Inspired by this tweet by @TheMenacheryLab, I reached out to the wonderful colleagues at the @serimmune to see if the other mutations found in the B.1.1.7 variant would evade antibody responses generated by the wild type #SARSCOV2. (1/n)
https://twitter.com/TheMenacheryLab/status/1341460341293723650
According to this report, B.1.1.7 harbors non-synonymous mutations in the following viral genes, resulting in truncation, deletions and amino acid changes. Would these mutations result in evasion from antibodies generated by wild type virus? (2/n)
virological.org/t/preliminary-…
virological.org/t/preliminary-…

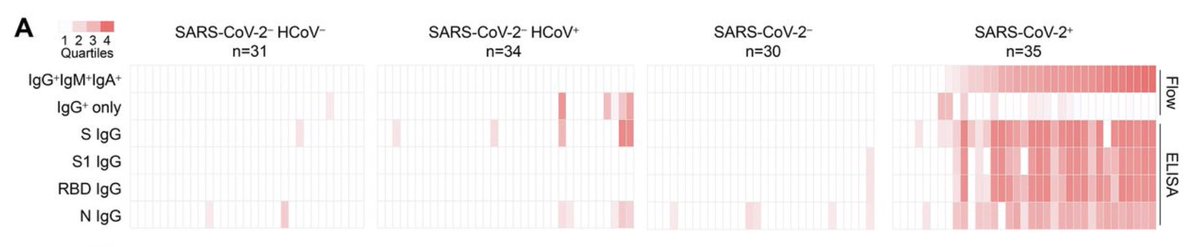
To probe this possibility, @serimmune used their technology platform based on bacterial display peptide libraries, next generation sequencing & machine learning to reveal antibody reactivity against WT and B.1.1.7 viral antigens. (3/n)
serimmune.com/technology.html
serimmune.com/technology.html
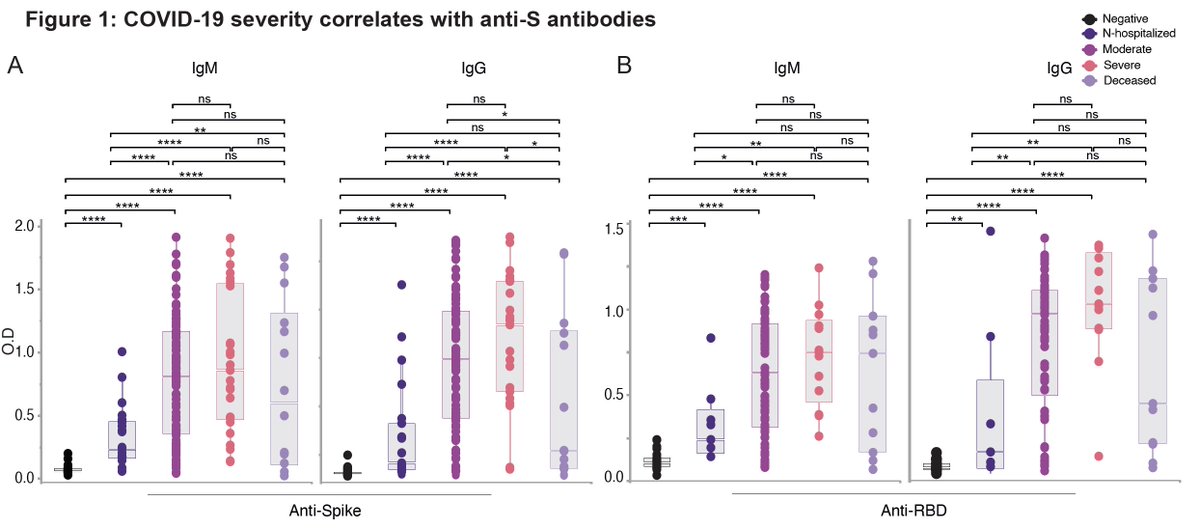
From 579 COVID patients, they looked for antibody reactivity to regions (linear epitopes) of the spike and nucleoprotein containing mutations. (4/n)
For the antibodies against the spike, dominant linear epitopes are indicated in red at the bottom. For more about this, please read
medrxiv.org/content/10.110…
None of the mutations (orange) are within these dominant epitopes.
(5/n)
medrxiv.org/content/10.110…
None of the mutations (orange) are within these dominant epitopes.
(5/n)

Zooming in on the spike mutations, either there was no Ab binding (del69/70, N501Y, T716I, S982A, D1118H) or del144, N501Y, A570D, and P681H resulting in only 2/579 having a reduction in PIWAS antigen scores, which reflects the peak epitope signal along the entire antigen. (6/n) 

A caveat of these analyses is that we are only looking at linear epitopes. Mutations might result in conformational epitope changes that affect Ab binding. However, people make multiple antibodies to the spike protein. (7/n)
science.sciencemag.org/content/370/65…
science.sciencemag.org/content/370/65…
As RT above, @TheMenacheryLab has shown functionally that the N501Y mutation in the RBD does not evade existing antibodies’ ability to block replication. (8/n)
So overall, while B.1.1.7 may have enhanced transmission capabilities, it does not appear to evade antibody responses. Antibodies induced by prior infection and vaccines should provide protection. For more read this thread by @hayneswa 👇🏽 (9/n)
https://twitter.com/hayneswa/status/1343983411795427330?s=20
It does not mean that viral variants that evade antibodies won’t arise in the future. This is why viral genome surveillance effort is so crucial. (End)
https://twitter.com/trvrb/status/1340409968818671616?s=20
PS. @serimmune has uploaded these analyses on preprint server. Once live I will post the link.
• • •
Missing some Tweet in this thread? You can try to
force a refresh