10…
👉 31% in CREDENCE (#canagliflozin)
🔓nejm.org/doi/10.1056/NE…
👉 35% in DAPA-CKD (#dapagliflozin)
🔓pubmed.ncbi.nlm.nih.gov/34619106/
👉 32% in FIGARO-CKD (#finerenone)
🔓nejm.org/doi/full/10.10…
36) #UACR will continue to play a role for the development of future novel therapies in #CKD and #T2D as it fulfills the criteria for surrogate end point in clinical trials in early kidney disease.
pubmed.ncbi.nlm.nih.gov/31473020/
pubmed.ncbi.nlm.nih.gov/31473020/
37) The biological plausibility for #UACR as a surrogate is high:
👉 ⬆️#UACR in UACR precede ⬇️ in #eGFR
👉 ⬆️#UACRreflect increase glomerular permeability (and thus kidney damage)
👉 ⬆️ albumin may exert direct toxic effects
👉 ⬆️#UACR in UACR precede ⬇️ in #eGFR
👉 ⬆️#UACRreflect increase glomerular permeability (and thus kidney damage)
👉 ⬆️ albumin may exert direct toxic effects

38) The analyses of #UACR as a surrogate marker included 28 cohorts with nearly 700k participants & 41 #RCTs.
⬇️UACR reduction of 30% or eGFR slope ⬇️by 0.5 to 1.0mL/min/1.73m2 per year were associated with an HR of ∼0.7 for the clinical outcome of #ESKD in cohorts and trials


⬇️UACR reduction of 30% or eGFR slope ⬇️by 0.5 to 1.0mL/min/1.73m2 per year were associated with an HR of ∼0.7 for the clinical outcome of #ESKD in cohorts and trials



39) In summary #UACR is an underutilized diagnostic of great clinical utility in patients with #CKD & #T2D:
👉 It can be used to #diagnose & #stage CKD
👉Predict the risk of both #cardiovascular & #kidneydisease
👉Allows the risk to be communicated to patients & empower them
👉 It can be used to #diagnose & #stage CKD
👉Predict the risk of both #cardiovascular & #kidneydisease
👉Allows the risk to be communicated to patients & empower them
40) Furthermore, it
👉 Can be used to select patients with #residual #UACRelevations for guideline guided medical therapies (#SGLT2i & #MRAs) in the present
👉 Will continue to be used to enroll patients in #RCTs of investigational drugs in the future.
Measure it!
👉 Can be used to select patients with #residual #UACRelevations for guideline guided medical therapies (#SGLT2i & #MRAs) in the present
👉 Will continue to be used to enroll patients in #RCTs of investigational drugs in the future.
Measure it!
41) One last knowledge check: Our index patient is put on losartan 100mg. Six months later her eGFR was 40ml/min/1.73m2, potassium is 4.5 meq/l, UACR 300mg/gm creatinine & blood pressure is 130/80 mmHg. Which data should drive the next step in therapy for her #T2D & #CKD?
42) The correct answer is UACR! The patient has had a good response to a maximal dose of an ARB by experiencing a drop in her #UACR by 40%, but she still has considerable albuminuria putting her at risk for cardiovascular & kidney complications, i.e. a #SGLT2i, #MRA or both.
43) And you just earned 0.5hr 🆓CE/CME! Congratulations! Claim your certificate right now at cardiometabolic-ce.com/cardiorenal43/ & FOLLOW US while we are top of kidney . . . er, mind! @ChristosArgyrop thanks you for tuning in!
#FOAMed #nephtwitter #CardioTwitter #MedEd
#FOAMed #nephtwitter #CardioTwitter #MedEd
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter










