Does atelectasis cause post-operative fever?
I occasionally hear atelectasis listed in the differential diagnosis for early post-op fever (EPF) but this idea has never made much physiologic sense to me.
Let's explore this question in the following #tweetorial.
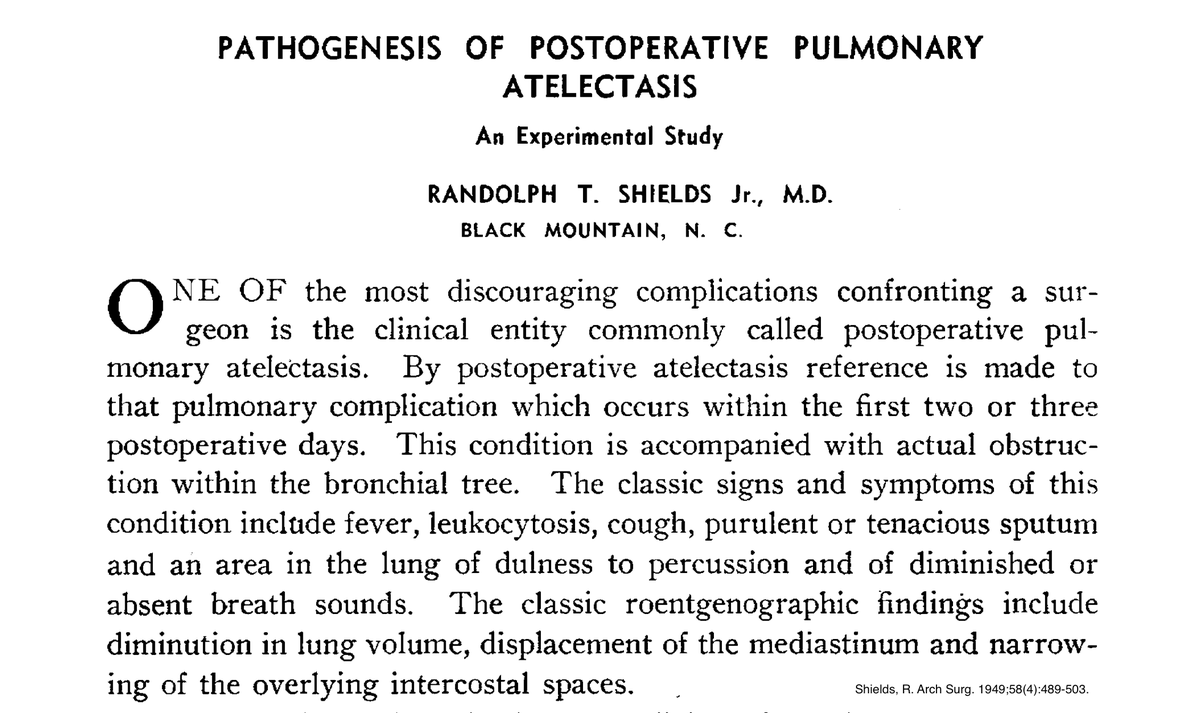
Despite its ubiquity, however, there is little published evidence to support this idea. One of the largest systematic reviews on the topic found that in 7 of 8 studies there was no significant association between atelectasis and early post-op fever.
PMID: 21527508
The only study to show any association suffered from methodological flaws since it compared fever on post-op day (POD) 1 or 2 with atelectasis looked for on POD 4.
Using fever as a diagnostic test for atelectasis in this manner was poor (sensitivity of 25%).
PMID: 3350683
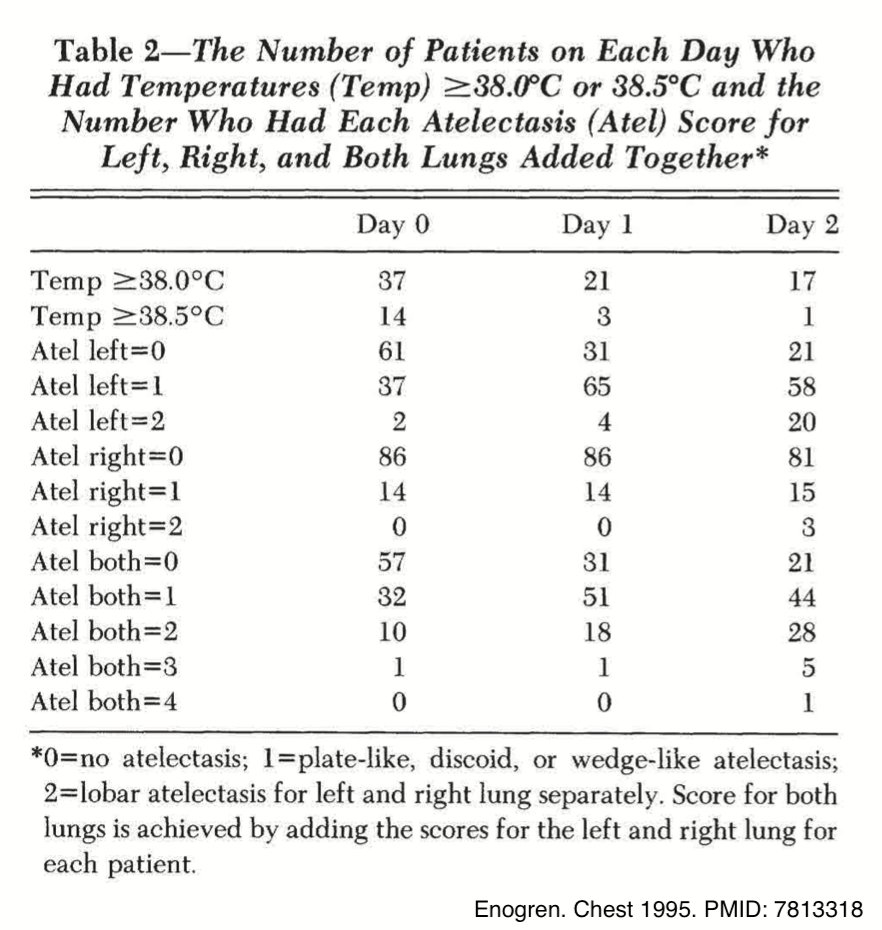
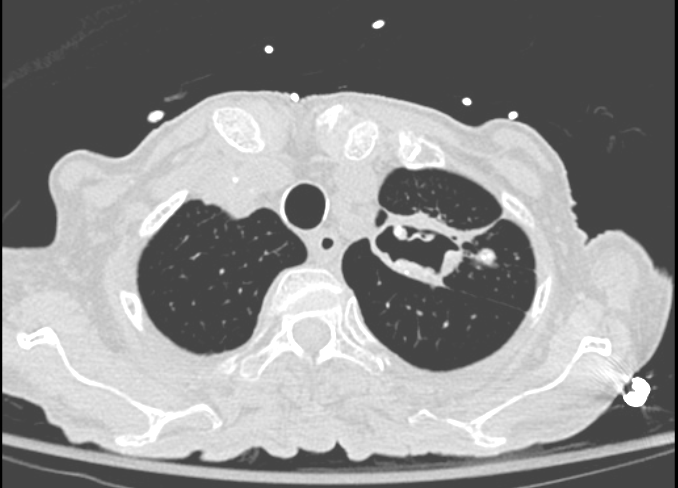
Another study of 100 cardiac surgery patients evaluated with daily chest x-rays and continuous bladder thermometry revealed that both fever and atelectasis are common after surgery, but were actually inversely related.
PMID: 7813318
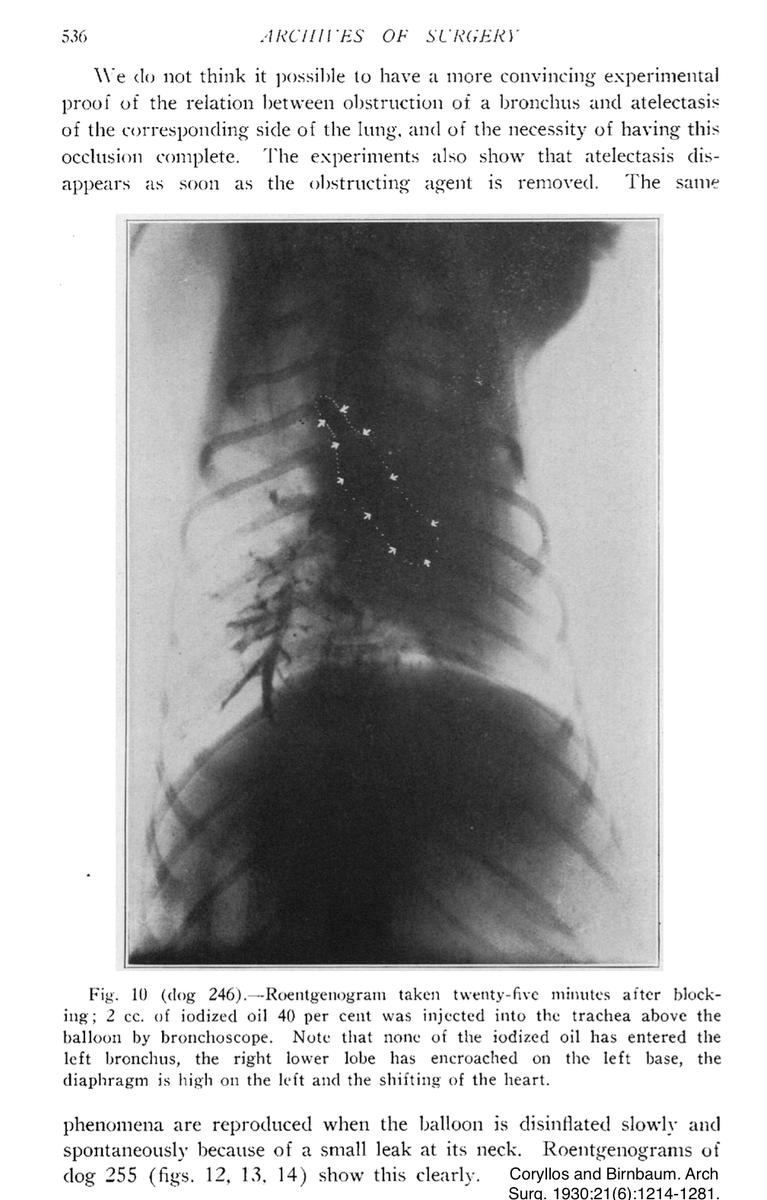
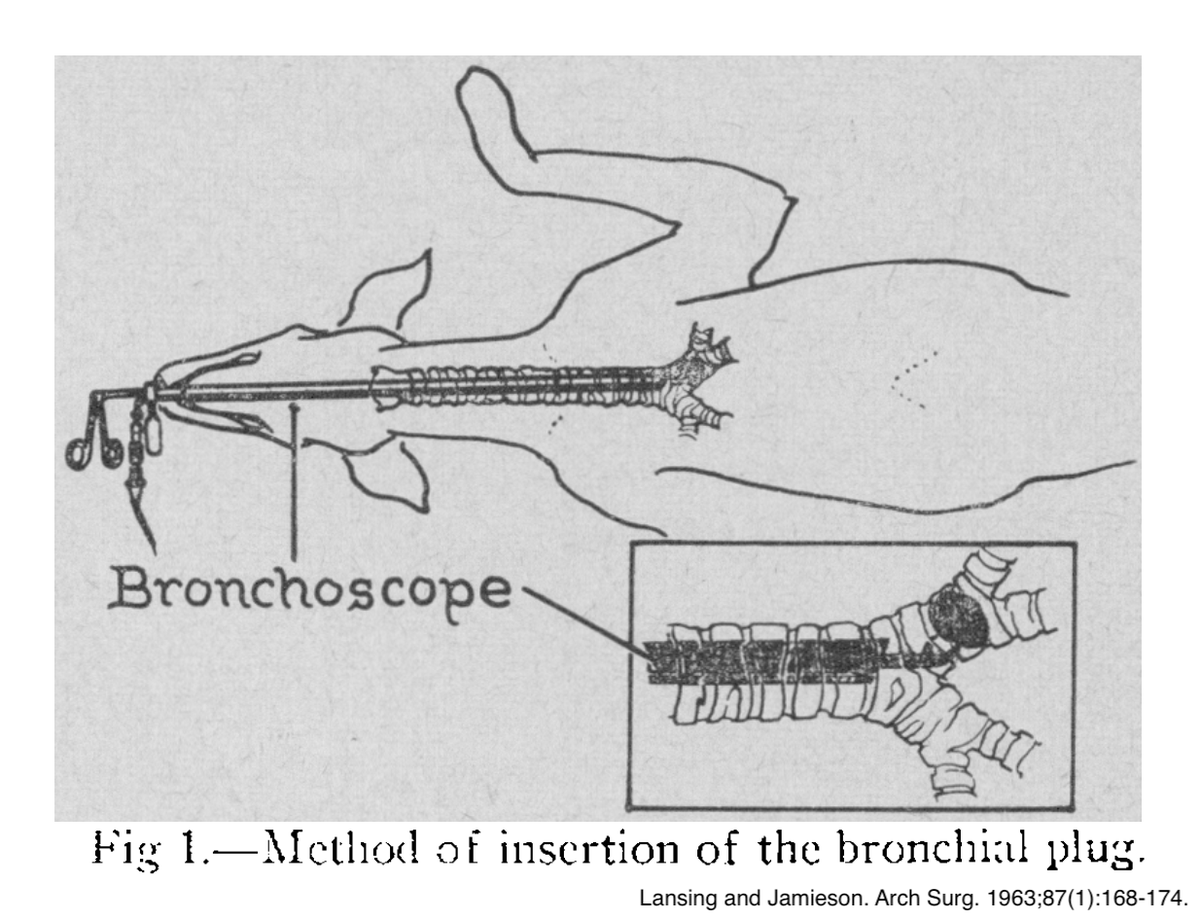
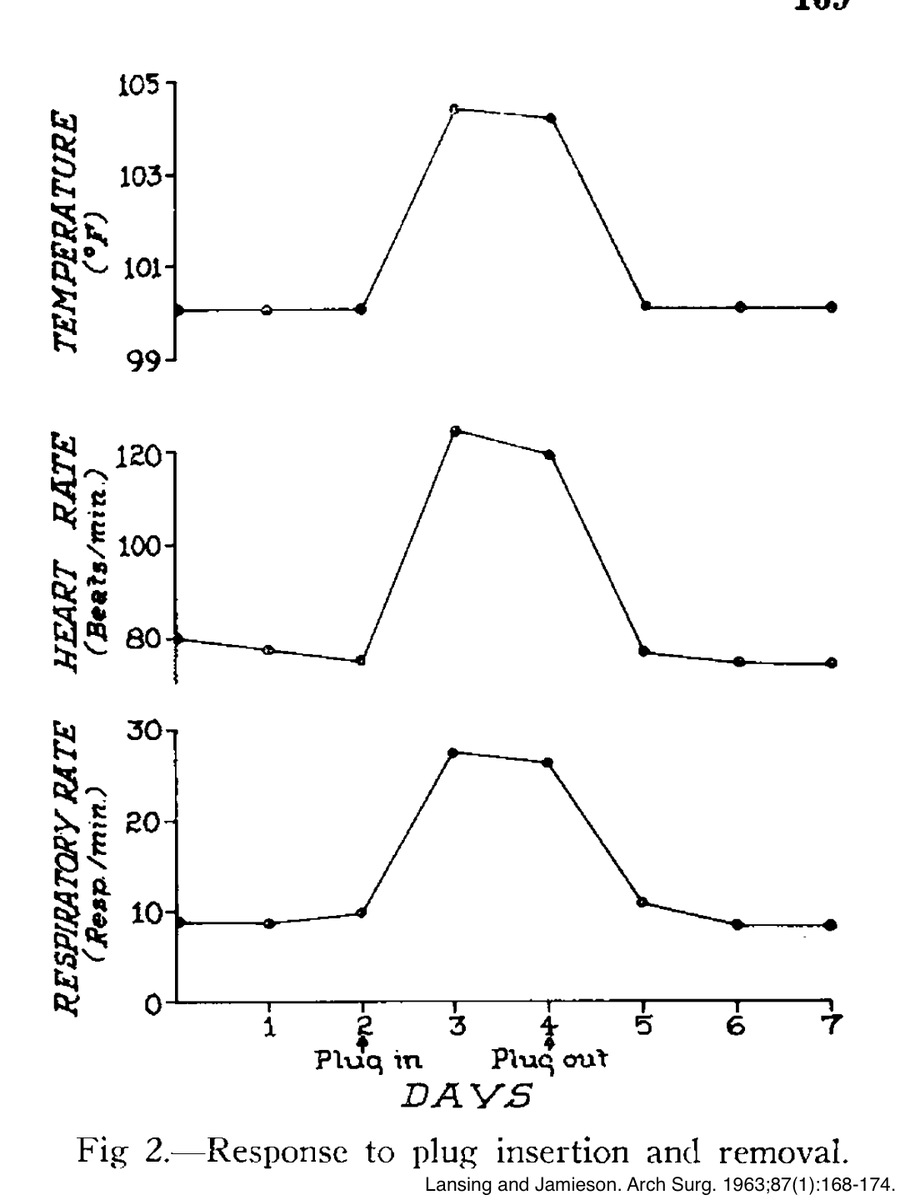
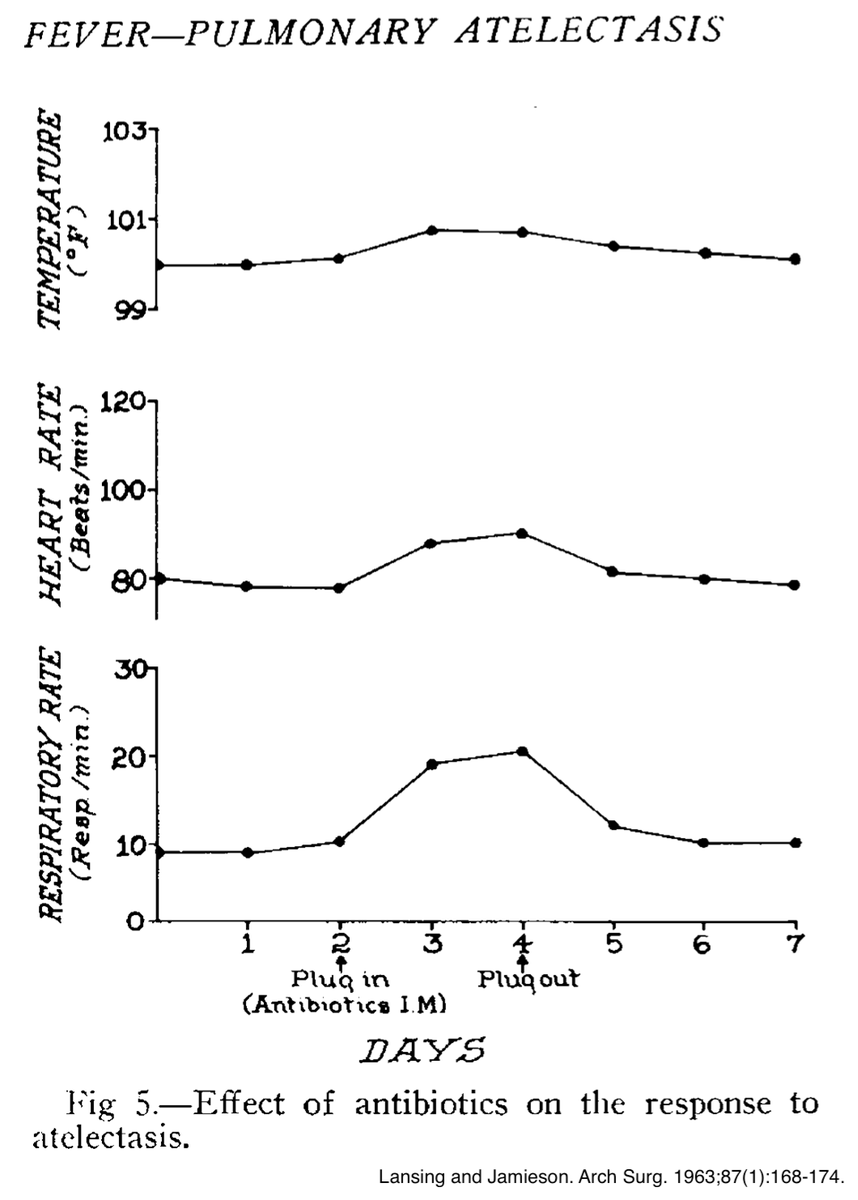
In another modern study, rats undergoing ligation of a main stem bronchus were found to have ⬆️ IL-1/TNF levels. This is difficult to interpret as the tissue injury from a thoracotomy and infracting lung tissue likely confounds any affect of atelectasis alone.
PMID: 8457016
So if atelectasis does not directly cause fevers, is there a more plausible explanation for noninfectious early post-operative fever?
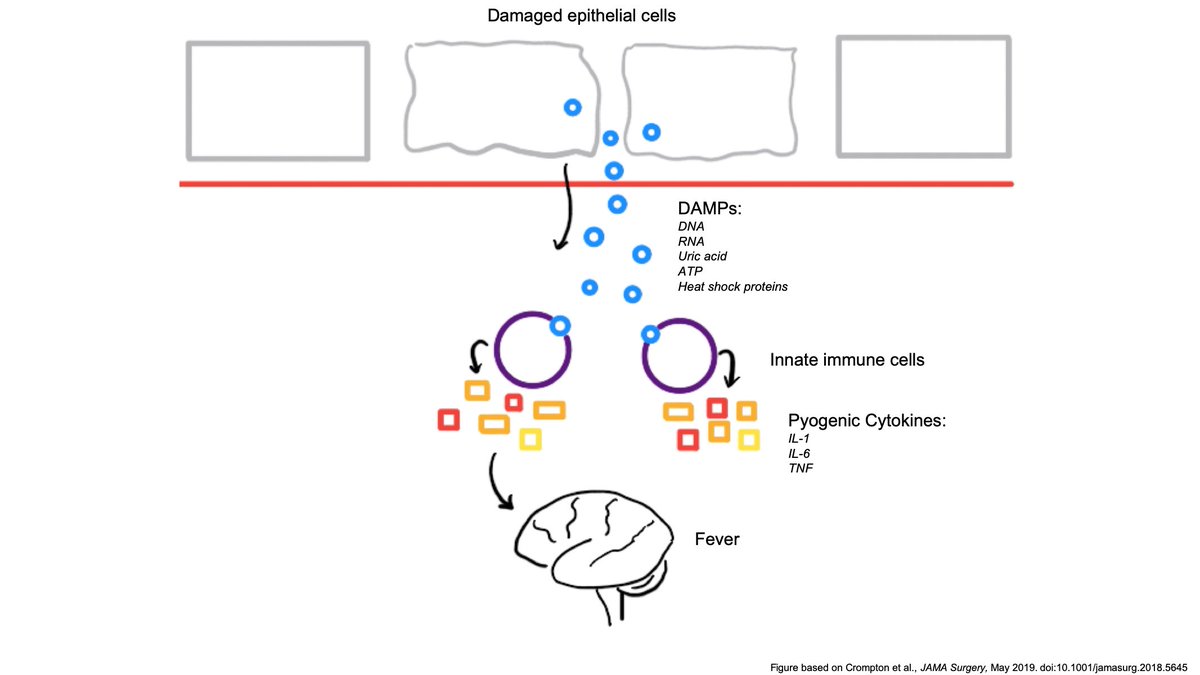
Enter every internist's favorite hand-waiving explanation: cytokines!
To be more specific, it may be that the "danger model of immunity", as proposed in a recent opinion paper by Crompton et al. in JAMA Surgery, may provide an alternative explanation for EPF.
PMID: 30840058
While not definitive, this model intuitively makes more physiologic sense. It may provide a satisfactory explanation for the phenomenon of non-infectious EPF and help to relieve the existential discomfort most doctors feel when a fever has no obvious infectious cause.
I'll conclude with a few 🔑 takeaways:
🔘Fever and atelectasis are both common after surgery but are poorly correlated
🔘Animal studies of atelectasis and fever are plagued by confounding
🔘 The danger model of immunity may provide a plausible alternative explanation for EPF
ncbi.nlm.nih.gov/pubmed/21527508
ncbi.nlm.nih.gov/pubmed/3350683
ncbi.nlm.nih.gov/pubmed/7813318
jamanetwork.com/journals/jamas…
jamanetwork.com/journals/jamas…