New exciting collaboration work with @Aaronmring lab reveals diverse and functional autoantibodies in #COVID patients.
Our findings provide clues for why COVID affects many organs, induce range of symptoms that are long lasting.
Thread (1/n)
medrxiv.org/content/10.110…
Our findings provide clues for why COVID affects many organs, induce range of symptoms that are long lasting.
Thread (1/n)
medrxiv.org/content/10.110…
How do we look for autoantibodies against a wide range of self antigens? The @aaronmring lab developed a high-throughput autoantibody discovery technique called Rapid Extracellular Antigen Profiling (REAP) against 2,770 extracellular and secreted proteins "exoproteome" 💪🏼 (2/n) 

A large fraction of #COVID patients had autoantibodies to multiple self antigens. The more severe the disease, more autoantibodies they had.(3/n) 

So what are the targets of these autoantibodies? It turns out to be many. Some antibodies bound to interferons, chemokine and cytokines, while others bound to proteins expressed on the surface of immune and non-immune cells. (4/n) 

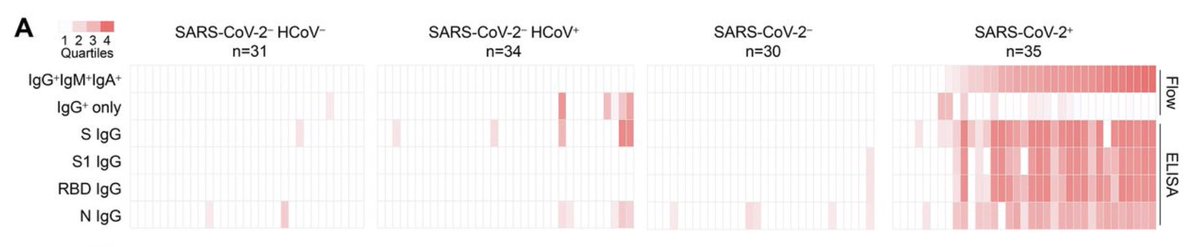
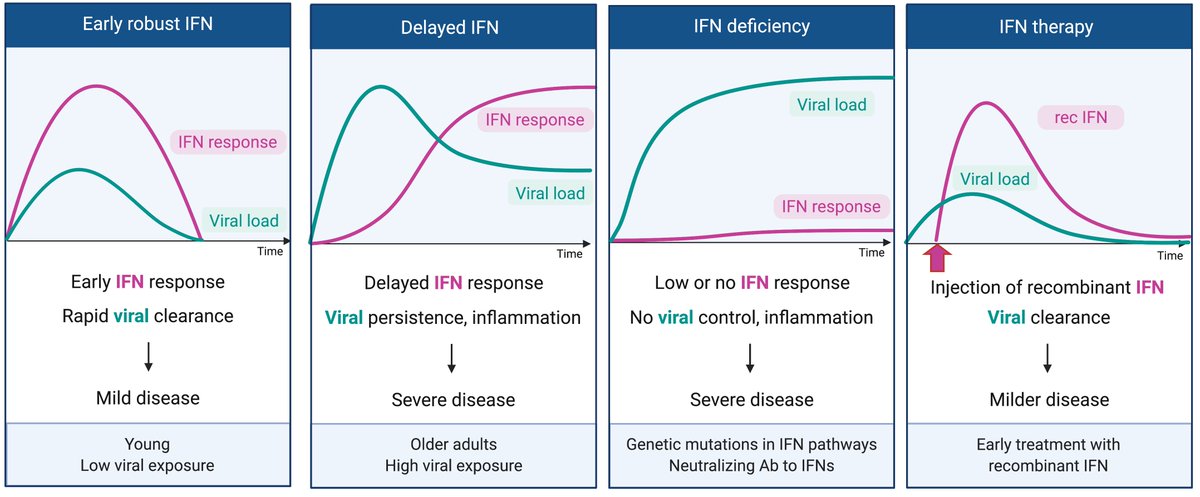
Here are the autoantigens that are detected by antibodies in COVID patients. Columns represent patients. Rows are antigens. Notice the frequency of anti-interferon antibodies in severe COVID patients! Very reminiscent of this study👇🏽 (5/n)
science.sciencemag.org/content/370/65…
science.sciencemag.org/content/370/65…

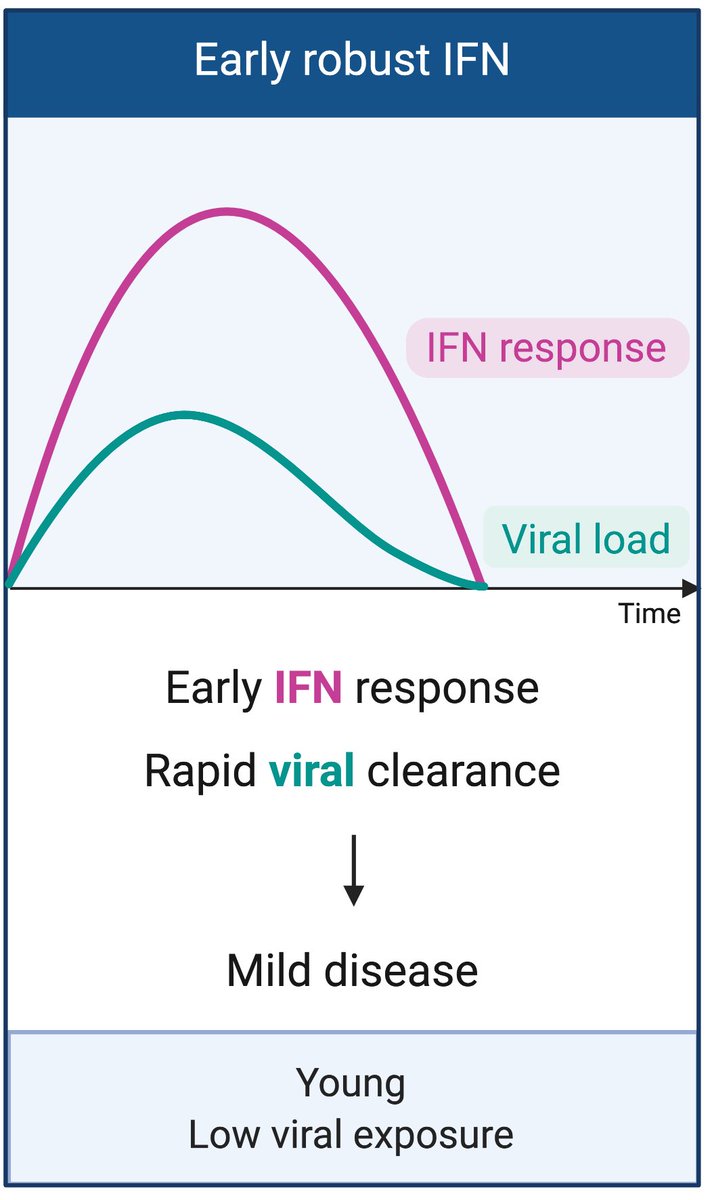
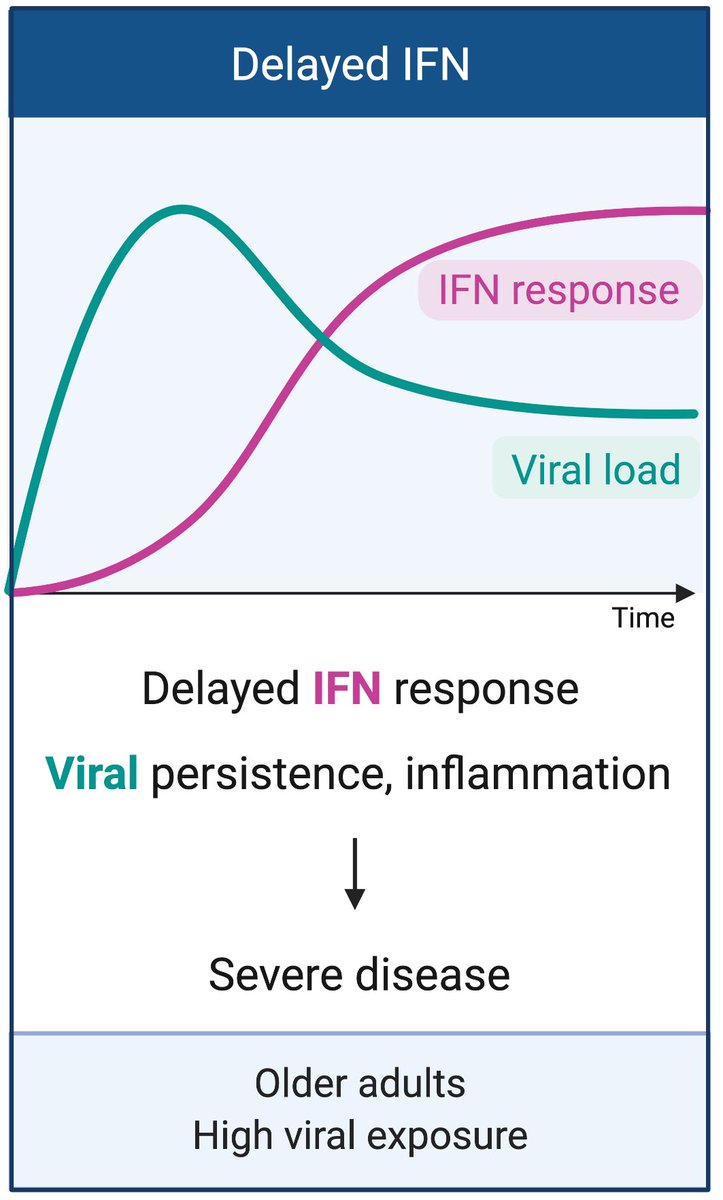
These autoantibodies to IFN-I are likely functional - people who have them were unable to control viral load, compared to those without - matched for comparable average age, sex, and disease severity. (6/n) 

In addition to IFN-I, there were many other immune proteins that become target of antibody attack. IL-1α/β, IL-6, GM-CSF, IL-18Rβ, and Leptin (LEP). Chemokine autoantibody targets included CXCL1, CXCL7, CCL2, CCL15, CCL16, and the chemokine decoy receptor ACKR1. (7/n)
Surface autoantigens on immune cells also found; NKG2D ligands (RAET1E/L, ULBP1/2), NK cell receptors NKG2A/C/E (KLRC1/2/3), B cell-expressed proteins (CD38, FCMR, FCRL3, CXCR5), T cell expressed proteins (CD3E, CXCR3, CCR4), and myeloid expressed proteins (CCR2, CD300E).(8/n)
These Abs appear to be functional in vivo. People who had anti-B cell antibodies had very low number of circulating B cells and very low IgM response against RBD. (9/n) 

One patient with autoantibodies against CD3E (a component of the T cell receptor complex) had intact B and NK cell compartments but dramatically reduced levels of
CD4 T cells, CD8 T cells, and NKT cells in the blood. (10/n)
CD4 T cells, CD8 T cells, and NKT cells in the blood. (10/n)

Another way we validated the function of the autoantibodies is through the use of mouse model. Anti-IFNAR or anti-IL-18 Ab treatment of mice rendered them more susceptible to disease and death after #SARSCoV2 challenge. (11/n) 

In addition to immune-related antigens, we also found antibodies to various tissue-specific antigens in organs like the central nervous system, vascular, connective tissues, liver, GI tract..etc. Such antibodies could drive damage in target tissues. (12/n) 

Some of the autoantibodies were found from the very beginning of analysis, while others were induced during the course of study. Others declined in their levels over time. (13/n) 

There are many unanswered questions. How long do these autoantibodies last? What damage do they cause? How are they induced? Do they occur in #LongCovid?
Finally, this was a heroic effort by many, led by @Eric_Y_Wang @tianyangmao @sneakyvirus1 Yile Dai and Yale IMPACT team 👏🏼
Finally, this was a heroic effort by many, led by @Eric_Y_Wang @tianyangmao @sneakyvirus1 Yile Dai and Yale IMPACT team 👏🏼
• • •
Missing some Tweet in this thread? You can try to
force a refresh