There are 2 main components to all procedures: cognitive aspects (indications, contraindications, complications) and technical aspects (steps of procedure, hand positioning, etc.).
Let’s start with the cognitive aspects.
Additionally, fluid can be removed to provide comfort. Also remember that fluid removal can alleviate abdominal compartment syndrome.
Contraindications. The closest thing to an absolute contraindication is cellulitis overlying the needle entry site. Bleeding risk must be individualized. Elevated INR from cirrhosis does not necessarily increase bleeding risk.
C. Circulatory dysfunction from fluid shift. Risk increases with removal of 5L or more. Data on colloid replacement following LVP is not robust, but it is commonly done. 6-8 g of albumin per L removed is reasonable.
D. Ascitic fluid leak. I don't like Z-track method because it requires additional hands in field, increasing risk of error/needle stick. And doesn't prevent something serious. Ostomy bag not a good solution. Pt should lie on opposite side for 1-2 h to allow tract to close.
Technical aspects.
Patient should be supine, up to ~20 degrees. Patient comfort is crucial to the success of your procedure. Your comfort and convenience is equally so. Make sure to adjust height of bed. Good lighting. Have an empty garbage can near by.
Finding needle entry site.
Use landmarks, percussion, and US to find your needle entry point. Flanks or sub-umbilical. Do not let US seduce you into a “beautiful” pocket right over the inferior epigastric. Always evaluate for vessels near your marked site.
I prefer small probe because it is precise. And precision is necessary for procedures. For smaller pockets, aim the probe in various directions to find the optimal approach and try to mimic it with your needle. Have pt roll toward ipsilateral side to help increase pocket.
Lidocaine does 4 things for you: 1) it numbs the patient, 2) it allows you to rehearse the steps of the procedure with a much smaller needle, 3) it tells you exactly how deep the peritoneal space is, 4) it informs you about the nature of the fluid. More on 3 and 4 below.
Body habitus and US provide a sense of the depth of the peritoneal space. The lidocaine needle provides exact depth. Why important?
If the needle is nonfunctional out of the kit or becomes clogged, you will never aspirate fluid and the tendency will be to keep going deeper, risking injury. If you know the depth of the pleural space, you will immediately recognize there is an issue w the equipment.
Why helpful to know the nature of the fluid before going in w larger catheter? Peace of mind. Many become anxious when bloody fluid begins draining into the collection bag. If the fluid was bloody with the small lidocaine needle (unlikely to do any damage), then rest easy.
Now that you have 1) numbed the patient, 2) rehearsed the procedure with a much smaller needle, 3) know exactly how deep the pleural space, and 4) know the nature of the fluid, you are ready to go in with the catheter/needle.
The moment you get flash of peritoneal fluid, you must go forward with both needle/catheter a few millimeters before threading catheter to ensure that it enters peritoneal space and not soft tissue.
Troubleshooting. Commonly bowel will obstruct the catheter and stop flow. Clamp tubing (or turn stopcock), manipulate the catheter by twisting/retracting to try to pull away from bowel, then release clamp. Repeat prn.
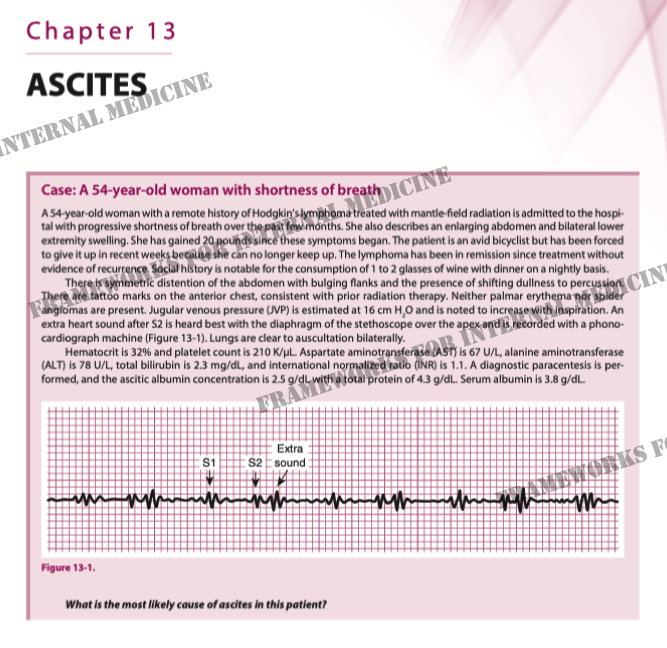
The end. Answer to the case?
(From: Frameworks for Internal Medicine: amazon.com/Frameworks-Int…)