My first tweet of 2021 is going to be about 1 dose vs. 2 dose vaccine. I have tweeted in the past of the immunological advantages of a 2 dose vaccine. However, given the enhanced transmission variants on the rise, we need a modified strategy. (1/n)
theatlantic.com/science/archiv…
theatlantic.com/science/archiv…
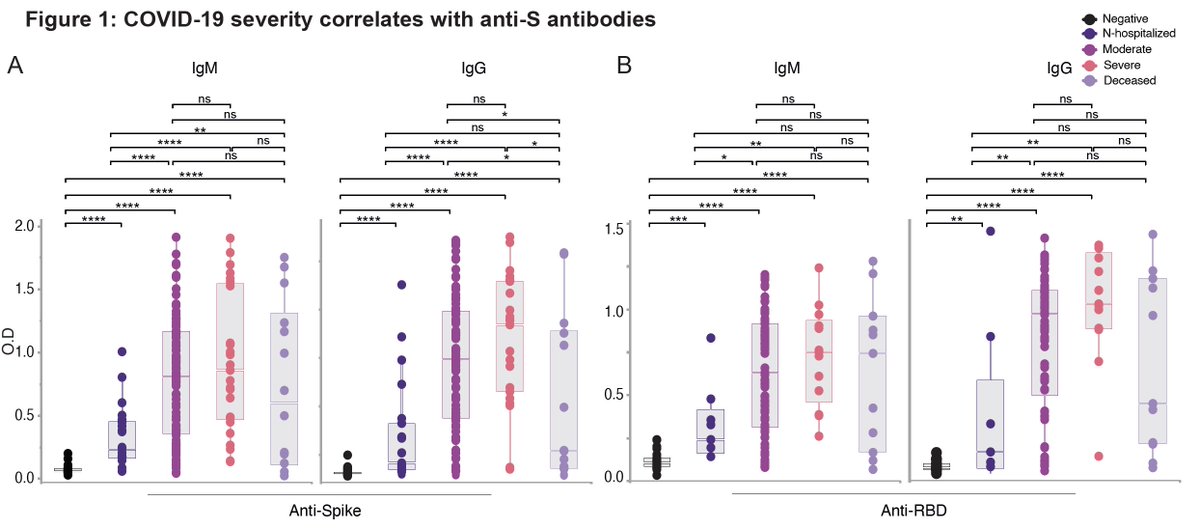
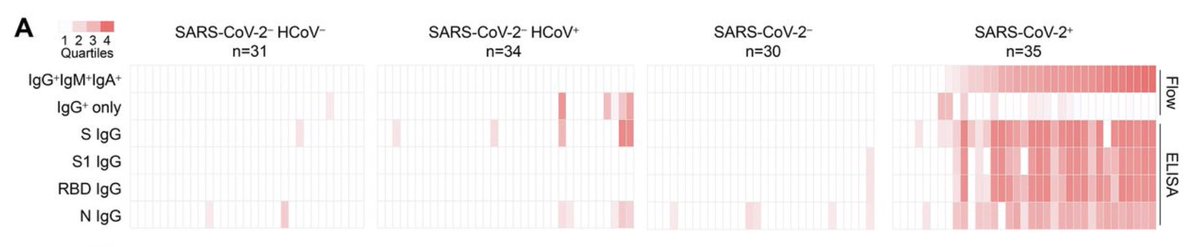
We typically give vaccines in more than one dose to increase 1) quantity, 2) quality, 3) longevity of antibody responses. This holds true for most vaccines including mRNA vaccines. Here is what I tweeted about this before. (2/n)
https://twitter.com/VirusesImmunity/status/1336323024786653187?s=20
However, the 2 dose vaccine with limited number of vaccine means only half the people getting vaccinated at this time. If the virus is spreading slowly, we want to do the right thing and give the most vulnerable 2 doses and others to wait. (3/n)
Unfortunately, the vaccine roll-out is much slower than we had expected. This means that even the vulnerable have to wait for months to get their 2 shot vaccines. (4/n)
statnews.com/2020/12/29/pub…
statnews.com/2020/12/29/pub…
In the meantime, the virus is mutating and spreading faster. A mutant virus with 50% ⬆️ in transmission kills a lot more people than a mutant with 50% ⬆️ in lethality. A must read thread from @AdamJKucharski 👇🏽 (5/n)
https://twitter.com/AdamJKucharski/status/1343567425107881986?s=20
So how effective is a single dose vaccine? We do not know for sure, but for at least a month or more, a single shot mRNA vaccines should provide ~90% protection (>14 d post vaccination). This is from the Moderna VRBPAC Briefing Document. (6/n) 

Whether a single dose vaccine provide protection from severe COVID is not clear due to small sample size and short follow up duration. (7/n) 

I am still a proponent of 2 dose vaccine but given the urgency, we can delay the 2nd dose until more vaccines become available. I know many others have been saying this all along, but it was the B.1.1.7 variant transmission rate that did it for me. (8/n)
https://twitter.com/jcbarret/status/1344607063658405888?s=20
The good thing about the mRNA vaccine is that if you prime with it, you can boost with other types of vaccines (viral vectored, DNA, mRNA…etc). In the future, a mixed prime boost vaccine strategies can be tested to provide long term protective immunity. (9/n)
So how long can we safely wait in between 1st and 2nd doses? If you look at the childhood vaccine schedules, some boosters are given months to years apart. For COVID vaccine, booster after a few months might be okay. (10/n)
cdc.gov/mmwr/preview/m…
cdc.gov/mmwr/preview/m…

Well I guess things are already moving along faster than I can type (but @EricTopol types faster than the news) in both UK and US. Posting my thread now before it is completely obsolete (end).
https://twitter.com/EricTopol/status/1345080202964029442?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh