Pre-print of the @remap_cap RCT of #anticoagulation for ICU patients w/ #COVID19 adds details but confirms what we learned from the press release:
- no improvement in survival or organ failure w/ therapeutic (TA) vs prophylactic anticoagulation (PA)
- medrxiv.org/content/10.110…
1/


- no improvement in survival or organ failure w/ therapeutic (TA) vs prophylactic anticoagulation (PA)
- medrxiv.org/content/10.110…
1/


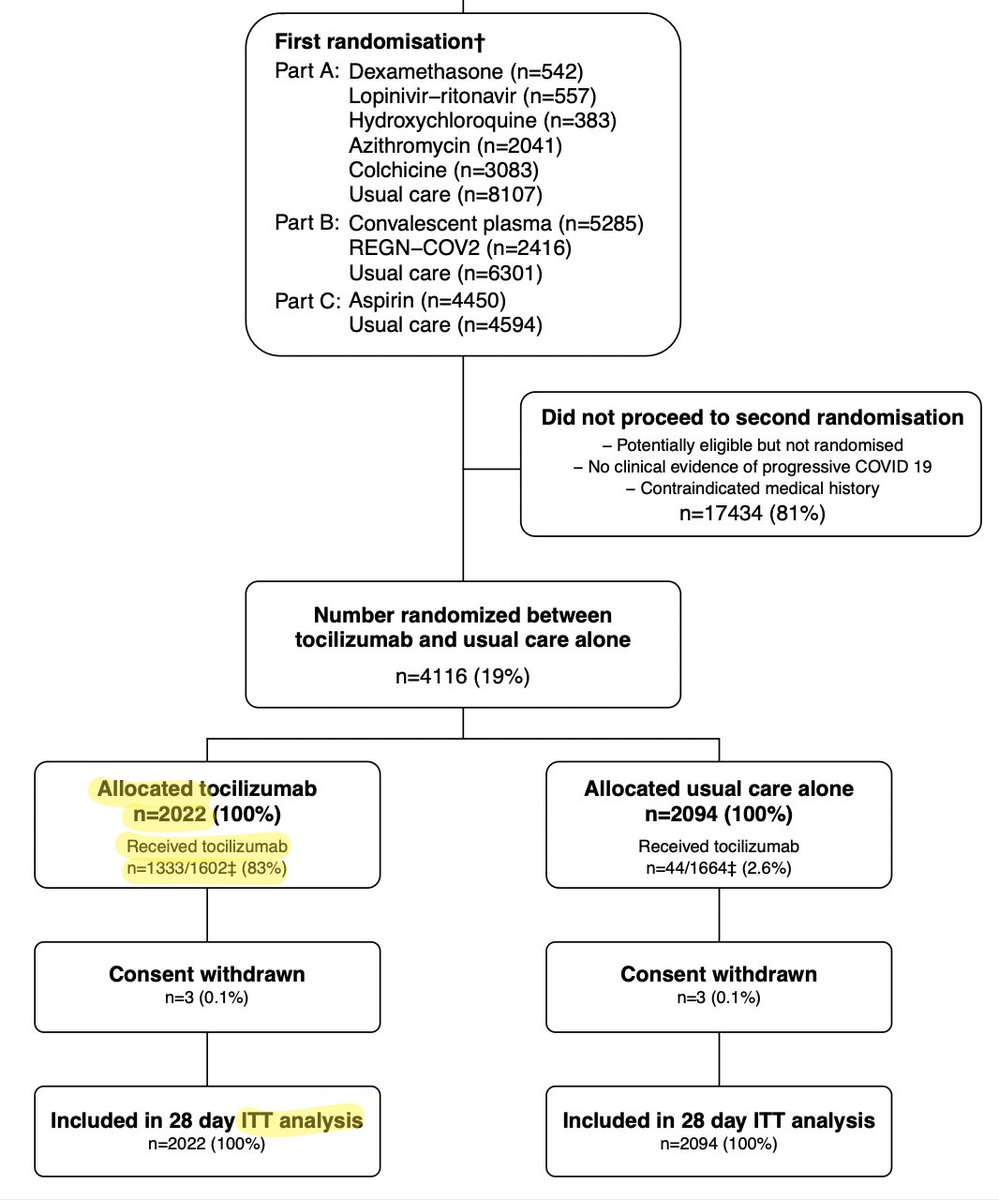
This study is the amalgam of 3 large platform RCTs of TA in COVID19: @remap_cap @ACTIV4a & ATTACC.
Each trial was administered separately but as much as possible they harmonized the design so the results could be analyzed together. (a pragmatic way to enroll more pts faster)
2/
Each trial was administered separately but as much as possible they harmonized the design so the results could be analyzed together. (a pragmatic way to enroll more pts faster)
2/

There were some differences:
-REMAP enrolled suspected & confirmed infxn; the others only enrolled confirmed
-choice of anticoagulant varied
-most importantly, the definition of prophylaxis: ~1/2 the sites used standard low-dose heparin, the remainder used “intermediate dose”
3/
-REMAP enrolled suspected & confirmed infxn; the others only enrolled confirmed
-choice of anticoagulant varied
-most importantly, the definition of prophylaxis: ~1/2 the sites used standard low-dose heparin, the remainder used “intermediate dose”
3/

The groups were randomized centrally. ACTIV-4a assigned 1:1, the other arms were adaptive so slightly more in PA.
Overall the groups were pretty similar @ baseline: mostly male, median ~60yo, fairly sick (p/f 119)
Most received corticosteroids. Oddly 35-40% were on NIPPV.
4/
Overall the groups were pretty similar @ baseline: mostly male, median ~60yo, fairly sick (p/f 119)
Most received corticosteroids. Oddly 35-40% were on NIPPV.
4/

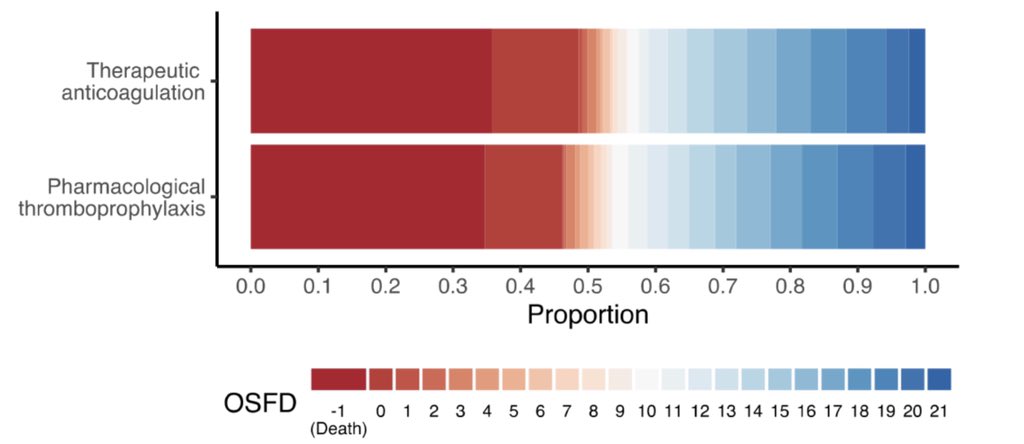
The 1° outcome was organ failure support free days (OSFDs) up to day 21. This includes days not on HFNC, NIV, IMV, or ECMO.
I’m not a big fan of lumping these together; being on HFNC is very different than being on ECMO. 🤷♂️
2° outcomes: 90-day survival, thrombosis, bleeding
5/
I’m not a big fan of lumping these together; being on HFNC is very different than being on ECMO. 🤷♂️
2° outcomes: 90-day survival, thrombosis, bleeding
5/
The results are pretty compelling:
-Therapeutic anticoag (TA) didnt increase days free of organ failure support (OSFDs); in fact there were numerically more OSFDs w prophylactic anticoag (PA)
-TA didn’t improve survival
-there was more bleeding w/ TA & more thrombosis w/ PA
6/


-Therapeutic anticoag (TA) didnt increase days free of organ failure support (OSFDs); in fact there were numerically more OSFDs w prophylactic anticoag (PA)
-TA didn’t improve survival
-there was more bleeding w/ TA & more thrombosis w/ PA
6/



Importantly both “standard dose” & “intermediate dose” prophylactic anticoagulation (PA) subgroups trended superior to therapeutic anticoagulation (TA).
Patients not on IMV appeared to do better w/ PA than TA. Big strike against the “you have to anticoagulate early” argument.
7/
Patients not on IMV appeared to do better w/ PA than TA. Big strike against the “you have to anticoagulate early” argument.
7/

They conclude that therapeutic AC is not only likely worse than prophylactic AC, but there is an 81% chance that therapeutic AC actually reduces hospital survival.
The authors (being Bayesians) point out that the small ongoing studies are unlikely to change this conclusion.
8/
The authors (being Bayesians) point out that the small ongoing studies are unlikely to change this conclusion.
8/

Last March as were inundated treating the first wave of people with COVID19, we saw a pattern of thrombosis. It was reasonable to wonder if therapeutic anticoagulation was needed for this new disease.
A year later we’ve studied the problem & we now know the answer: it isn’t.
9/
A year later we’ve studied the problem & we now know the answer: it isn’t.
9/
• • •
Missing some Tweet in this thread? You can try to
force a refresh