What aspects of antibody responses determine the outcome of #COVID19? In this new preprint by @carolilucas @sneakyvirus1 et al., we found that the early timing of antibody response (before 14 days of symptom) in infected person is key to recovery. (1/n)
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
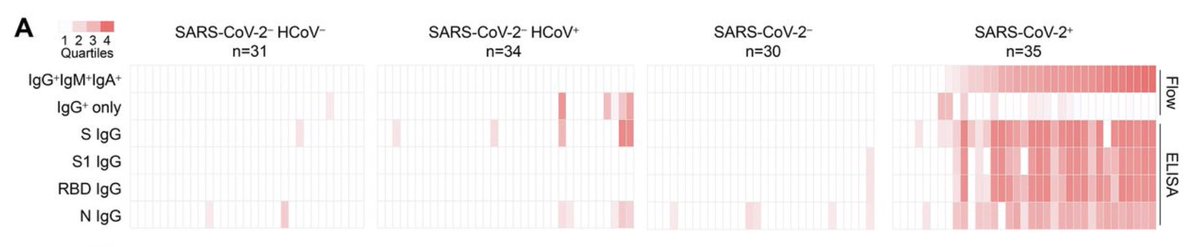
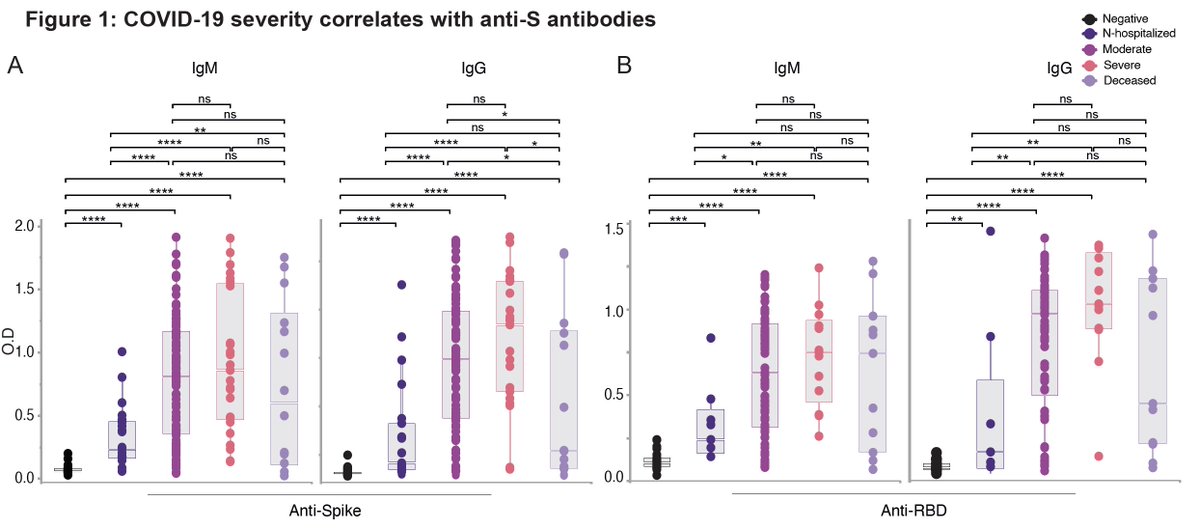
As others have shown, we found that antibody levels from COVID patients correlated with disease severity.
journals.plos.org/plospathogens/…
wwwnc.cdc.gov/eid/article/26…
However, patients with lethal COVID did not have the highest level of anti-S or anti-RBD antibodies. What’s going on? (2/n)
journals.plos.org/plospathogens/…
wwwnc.cdc.gov/eid/article/26…
However, patients with lethal COVID did not have the highest level of anti-S or anti-RBD antibodies. What’s going on? (2/n)
To understand better the features of antibody responses in patients who died vs. survived, we compared their time course. We found a delay in antibody responses in lethal disease. We also noted patients with very high neutralizing Ab (HN) with very early antiviral Abs. (3/n) 

An important study by Dr. Galit Alter’s group also showed delayed antibody responses in lethal COVID. (4/n)
pubmed.ncbi.nlm.nih.gov/33207184/
pubmed.ncbi.nlm.nih.gov/33207184/
In patients who died of COVID, viral load remained high over the course of disease, while surviving patients eventually controlled the virus. High neutralizers had very low viral load. (5/n) 

What about neutralizing antibodies? Similar to anti-S and anti-RBD IgG, neutralizing antibodies also developed late in non-survivors. Also people with lethal COVID did not develop neutralizing Abs at highest titers. (6/n) 

Of all the COVID patients in our study, 54% made high anti-S IgG. Of those, 89% of patients made detectable neutralizing Abs - about half made NAb before 14 days of symptom, and other half after. (7/n) 

Patients who developed neutralizing antibodies before 14 days of symptom eventually recovered, while those who made NAb after 14 days developed severe disease and sustained higher viral load. (8/n) 

These data showed that the timing of antibody response, and not how much antibody a person makes, during COVID19 determines whether you recover from disease.
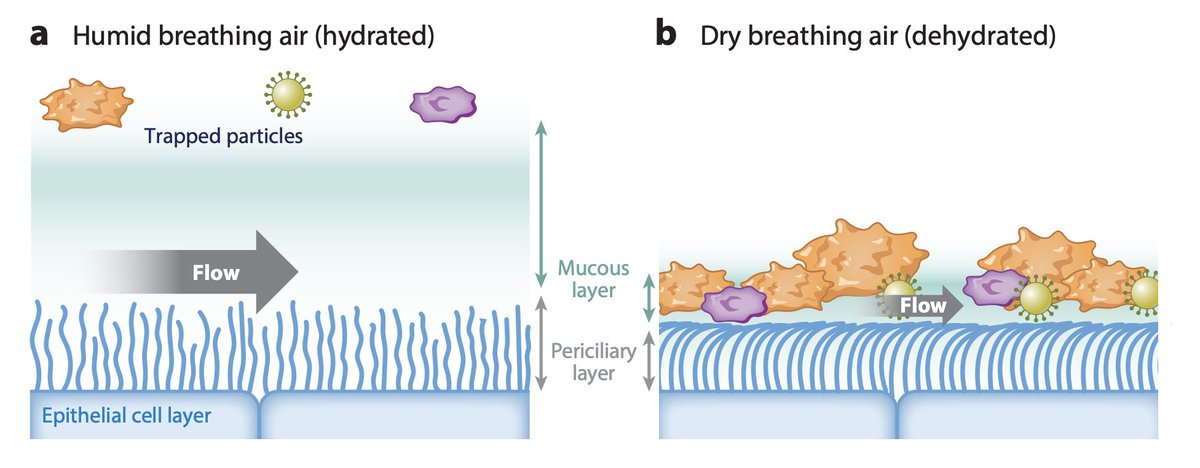
Why would late Abs not work? It’s possible that virus somehow becomes resistant by hiding in inaccessible tissues. (9/n)
Why would late Abs not work? It’s possible that virus somehow becomes resistant by hiding in inaccessible tissues. (9/n)
It is also notable that pathogenic antibodies develop in severe COVID, such as afucosylated IgG1. (10/n)
nature.com/articles/s4159…
science.sciencemag.org/content/early/…
nature.com/articles/s4159…
science.sciencemag.org/content/early/…
More practical implication is that therapy such as monoclonal antibodies is likely to work only if used early during #SARSCoV2 infection.
This study was again a result of teamwork, headed by @carolilucas, @sneakyvirus1 in collaboration with the awesome Yale IMPACT team 🙏🏼 (end)
This study was again a result of teamwork, headed by @carolilucas, @sneakyvirus1 in collaboration with the awesome Yale IMPACT team 🙏🏼 (end)
• • •
Missing some Tweet in this thread? You can try to
force a refresh