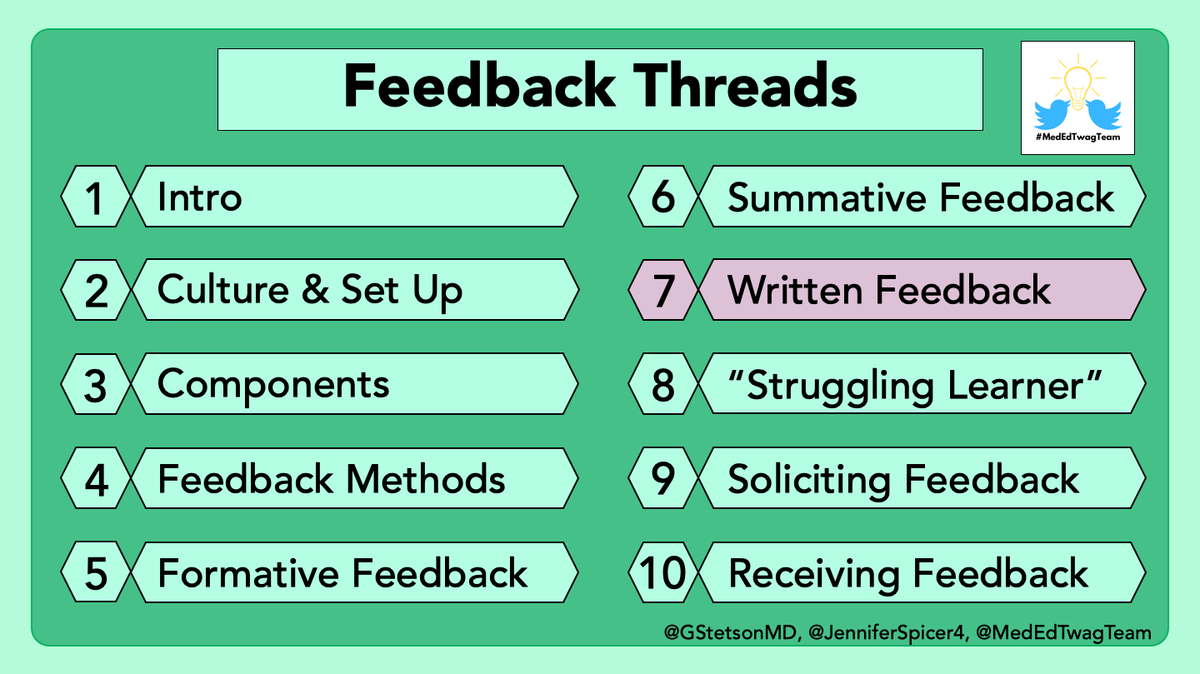
1/ It's another #TweetorialTuesday from the @MedEdTwagTeam for our #MedTwitter & #MedEd friends.
This week, I will give you a glimpse into how I structure my day on the inpatient service to balance teaching & completing my own tasks as an attending!
This week, I will give you a glimpse into how I structure my day on the inpatient service to balance teaching & completing my own tasks as an attending!

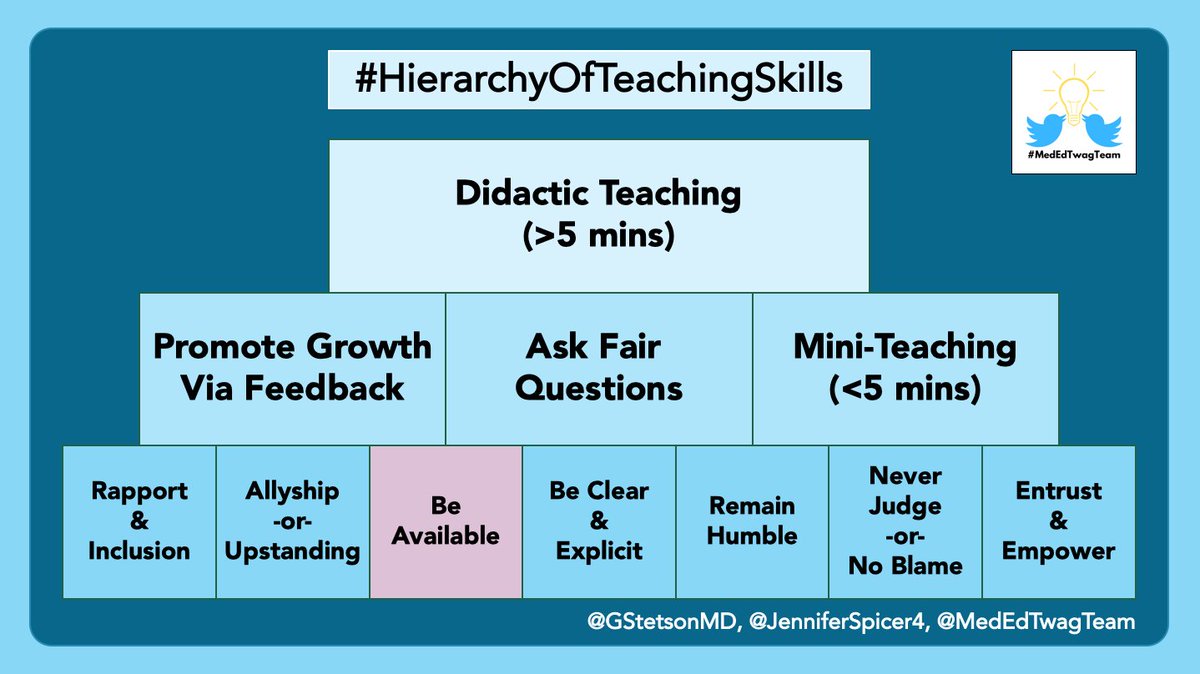
2/ As a reminder, we are discussing the foundational skills for inpatient teaching - i.e., how to "fit it in"
@GStetsonMD provided his perspective last week.
This week, I will compare/contrast how I approach this when I'm on a primary vs consulting team.
@GStetsonMD provided his perspective last week.
https://twitter.com/GStetsonMD/status/1432706288211869699
This week, I will compare/contrast how I approach this when I'm on a primary vs consulting team.

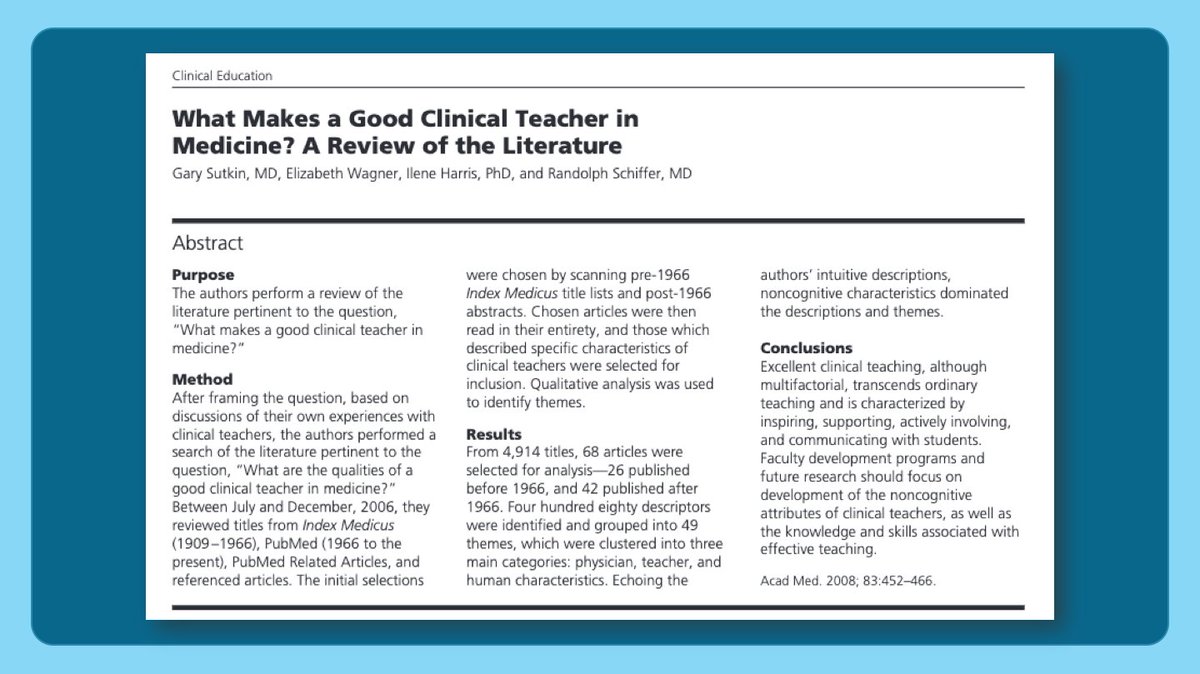
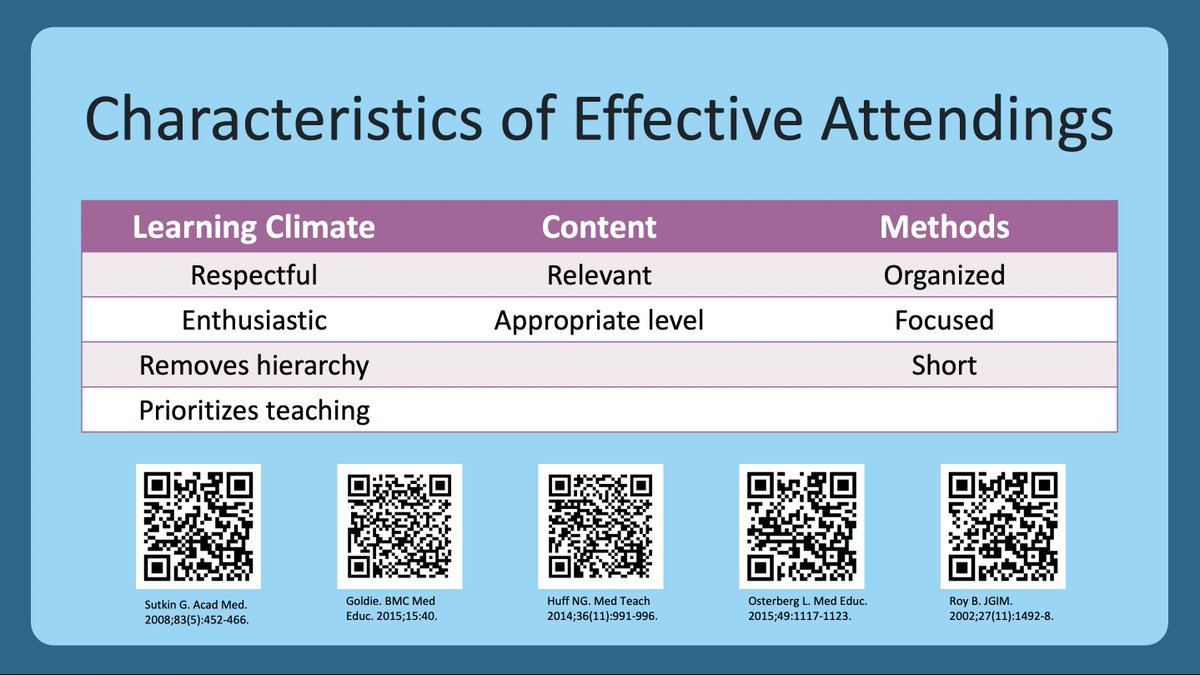
3/ I've used the literature to consider how I want to teach and conduct rounds.
Therefore, I consider:
1⃣ how my actions impact the learning climate
2⃣ what content my learners need to know for their future practice
3⃣how to incorporate focused, relevant teaching into rounds
Therefore, I consider:
1⃣ how my actions impact the learning climate
2⃣ what content my learners need to know for their future practice
3⃣how to incorporate focused, relevant teaching into rounds
4/ Last week @GStetsonMD highlighted some literature describing these 4 purposes of rounds.
When I round, I tend to prioritize developing a patient care plan & team education.
Myself & the team typically communicate with patients before/after rounds.
When I round, I tend to prioritize developing a patient care plan & team education.
Myself & the team typically communicate with patients before/after rounds.

5/ I serve as an attending on 2 different teams: an inpatient HIV wards team (where we serve as the primary team) & a general ID consult team.
Differences in learners, patient type, and patient volume on these two teams influence my teaching & daily schedule.
Differences in learners, patient type, and patient volume on these two teams influence my teaching & daily schedule.

6/ So here is the schedule for a typical day on the HIV inpatient service.
Key things to note:
1⃣ I see f/u patients early since residents may not recognize "sick" in this immunocompromised population.
2⃣ Longer teaching time in PM b/c each resident has fewer patients.
Key things to note:
1⃣ I see f/u patients early since residents may not recognize "sick" in this immunocompromised population.
2⃣ Longer teaching time in PM b/c each resident has fewer patients.

7/ Because this is a subspecialty service, residents require more help making medical decisions than on a Gen Med service. Additionally, they are on this service to learn, so it's important to have specialized didactics to help them feel competent & promote progressive autonomy.
8/ In contrast, here is my schedule on our consult service.
The day is longer & less predictable since we never know how many new consults we will get.
(shameless 🔌 to call consults early!)
Therefore, teaching happens first so rounds can be shortened if the day explodes 🤯🧨
The day is longer & less predictable since we never know how many new consults we will get.
(shameless 🔌 to call consults early!)
Therefore, teaching happens first so rounds can be shortened if the day explodes 🤯🧨
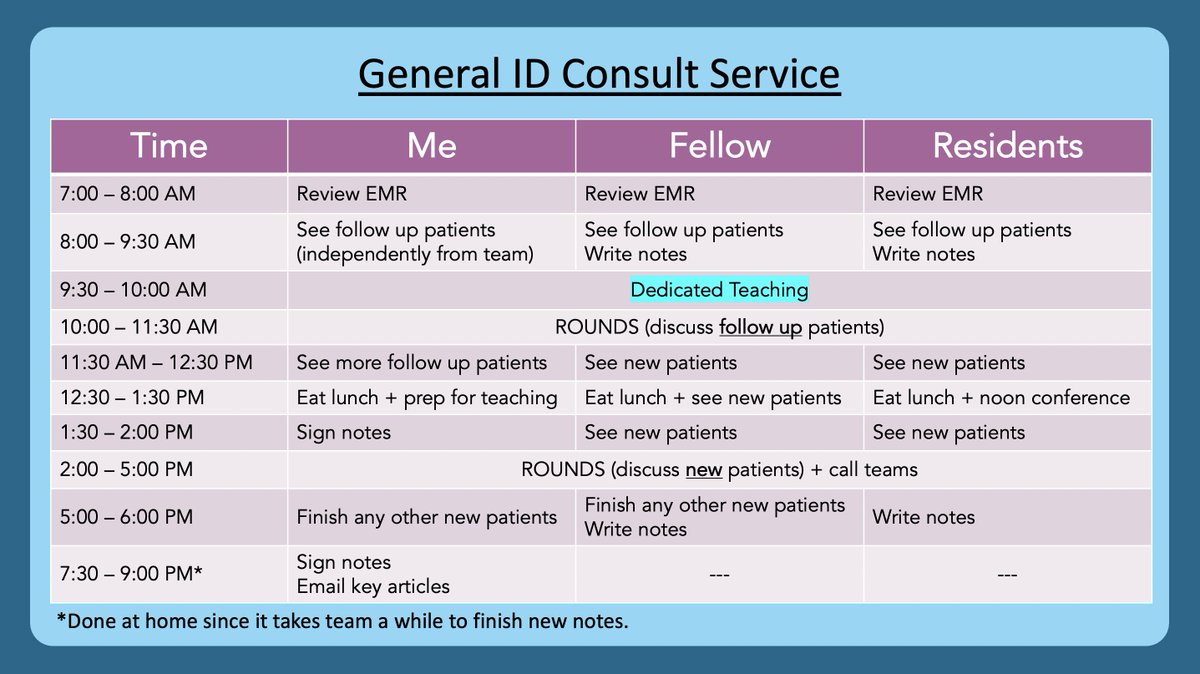
9/ I see many f/u patients before rounds b/c:
1⃣I finish my day at a reasonable time (I like to arrive early, leave early)
2⃣Rounds are spent discussing plans > presenting data.
I tell learners WHY I do this & encourage short presentations to make room for teaching on rounds.
1⃣I finish my day at a reasonable time (I like to arrive early, leave early)
2⃣Rounds are spent discussing plans > presenting data.
I tell learners WHY I do this & encourage short presentations to make room for teaching on rounds.

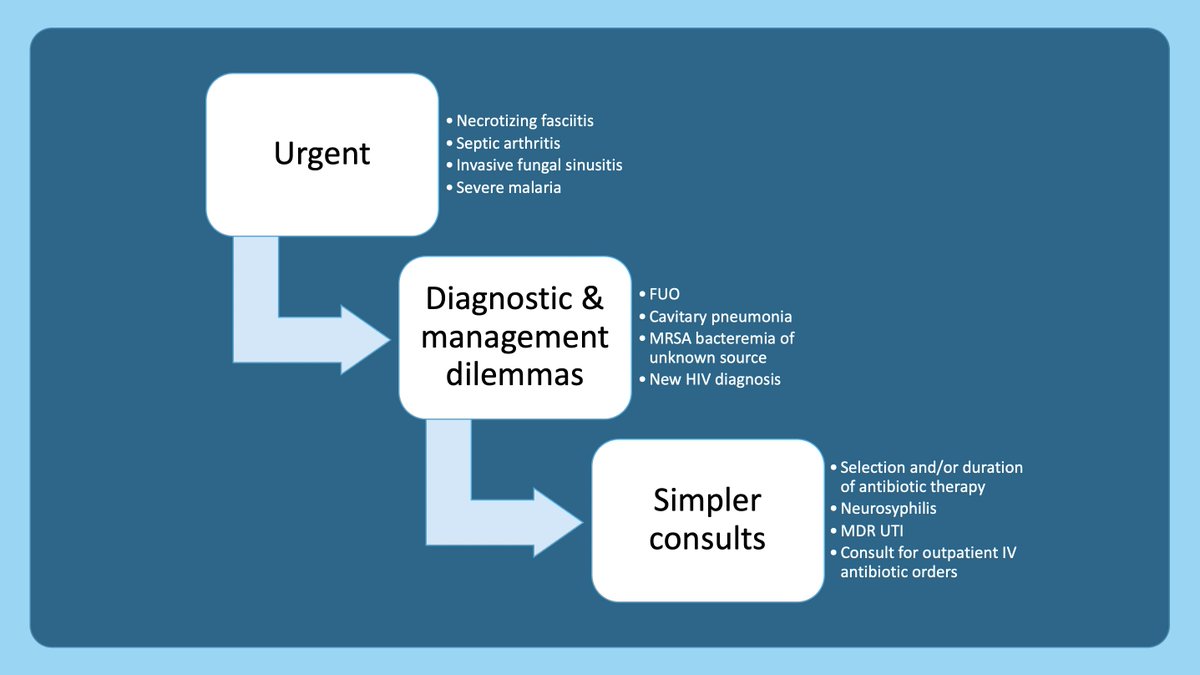
10/ When discussing patients, I ask the fellow to prioritize our discussion based on:
1. Urgent consults➡️cases that require emergent intervention
2. Diagnostic/management dilemmas➡️cases that require in-depth thinking
3. Simpler cases➡️cases with routine decision-making
1. Urgent consults➡️cases that require emergent intervention
2. Diagnostic/management dilemmas➡️cases that require in-depth thinking
3. Simpler cases➡️cases with routine decision-making
11/ For new patients, I encourage trainees to keep their presentations focused with pertinent positives/negatives to allow time for teaching.
But, I have to admit, ID docs like the story b/c it often gives us the diagnosis. Right, @DGlaucomflecken? 🤣
But, I have to admit, ID docs like the story b/c it often gives us the diagnosis. Right, @DGlaucomflecken? 🤣
https://twitter.com/DGlaucomflecken/status/1424552154002452481
12/ And to keep things moving on rounds, I continue discussing patients & teaching the residents/students while the fellow answers pages.
I am explicit about this with the fellow on Day 1 so they feel comfortable doing their work. I update them if they miss something important.
I am explicit about this with the fellow on Day 1 so they feel comfortable doing their work. I update them if they miss something important.
13/ And if rounds last too long, I discuss/see patients with just the fellow.
However, I typically like for the entire team to see any new patients that we will be following for an extended period of time so that they can put a face with the name for our discussions on rounds.
However, I typically like for the entire team to see any new patients that we will be following for an extended period of time so that they can put a face with the name for our discussions on rounds.
14/ Here’s an overview of how I fit teaching into my days (highlighted).
As for my administrative work, it's hard to get much done outside of patient care while on the consult service, so I avoid scheduling ANYTHING (even routine meetings), if possible.
As for my administrative work, it's hard to get much done outside of patient care while on the consult service, so I avoid scheduling ANYTHING (even routine meetings), if possible.

15/ How do others handle their schedule on consult services? And what do trainees prefer? Please share!
Next week, stay tuned for @YihanYangMD who will provide her perspective on this same topic.
In the meantime, follow @MedEdTwagTeam to ensure you don't miss anything!
Next week, stay tuned for @YihanYangMD who will provide her perspective on this same topic.
In the meantime, follow @MedEdTwagTeam to ensure you don't miss anything!

• • •
Missing some Tweet in this thread? You can try to
force a refresh