
1/ In context of extra precautions against new COVID variants, some new questions pop up about #masks.
Article by @cwarzel @zeynep asks/answers some good questions to start. Other thoughts in a 🧵, e.g. N95s, fit (Tw7+ ⬇️), when to replace (Tw25 ⬇️), etc.
nytimes.com/2021/01/29/opi…
Article by @cwarzel @zeynep asks/answers some good questions to start. Other thoughts in a 🧵, e.g. N95s, fit (Tw7+ ⬇️), when to replace (Tw25 ⬇️), etc.
nytimes.com/2021/01/29/opi…
2/ Countless recent articles w/ interviews from relevant experts imploring people to still take mask-wearing & overall airborne COVID health seriously.
One of many, here by @skbaer w/ broad contribution. (Tw33 below has link to a compilation of more).
buzzfeednews.com/article/skbaer…
One of many, here by @skbaer w/ broad contribution. (Tw33 below has link to a compilation of more).
buzzfeednews.com/article/skbaer…
3/ Many good arguments recently towards motivating broader use of #bettermasks, i.e. #N95s. So if not using already, consider.
See e.g. this editorial by @j_g_allen: washingtonpost.com/opinions/2021/…
Or this opinion-piece by a group of excellent scientists:
See e.g. this editorial by @j_g_allen: washingtonpost.com/opinions/2021/…
Or this opinion-piece by a group of excellent scientists:
https://twitter.com/HuffmanLabDU/status/1354129198319693825?s=20
4/ One of the simplest overviews on practical aspects of this topic of upgraded masks/respirators (i.e. N95s, KN95s, double-masking) is a brief video interview also with @j_g_allen:
https://twitter.com/j_g_allen/status/1354608059771973648
5/ Also a great overview on the importance & physical science principles behind face masks for COVID-19 protection was written recently by @MonicaGandhi9 & @linseymarr. It's a very short, easy read; worth your time.
cell.com/med/fulltext/S…
cell.com/med/fulltext/S…
6/ This is one of the best videos to explain how masks work (especially focused on #N95s); by @minutephysics.
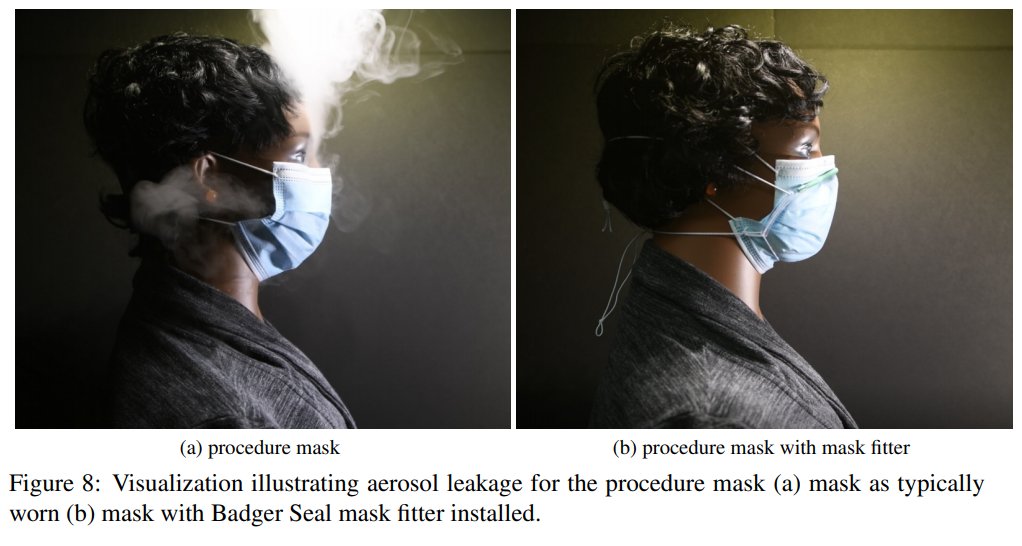
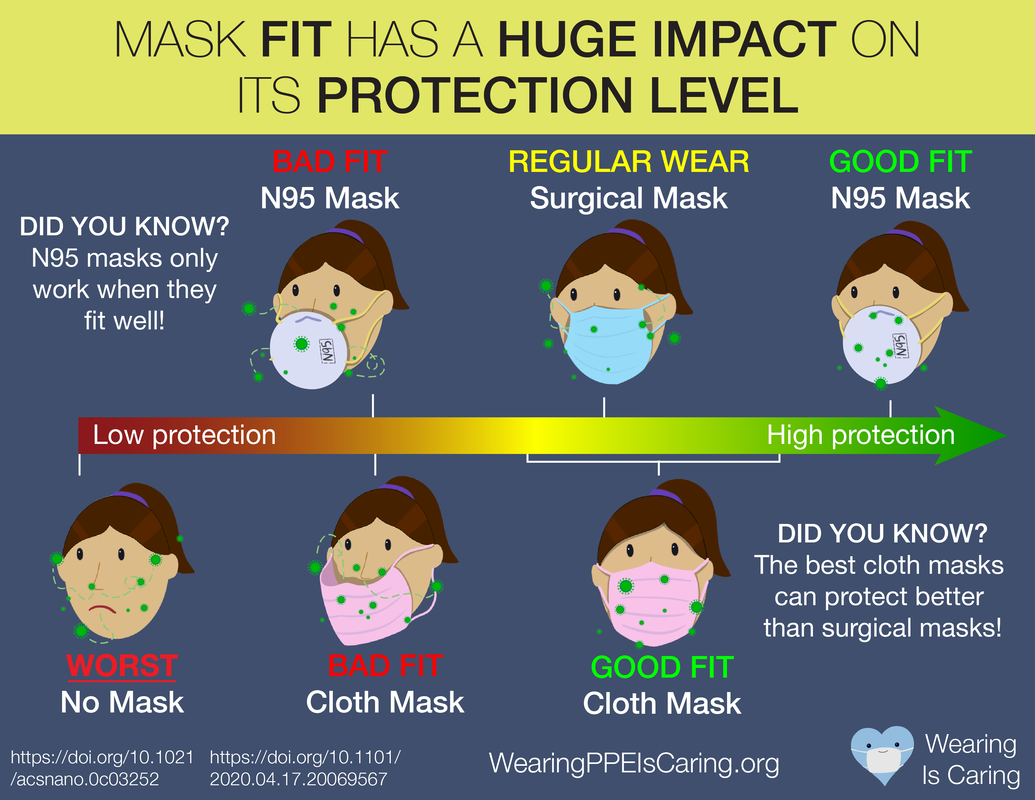
7/ To achieve adequate health benefit from masks, keep in mind that both FILTRATION & FIT are critical.
I frequently share this video that beautifully demonstrates the importance of fit. Notice what happens to the aerosol with a poorly fitting mask:
I frequently share this video that beautifully demonstrates the importance of fit. Notice what happens to the aerosol with a poorly fitting mask:
8/ Scientific motivation for better mask FIT quality is deep & wide. Three of *many*:
I.e. poor fit of surgical masks = insufficient & danger to HCWs
Goldberg et al:
Prof. @CappaSnappa: researchsquare.com/article/rs-142…
Rothamer et al (⬇️): medrxiv.org/content/10.110…
I.e. poor fit of surgical masks = insufficient & danger to HCWs
Goldberg et al:
https://twitter.com/HuffmanLabDU/status/1355580532814278661
Prof. @CappaSnappa: researchsquare.com/article/rs-142…
Rothamer et al (⬇️): medrxiv.org/content/10.110…
9/ Also *lots* of research & resources on mask/filtration quality. 🧵 not meant to be comprehensive, but e.g.:
Pan et al: medrxiv.org/content/10.110…
Clapp et al: jamanetwork.com/journals/jamai…
Interactive graphs by @smogdr: jv.colostate.edu/masktesting/
Lit: examine.com/topics/coronav…
Pan et al: medrxiv.org/content/10.110…
Clapp et al: jamanetwork.com/journals/jamai…
Interactive graphs by @smogdr: jv.colostate.edu/masktesting/
Lit: examine.com/topics/coronav…
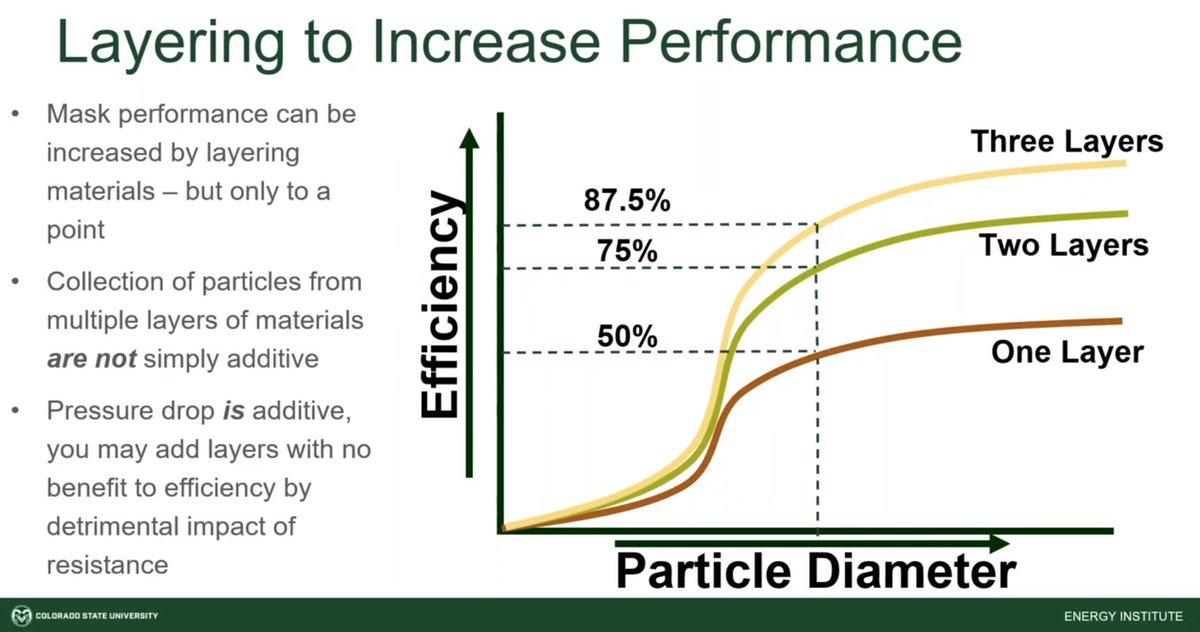
10/ One strategy to improve filtration/fit combo could be to double-mask. This can be effective (webinar from Sept by @Smogdr w/ test data: ).
But make sure that the added layers don't interfere with your ability to breath smoothly through the material.
But make sure that the added layers don't interfere with your ability to breath smoothly through the material.
11/ Another broad strategy to improve mask FIT is to add a #maskbrace to hold on a looser mask w/ gaps (i.e. surgical). It's usually a piece of rubber that makes sure no aerosol sneaks in or out through gaps at your face, nose, chin.
E.g. Rothamer et al.: medrxiv.org/content/10.110…
E.g. Rothamer et al.: medrxiv.org/content/10.110…
12/ Here is a short video interview with @katherinepasem1, a designer of the @FixTheMask brace:
You can buy these braces at fixthemask.com.
https://twitter.com/abc7kristensze/status/1356387694348177408
You can buy these braces at fixthemask.com.
13/ OR you can use the free template provided by @FixTheMask to make your own #maskbrace for improved fit.
fixthemask.com/products/v2-di…
fixthemask.com/products/v2-di…
14/ This is a nice video explaining by @FixTheMask filtration in general and the importance of good mask fit:
15/ @linseymarr (aerosol & mask-testing expert) recently shared her impressions after having made one of these DIY mask braces:
https://twitter.com/linseymarr/status/1354099221687918592
16/ Another good #maskbrace option is the Badger Seal developed through @UWMadEngr, which can be purchased for ~$10 or made yourself using their linked instructions & videos.
making.engr.wisc.edu/mask-fitter/
making.engr.wisc.edu/mask-fitter/
17/ No matter the mask, only as effective as it's ability to seal to face around both nose & mouth.
If hard to breath through a #mask, it is too restrictive/thick. Air (& aerosol) will always escape mask. If air exits via gaps rather than THROUGH layer(s), mask is ineffective!
If hard to breath through a #mask, it is too restrictive/thick. Air (& aerosol) will always escape mask. If air exits via gaps rather than THROUGH layer(s), mask is ineffective!
18/ CDC doc gives some tips related to checking the seal of your mask/respirator:
- Make sure material sucks in or blows out sufficiently when breathing
- Fogging glasses or gaps formed are signs of poor fit
(Note: for COVID, never use a mask w/ valve!)
cdc.gov/niosh/docs/201…
- Make sure material sucks in or blows out sufficiently when breathing
- Fogging glasses or gaps formed are signs of poor fit
(Note: for COVID, never use a mask w/ valve!)
cdc.gov/niosh/docs/201…
19/ This is a 4-min video also shows how to do a user seal-check on a #N95 mask/respirator.
Keep in mind that this was developed for occupational safety and not wrt general public health, but most principles still apply.
(HT @DavidLKeating)
Keep in mind that this was developed for occupational safety and not wrt general public health, but most principles still apply.
(HT @DavidLKeating)
20/ Some other links with various tips & hacks in terms of mask fit:
Via @NebraskaMed: nebraskamed.com/COVID/13-mask-…
O'Kelly et al: medrxiv.org/content/10.110…
CDC: cdc.gov/coronavirus/20…
Via @lisa_iannattone:
Article by @mgodoyh: npr.org/sections/healt…
Via @NebraskaMed: nebraskamed.com/COVID/13-mask-…
O'Kelly et al: medrxiv.org/content/10.110…
CDC: cdc.gov/coronavirus/20…
Via @lisa_iannattone:
https://twitter.com/lisa_iannattone/status/1357513295448702984
Article by @mgodoyh: npr.org/sections/healt…
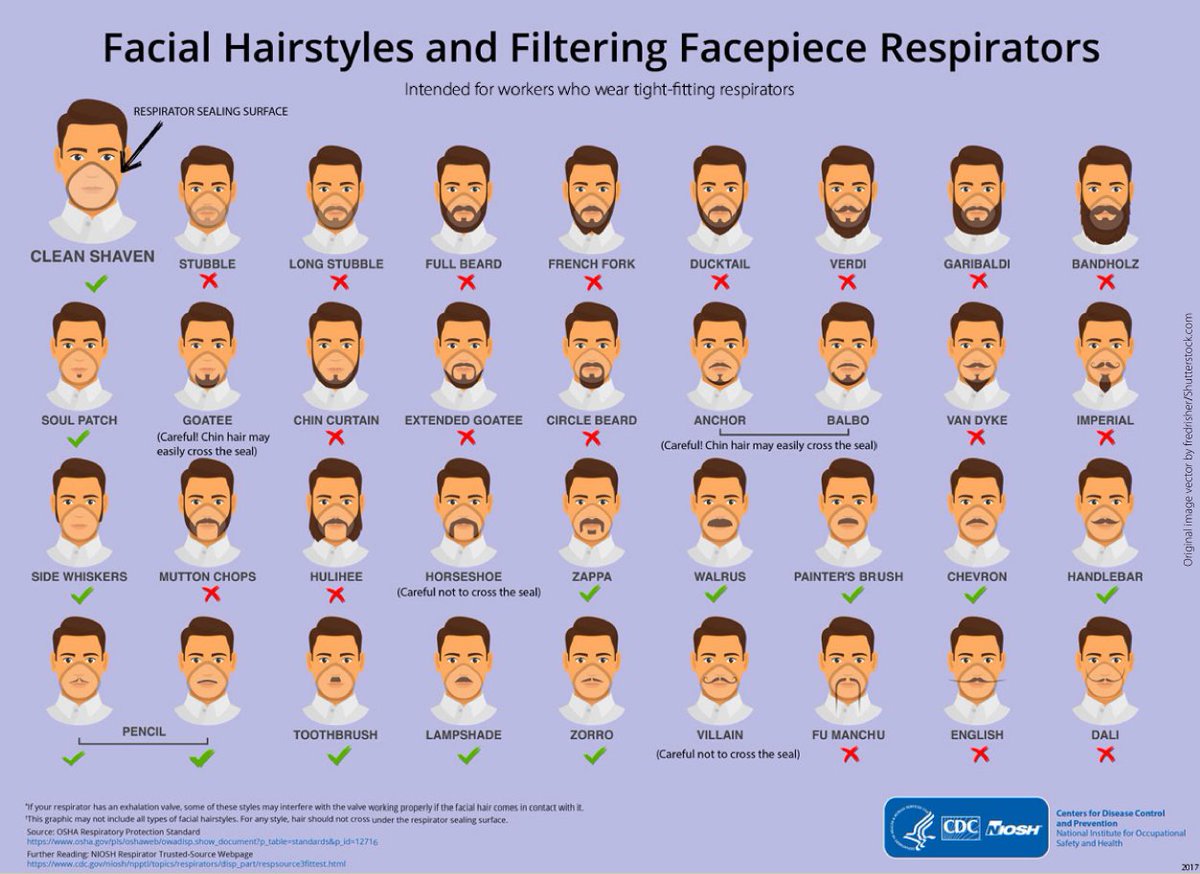
21/ Also important to note that facial hair/beards makes it very difficult/impossible to get a good fit to your face and so efficiency of the #mask is reduced.
Check out this awesome CDC/NIOSH chart.
Be a #walrus, not Dali!
cdc.gov/niosh/npptl/pd…
Check out this awesome CDC/NIOSH chart.
Be a #walrus, not Dali!
cdc.gov/niosh/npptl/pd…
22/ Related; you have probably heard of the "#candletest" for testing filtration quality (i.e. blow through mask; candle flame out = bad). I personally don't like this, b/c may just mean air/aerosol escapes through gaps. E.g.:
npr.org/sections/goats…
https://twitter.com/linseymarr/status/1357365723874680832
npr.org/sections/goats…
23/ Mid-summary: Upgrade to best mask quality you can find (N95 if avail., KF94, possibly KN95), but FIT is always still critical. #bettermasks
If you can't breathe easily so exhaled breath goes THROUGH material, it is too restrictive and/or a bad fit.

If you can't breathe easily so exhaled breath goes THROUGH material, it is too restrictive and/or a bad fit.
24/ One concern is counterfeit or knock-off #N95, #KN95 respirators. I don’t think anything is fool-proof, but the CDC has this resource:
cdc.gov/niosh/npptl/us…
cdc.gov/niosh/npptl/us…
25/ Another question that has come up a lot recently is how long you can wear your #N95-type mask. See tweet #1 for some ideas & sub-links.
First, if possible look at manufacturer recommendations for tips.
CDC/NIOSH officially lists e.g. 8-hr limit: cdc.gov/niosh/topics/h…
First, if possible look at manufacturer recommendations for tips.
CDC/NIOSH officially lists e.g. 8-hr limit: cdc.gov/niosh/topics/h…
26/ The next set of tweets is NOT meant to be definitive, b/c there are plenty of people who work in this space more than I do. I assembled some thoughts related to practical questions, however, and these may be helpful as you answer questions specific to your situation.
27/ Convos about practical N95 care & longevity, w/ @linseymarr @Smogdr @j_g_allen @JudahWorldChamp +
- Rotate use per day:
- Filtration likely good for months:
- Good until straps no longer pull to seal:
- Rotate use per day:
https://twitter.com/Smogdr/status/1357120830610632704
- Filtration likely good for months:
https://twitter.com/linseymarr/status/1357103925380280321
- Good until straps no longer pull to seal:
https://twitter.com/Smogdr/status/1357121649963720704

28/ A few add’l #N95 tips:
- Use longer than 8-hrs likely ok if necessary:
- But best to swap when damp from use (can reduce filtration)
- N95, HEPA filtration add electrostatic properties to boost filtration; this is reduced when damp or after washing
- Use longer than 8-hrs likely ok if necessary:
https://twitter.com/HuffmanLabDU/status/1357111817554698241
- But best to swap when damp from use (can reduce filtration)
- N95, HEPA filtration add electrostatic properties to boost filtration; this is reduced when damp or after washing

29/ For use outside of a medical environment, it is probably best not to clean N95s but rather to rotate use. I.e. place aside in a paper bag for a couple days and then return, e.g. suggestion by @smogdr:
https://twitter.com/Smogdr/status/1357120830610632704
30/ In a medical environment, may be necessary to sterilize if not enough to dispose. Several studies have focused on break-down after rounds of cleaning, e.g.:
generalsurgerynews.com/In-the-News/Ar…
pubmed.ncbi.nlm.nih.gov/33279587/
Via @linseymarr:
generalsurgerynews.com/In-the-News/Ar…
pubmed.ncbi.nlm.nih.gov/33279587/
Via @linseymarr:
https://twitter.com/linseymarr/status/1341759236989214721
31/ One question is about shelf-life of N95 (and similar) masks. That is relatively little concern. They don't physically break down easily.
This study also supported that from an experimental perspective:
aaqr.org/articles/aaqr-…
This study also supported that from an experimental perspective:
aaqr.org/articles/aaqr-…
32/ Summary: Masks still a critical piece of community armor against further COVID transmission. As variants of concern threaten, upgrade to #bettermasks & focus on fit.
For more general answers wrt #COVIDisAirborne, see FAQ by @jljcolorado & colleagues: tinyurl.com/FAQ-aerosols
For more general answers wrt #COVIDisAirborne, see FAQ by @jljcolorado & colleagues: tinyurl.com/FAQ-aerosols
33/ If you want to read still further about #bettermasks and much more, lots of articles (search "mask") compiled on both 'media' tab (i.e. news) & 'science articles' tab (research).
docs.google.com/spreadsheets/d…
docs.google.com/spreadsheets/d…
• • •
Missing some Tweet in this thread? You can try to
force a refresh






