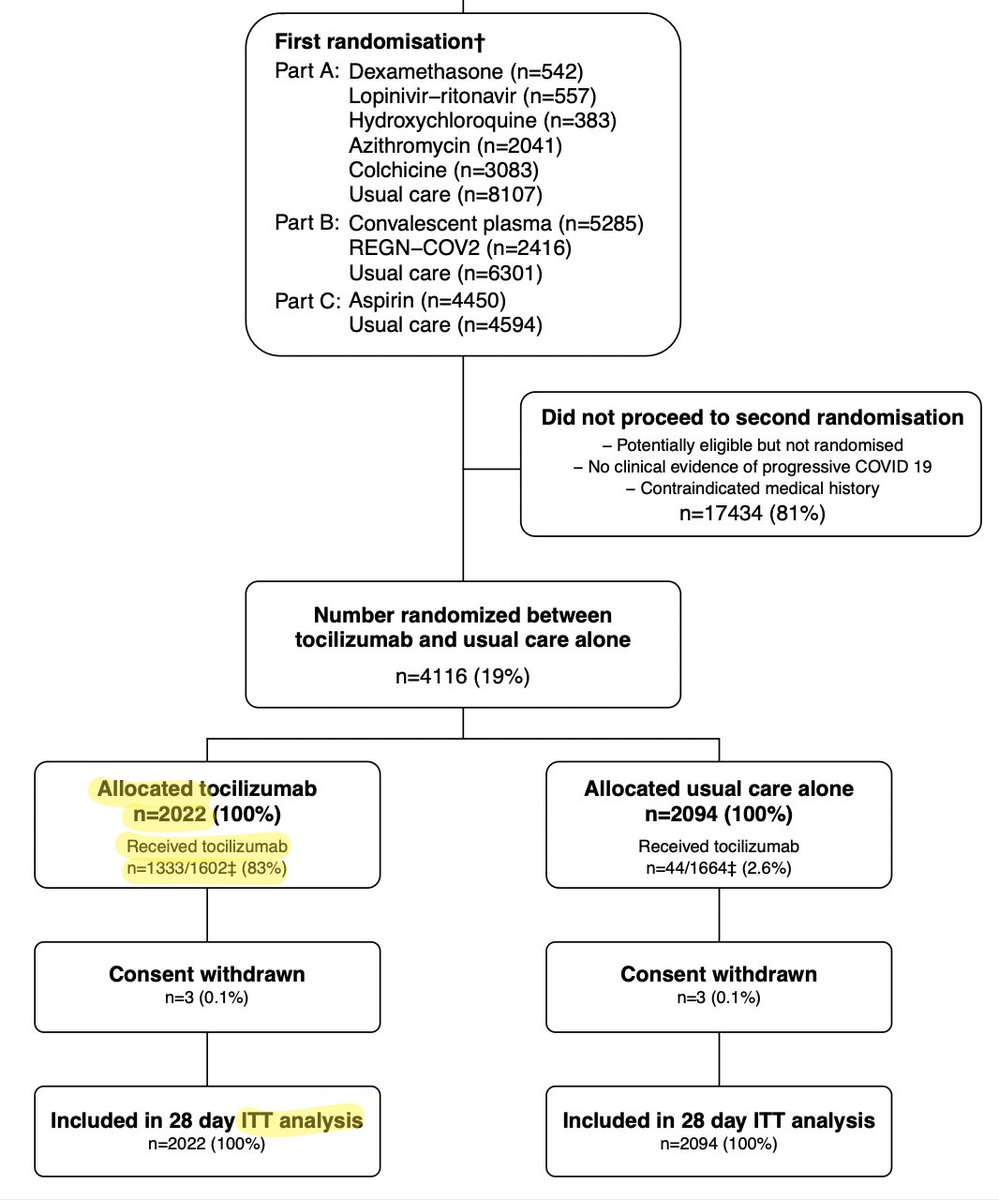
Following @remap_cap & #RECOVERY #Tocilizumab results, @NIHCOVIDTxGuide has updated guidelines:
-#Toci + #Dexamethasone now recommended for all ICU pts on IMV, NIPPV, or HFNC
-Toci + Dex recommended for non-ICU pts w/ rapidly increasing O2 needs & elevated inflammatory markers
1/

-#Toci + #Dexamethasone now recommended for all ICU pts on IMV, NIPPV, or HFNC
-Toci + Dex recommended for non-ICU pts w/ rapidly increasing O2 needs & elevated inflammatory markers
1/


You can read the updated NIH COVID19 treatment guidelines here: covid19treatmentguidelines.nih.gov/statement-on-t…
IMO, this change makes sense based on the published & pre-published data, which I discussed last month:
2/
IMO, this change makes sense based on the published & pre-published data, which I discussed last month:
2/
https://twitter.com/nickmmark/status/1359964191306567680
There are some caveats:
-Toci must be combined with dexamethasone (not given alone; ? harm signal)
-It should be given early (w/i 3 days)
-Toci should NOT be given to people who are already immunosuppressed or who have “an uncontrolled” infxn (e.g. getting worse despite Abx)
3/
-Toci must be combined with dexamethasone (not given alone; ? harm signal)
-It should be given early (w/i 3 days)
-Toci should NOT be given to people who are already immunosuppressed or who have “an uncontrolled” infxn (e.g. getting worse despite Abx)
3/

I’m less convinced about the benefits of Toci in a non-ICU population. “Rapidly increasing O2 needs” & elevated inflammatory markers (such as CRP > 75 mg/dl) are a bit more subjective inclusion criteria for a costly intervention IMO.
4/
4/
Overall, these new reccs align with my practice after RECOVERY/REMAP. I think these are very reasonable guidelines for how & when to use #Toci in treating people with severe #COVID19. I’m impressed that NIH updated so fast.
#medtwitter What do y’all think?
#medtwitter What do y’all think?
• • •
Missing some Tweet in this thread? You can try to
force a refresh