Why is there a shortage of Remdesivir, with family members desperately trying to procure it when it has been proven that it is no better than routine care? #EvidenceBasedMedicine
There are two living meta analysis and systematic reviews that show it is not better than routine care. Close to 4000 patients in randomized trials showing no benefit, and patients & families desperate and buying in the black market because they believe it will save their patient
Wow! This tweet seems to have stirred up a lot of interest (and violent reactions). I'm glad there has been (some) discussion about the science, and the evidence, and justifiable disagreement. We've had experienced experts in the field weighing in, and I respect those views
Some part of this discussion however, seem to have degenerated into personal attacks, and that is disappointing. We are all mature adults, and we can well agree to disagree.
First, the reality. What provoked this tweet was the hundreds of patients' families running from pharmacy to pharmacy trying to source Remdesivir. The current blackmarket price is Rs 4 to 5000 and in some places Rs 12 to 15000 (price cap at Rs 1400; actual price closer to Rs 700)
While theoretically possible, it is unlikely that all these patients fit into the criteria where the experts seem to believe there is benefit. What this does is actually quite cruel...
In the event that the patient dies after the family could not source Remdesivir, it puts the burden of guilt squarely on the family, leaving them with "If only I had tried harder (or paid more) to get it, maybe our loved one would still be alive"
This is cruel
This is cruel
Second, the evidence - the two largest trials - RECOVERY and SOLIDARITY - both failed to show a difference in outcomes between Remdesivir and routine care. Does this rule out subsets where this may be effective? No
But prescribing it indiscriminately is not exactly evidence-based
But prescribing it indiscriminately is not exactly evidence-based
I still agree with the possibility that there may be subsets where this will work. That was not the point of my tweet. I quite enjoyed the scientific arguments put forth. What was disappointing were some of the arguments...
Argument 1. Our clinical decisions cannot be dictated by RCTs alone.
I agree, but only partially. We do need to exercise clinical judgement combined with the data, but if we allow clinical judgement to overshadow data from RCTs, we are going down a very slippery slope
I agree, but only partially. We do need to exercise clinical judgement combined with the data, but if we allow clinical judgement to overshadow data from RCTs, we are going down a very slippery slope
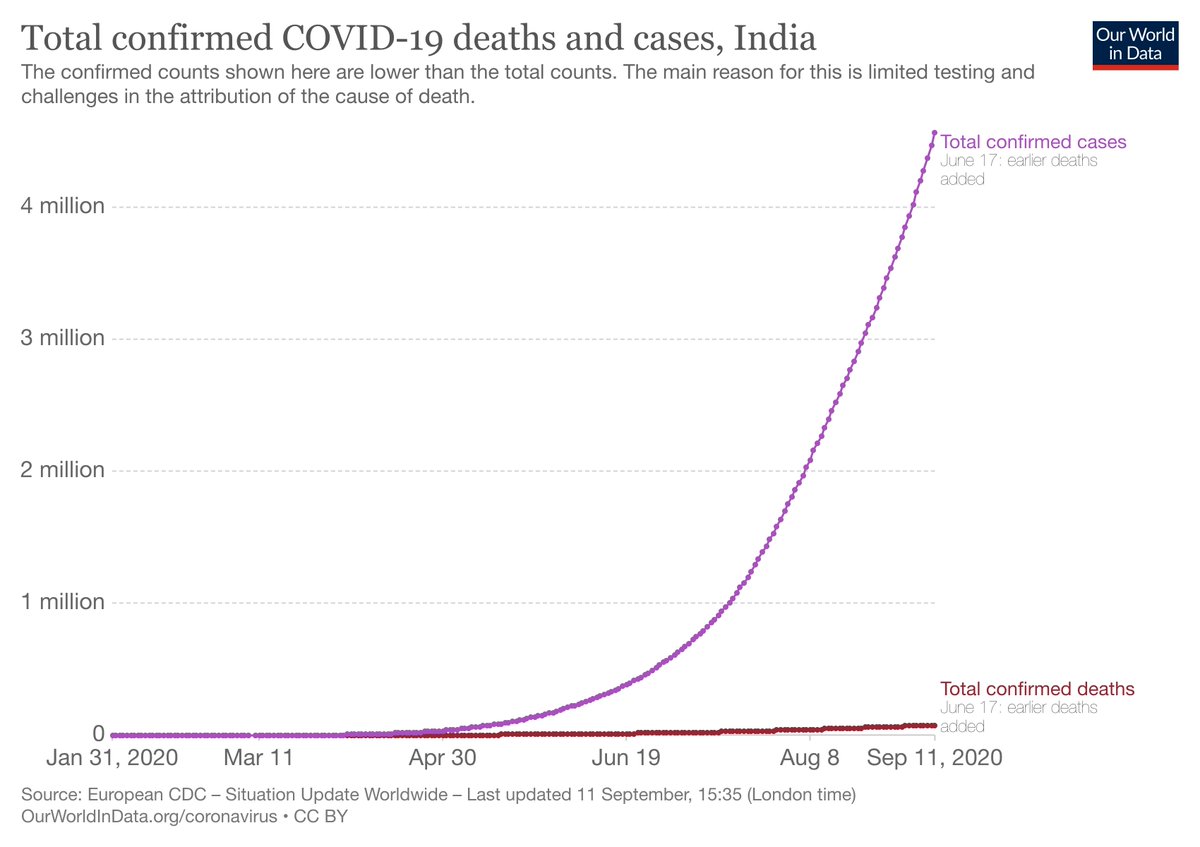
This is especially true in a disease like #COVID_19 where the vast majority of patients ultimately recover. If you were to give any drug to someone with COVID, there is a 98% chance that the patient will recover. The important point here is that it doesn't prove the drug works.
With a 98% recovery rate, crediting whatever drug you gave for the recovery is unwise, and certainly not the right decision for the next 100 patients with COVID that you treat. Which is why the reliance on RCTs and level 1 evidence.
Argument 2: "He got it wrong with #Tocilizumab in Oct 2020, so he's wrong here too."
Poor argument. There was no evidence to support Tocili in Oct 2020. There is now - I agree now that it has its role in specific indications...
Poor argument. There was no evidence to support Tocili in Oct 2020. There is now - I agree now that it has its role in specific indications...
But that doesn't change the fact that in Oct'20, we didn't have data. That's how science progresses. You get new data, and you change your mind - that is why having an open mind is so important for a researcher. Using that as an argument to question someone's credibility is weak
Argument(s) 3: a) You cannot argue with 'x' because he is so "well-known"
Though this was made to support my tweet, I disagree with this - what is important is the content, and not the person who has the opinion. I refuse to use my position to legitimize my statements
Though this was made to support my tweet, I disagree with this - what is important is the content, and not the person who has the opinion. I refuse to use my position to legitimize my statements
Argument(s) 3: b) Stay in your lane - you are an oncologist, and you can't speak about COVID treatment
Again, I disagree - if we had to be ID experts to comment on #COVID_19, the discourse over the past year would have been unidimensional and poor
Again, I disagree - if we had to be ID experts to comment on #COVID_19, the discourse over the past year would have been unidimensional and poor
And importantly, the assumptions that were made. That being an oncology centre, we didn't treat COVID. That's not true at all.
Responding to the magnitude of the pandemic, on request from the government, and being a responsible public hospital, Tata Memorial (in spite of being a dedicated cancer centre) has been treating COVID over the past year, at one point with 170 beds dedicated for COVID treatment
We have treated thousands of patients with COVID over the past year; and we did this while continuing to treat all our patients with cancer. I hope this clarifies things and we are able to accept disagreements without being disagreeable. Stay safe, folks.
• • •
Missing some Tweet in this thread? You can try to
force a refresh