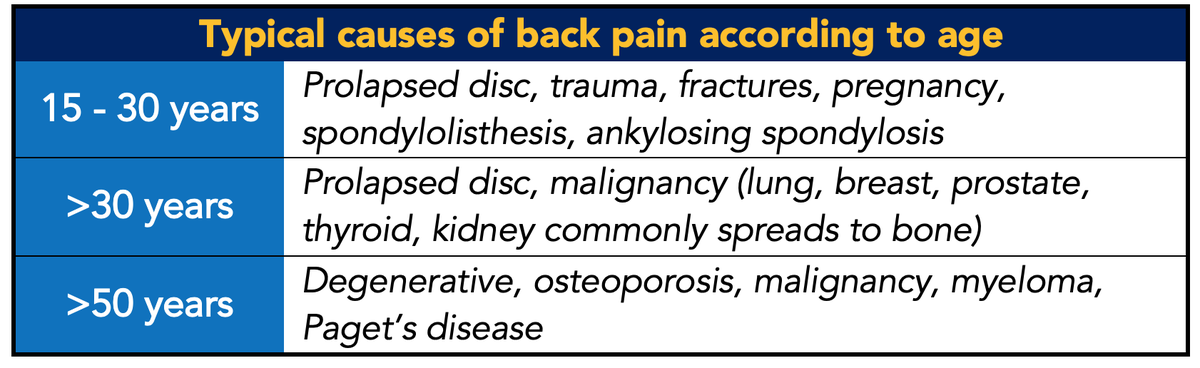
Tell me, what's a myotome?👀 #BBCES
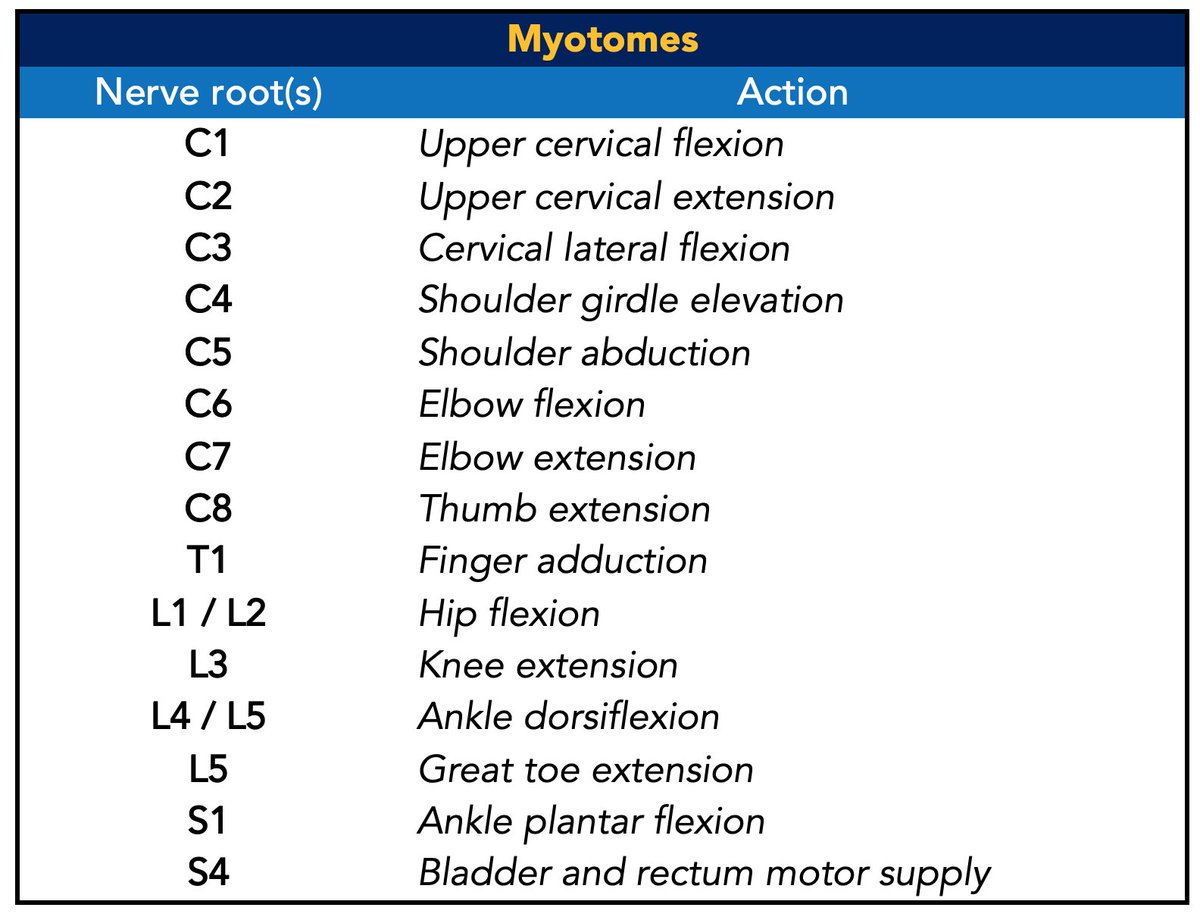
Image: bit.ly/2wHETfS
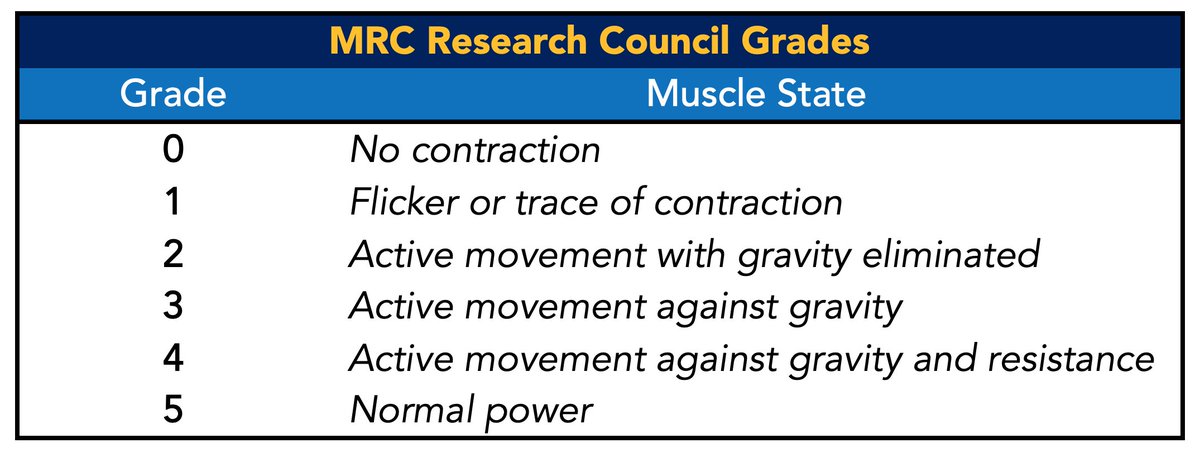
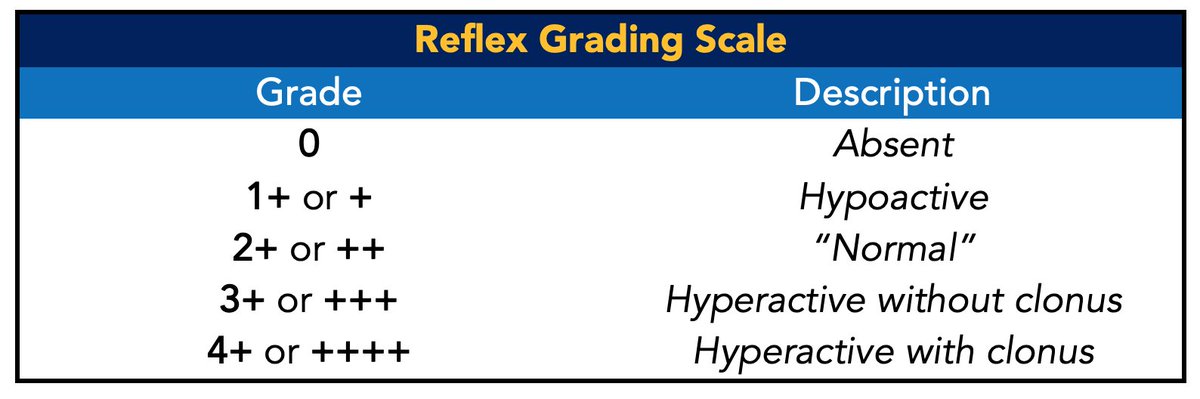
Do you know what root mediates the Ankle jerk reflex?
#BBCES
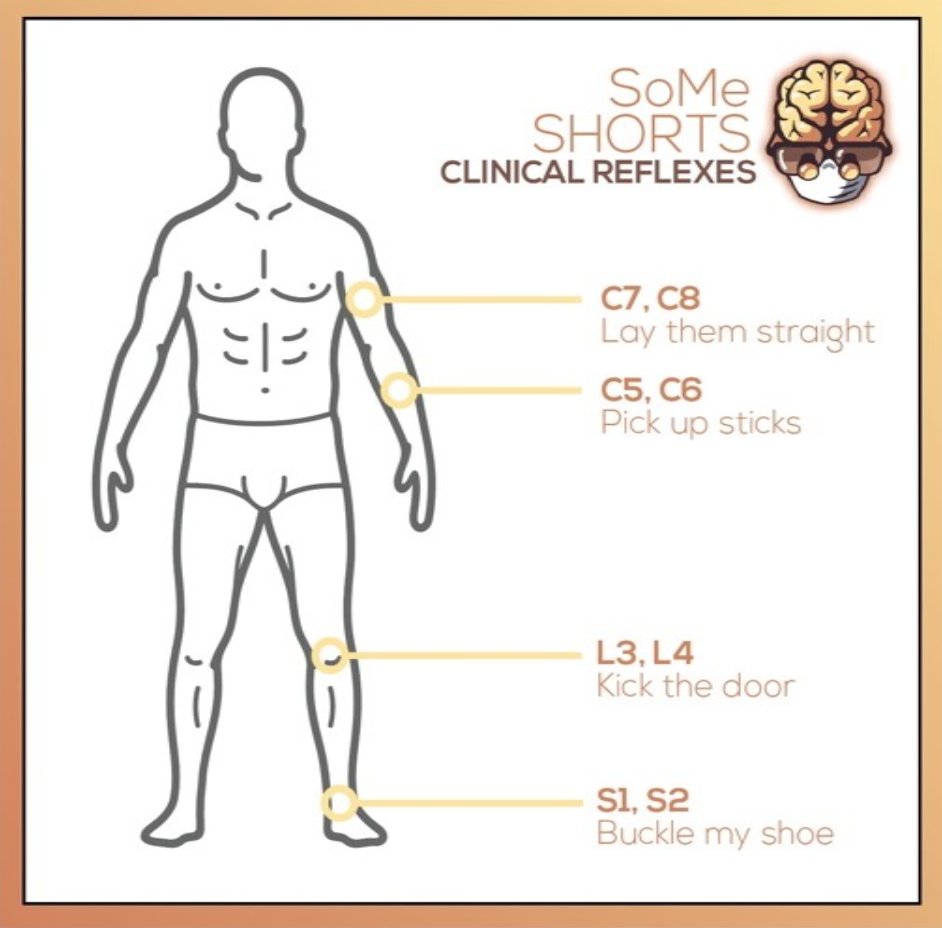
Are there any other tests you’d like to perform? #BBCES
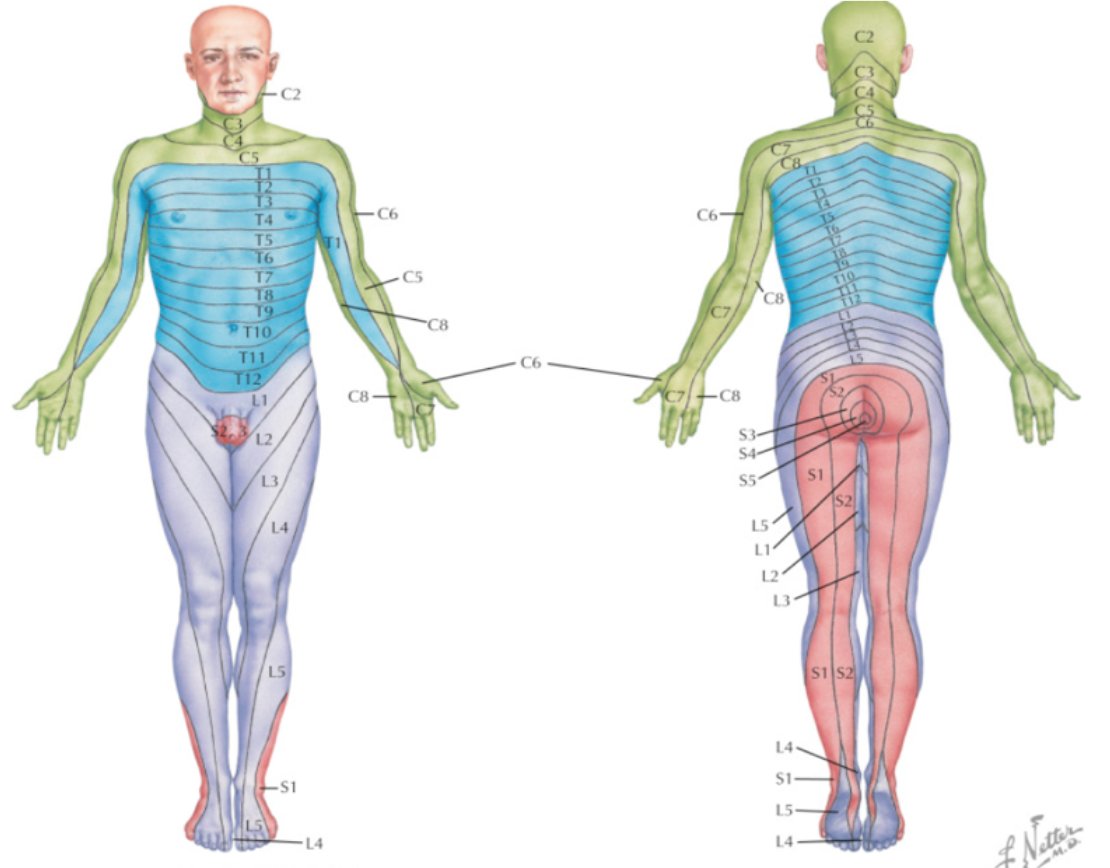
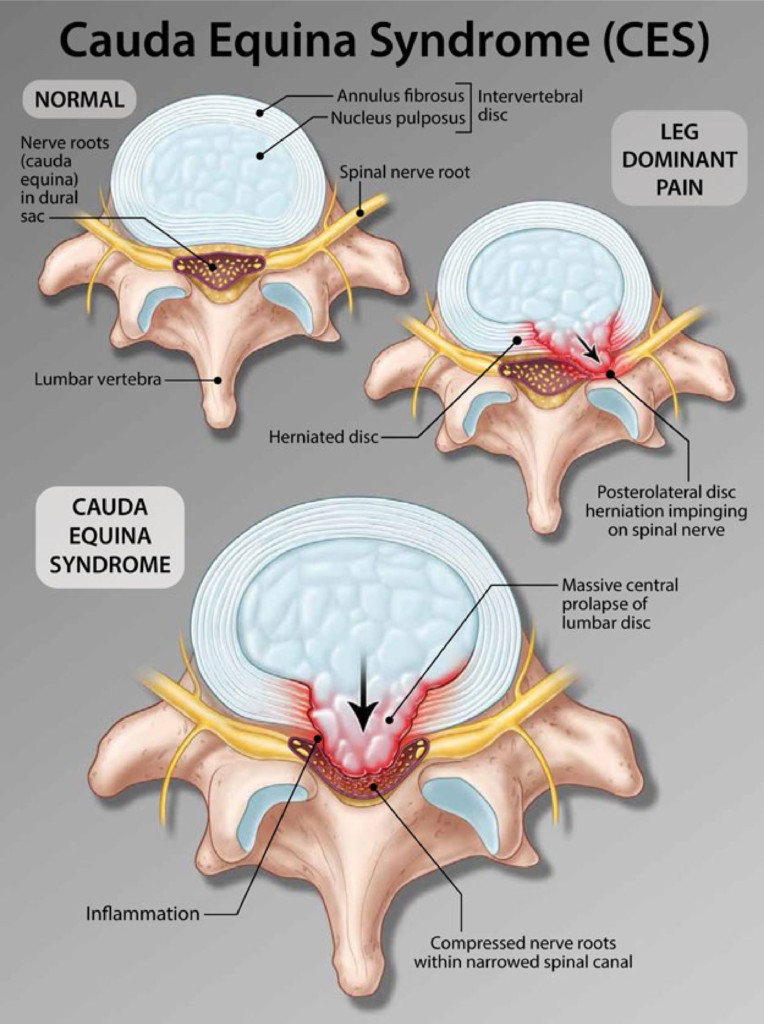
The adult spinal cord terminates at the level of the L1–L2 vertebrae. The lower distal part of the spinal cord is known as the conus medullaris, and its tapered end forms the filum terminale... #BBCES
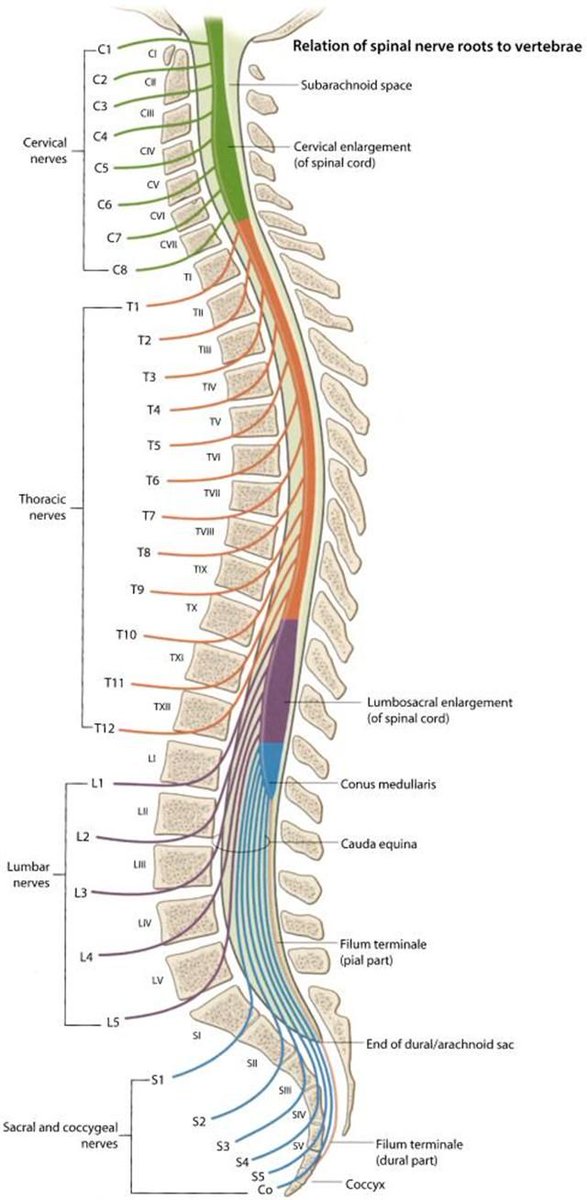
Now we understand the function of these nerves, lets go onto how cauda equina typically presents. #BBCES
Image: bit.ly/39aw0tT

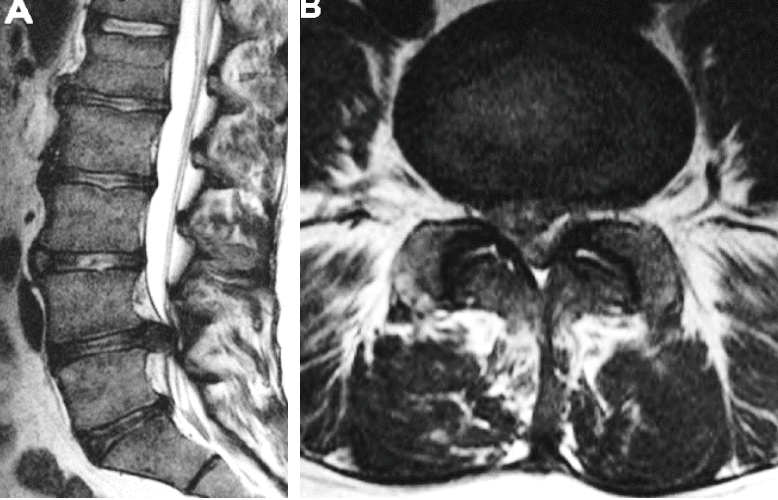
An MRI scan is performed. Can you identify anything from the images below?
#BBCES
What're your next steps in the management of this patient?
#BBCES
We really hope you enjoyed today's CbD, and hope you come back for the next one.
Huge thanks to @aswinchari for moderating!
Keep an eye out for our next Live CbD... feedback form in the next tweet!
👉👉👉bit.ly/3c8hLYo
Do be sure to enter your e-mail at the end of the survey as we'll be sending out all CbD certificates so far over the next few weeks.
Survey closes tomorrow at midday!