Pulmonary vasodilators are generally not used for patients with pulmonary hypertension due to COPD, even if severe.
Why would that be?
#medtwitter #medthread #tweetorial
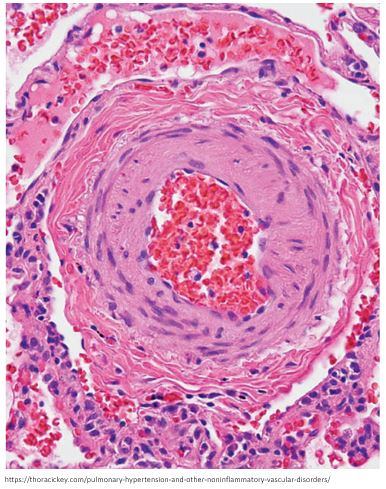
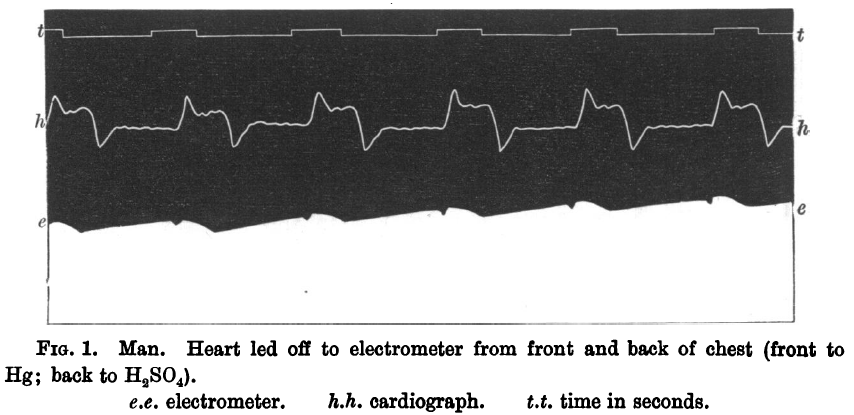
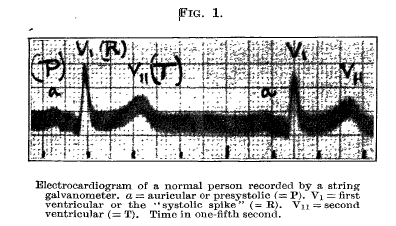
💥Let's first review the main source of pulmonary hypertension (PH) in the setting of COPD: hypoxic vasoconstriction
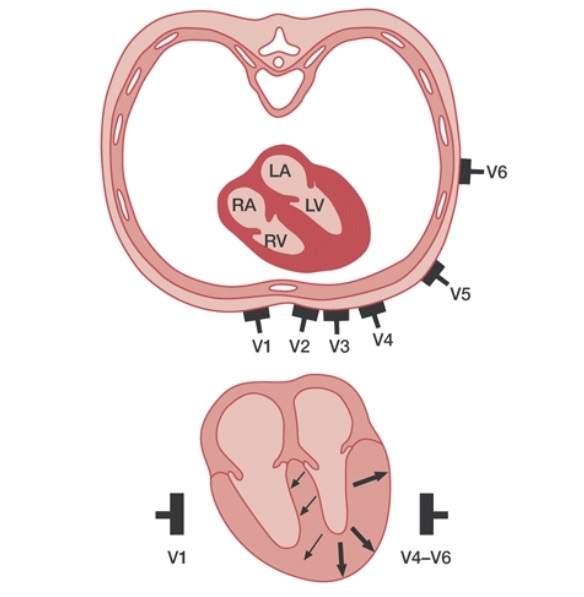
Areas of the lung that are poorly oxygenated have relative arteriolar vasoconstriction, in order to improve V/Q matching.
bit.ly/2QJxSD7
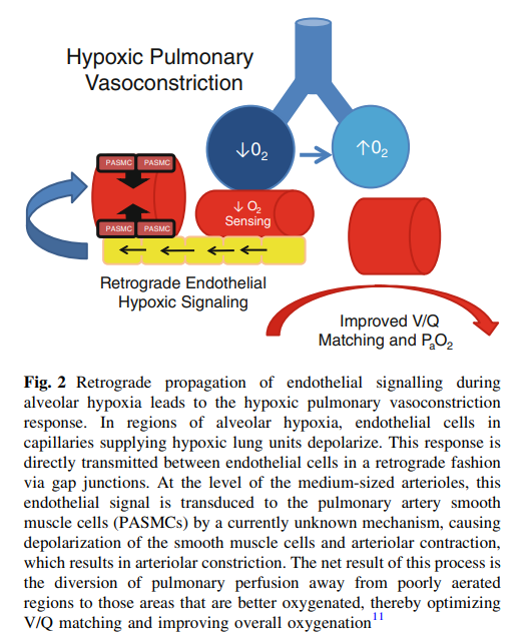
@tony_breu has previously covered the mechanisms of hypoxic vasoconstriction, but it involves endothelial mitochondria not sensing O2 and shutting down nitric oxide production.
💥Returning to our original question, why are pulmonary vasodilators generally avoided in patients with PH as a result of COPD?
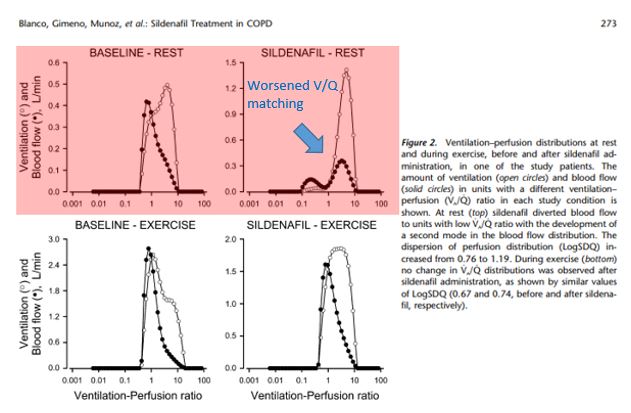
Let's take sildenafil, one of the most commonly used pulmonary vasodilators, as an example.
What happens when sildenafil is used in this setting?
Pulmonary pressures do decrease 👇
ncbi.nlm.nih.gov/pubmed/19875684

But at the same time V/Q mismatch worsens, due to unselective pulmonary vasodilation and loss of hypoxic vasoconstriction.
ncbi.nlm.nih.gov/pubmed/19875684
As a result, sildenafil use has been associated with either minimal or no benefit in PH patients with COPD.
Here's one example where it worsened A-a gradient, dyspnea, and quality of life 👇
ncbi.nlm.nih.gov/pubmed?term=22…
A poll:
💥Can you think of a way to administer pulmonary vasodilators that might get around this problem?
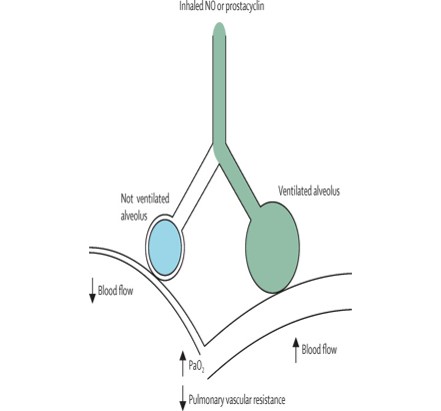
💡It turns out that giving pulmonary vasodilators via inhalation has the best evidence for safety/efficacy in the setting of COPD.
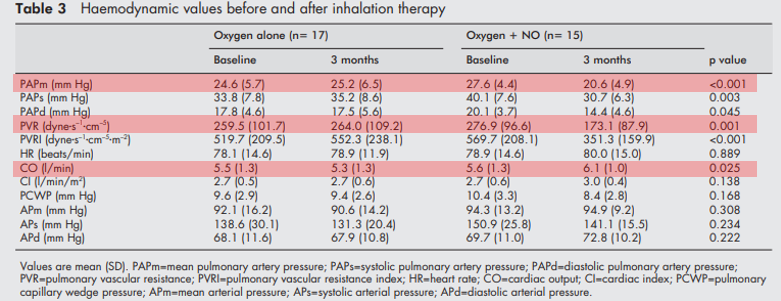
For example, inhaled nitric oxide improved pulmonary pressures and cardiac output without worsening O2 saturation.
ncbi.nlm.nih.gov/pmc/articles/P…
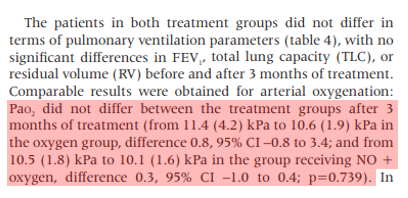
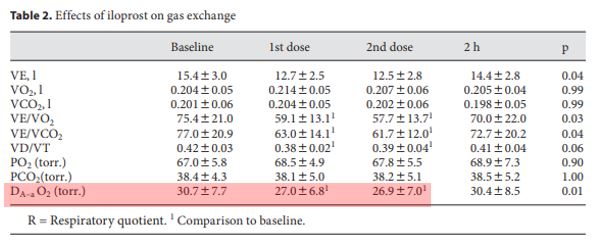
Another example: inhaled iloprost improved V/Q matching (as demonstrated by a decreased A-a gradient) and exercise tolerance.
ncbi.nlm.nih.gov/pubmed?term=19…
💡Physiologically this makes sense since inhaled medications are preferentially delivered to areas of the lung that are well-ventilated. Compensatory hypoxic vasoconstriction is therefore preserved.
ncbi.nlm.nih.gov/pubmed/27203510
Of course, plain old supplemental oxygen is effective as well at decreasing pulmonary pressures in hypoxemic patients with COPD.
ncbi.nlm.nih.gov/pubmed?term=67…
To summarize:
💡 Hypoxic vasoconstriction leads to PH in COPD. It is both compensatory and maladaptive.
💡 Pulmonary vasodilators can worsen V/Q mismatch in this setting by 🚫hypoxic vasoconstriction
💡Inhaled therapies avoid this issue, though data is limited