At the NIH Fatigue conference right now! Follow for more information.
We're at the first break, now, and there are some general comments/questions.
Excellent: ✨
~Cognitive fatigue
~Physical fatigue
~Cognitive impairment
~And then there is cognitive and physical fatigability!
~And self-report...
These are different & require different instruments.
Excellent: ✨
~Cognitive fatigue
~Physical fatigue
~Cognitive impairment
~And then there is cognitive and physical fatigability!
~And self-report...
These are different & require different instruments.
I fully agree with the above, and it is absolutely huge that people conflate these, or don't understand what instruments are actually measuring. Betsy Keller is talking about replacing w/biomedical testing like CPET, and talking about measuring cog impairment at the same time...
Which we were just talking about.
Keller is talking about doing 2-Day CPET in cancer patients and how some people post-treatment for cancer who go on to meet ME/CFS criteria.
"Is fatigue really so different in these disease states? To me, it's the final common pathway..."
Keller is talking about doing 2-Day CPET in cancer patients and how some people post-treatment for cancer who go on to meet ME/CFS criteria.
"Is fatigue really so different in these disease states? To me, it's the final common pathway..."
Christine Miaskowski:
"I really appreciate the idea of an objective measure, but reminder that these don't always correlate to subjective measures." She's participating in a project that looks @ the transition from acute to chronic pain. They are creating a "biosignature... (1/5)
"I really appreciate the idea of an objective measure, but reminder that these don't always correlate to subjective measures." She's participating in a project that looks @ the transition from acute to chronic pain. They are creating a "biosignature... (1/5)
"...that looks at not just objective but also subjective measures in combination. Could we get a similar 'biosignature' for fatigue?... it might offer some guidance...." (2/5)
Whittemore on, now, discussing RECOVER initiative for #LongCOVID. These kinds of objective measures re: what happens in the transition from acute to chronic illness in fatigue will be very important. The pain field has a lot to offer in this transition..." (3/5)
Josh Fessel from @nih_nhlbi says biosignature idea is "really exciting, really intriguing" -- and a "very realistic thing to think about". "Objective tests are important but if you're my patient and you tell me you're fatigued I can't run a test and say "no you're not"..." (4/5)
Fessel continues: "from biospecimens, from clinical measures, from EHR, from subjective report... I think the future for that line of inquiry could be really exciting." (5/5)
Question:
Some people show cooling helps with physical fatigue in exercise. Does lowering the temperature help cognitive fatigue (or fatigability)? (1/2)
Some people show cooling helps with physical fatigue in exercise. Does lowering the temperature help cognitive fatigue (or fatigability)? (1/2)
Craig Heller:
If indeed a final common pathway is energy metabolism, if temperature affects energy metabolism in a large, dynamic muscle, it is also likely to influence processes in the brain." (2/2)
If indeed a final common pathway is energy metabolism, if temperature affects energy metabolism in a large, dynamic muscle, it is also likely to influence processes in the brain." (2/2)
From me: I don't see why vasoconstriction from cooling wouldn't help cognitive function; that only makes sense. Especially in ppl with potentially comorbid POTS or hEDS.
Keller adds that #pwME have cold hands/feet/legs post-exertionally. The blood goes to the core to keep things functioning. "To me, a lot of what we see with this population is a huge blood flow issue". Decrease in word-finding, time-to-response, is clearly a blood flow issue.
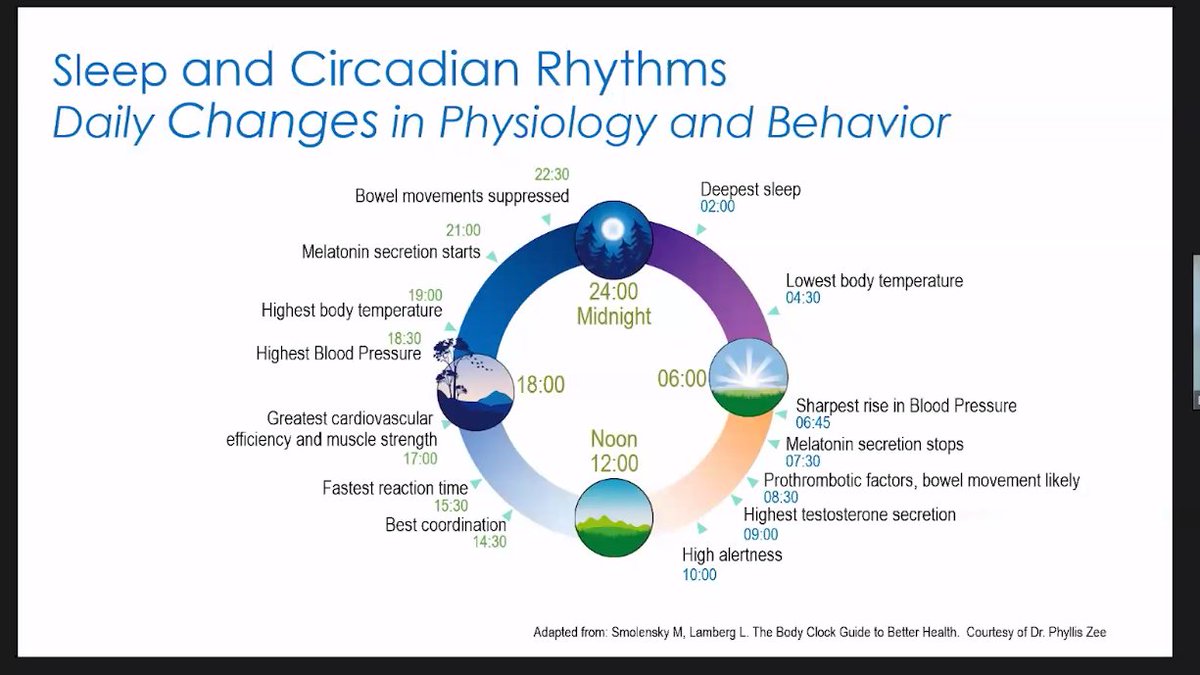
Phyllis Zee who, AFAIK, does not study #pwME mentions a huge gradient re: the proximal vs distal temperature -- something that has been noted in ME. me-pedia.org/wiki/Body_temp…
Was waiting for someone to mention Younger, and Komaroff just did. Brain temp is significantly higher at rest. me-pedia.org/wiki/Evidence_…
Kuppuswamy was asked about ME/CFS but stated that she had "mostly focused on neurological diseases". Whoops.
Now panelists are talking about the eyes and their responses in fatigue. It's been interesting to watch rising intrigue in this field. Spoken with Dr. Nina Muirhead on this a few times. Zee says that pupillary response & attention is "another biomarker to consider".
15 min break!
15 min break!
Not sure how the threading got messed up, but look starting here for Q&A at the break. Often the Q&A is the most interesting part, so you don't want to miss it!
https://twitter.com/exceedhergrasp1/status/1442534836116148230
Fourth talk: very interesting!
https://twitter.com/exceedhergrasp1/status/1442555842209849349
Sorry, y'all -- I need a break :(
I'm sitting in Andy Miller's talk rather than doing a play-by-play, but I will say this: don't ignore depression research. Depression is often the result of neuroinflammation and could be pertinent to other neuro diseases. I for one will be looking up his other work. 

This series of tweets is a self-demonstrating article. Back of my neck is burning, head is tingling; went from upright & super-interested to prone. Sensory sensitivity has kicked up; about to put in my audio-normalizing earbuds. Light seems brighter. Hanson up next!
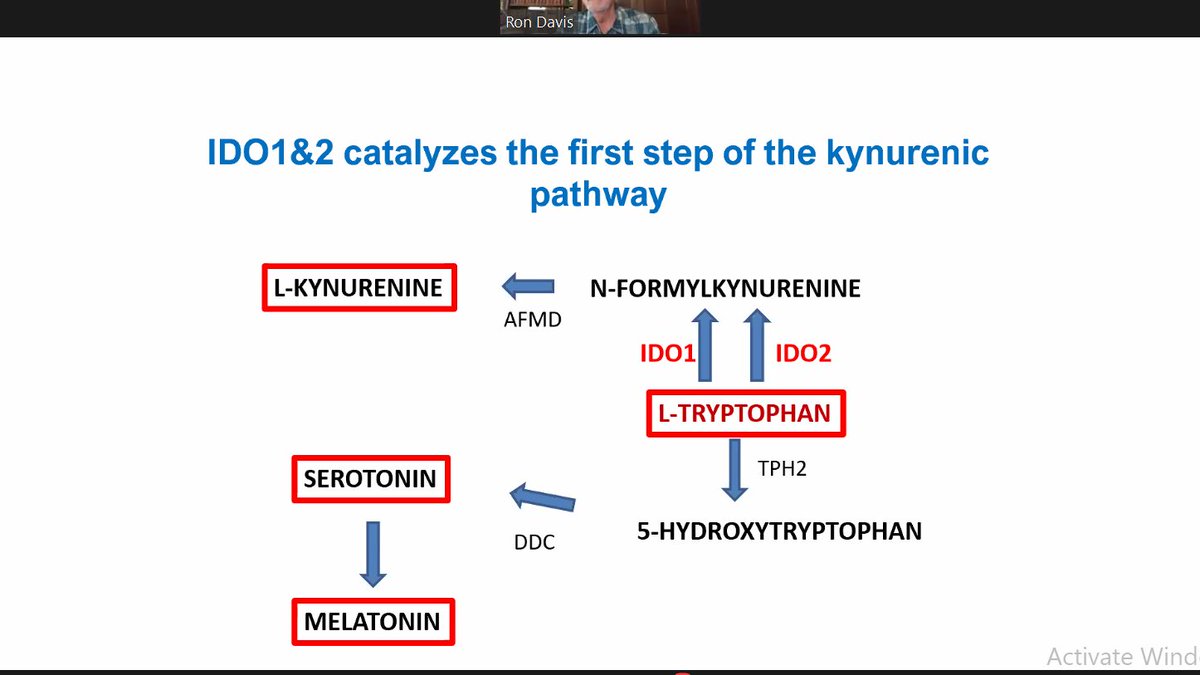
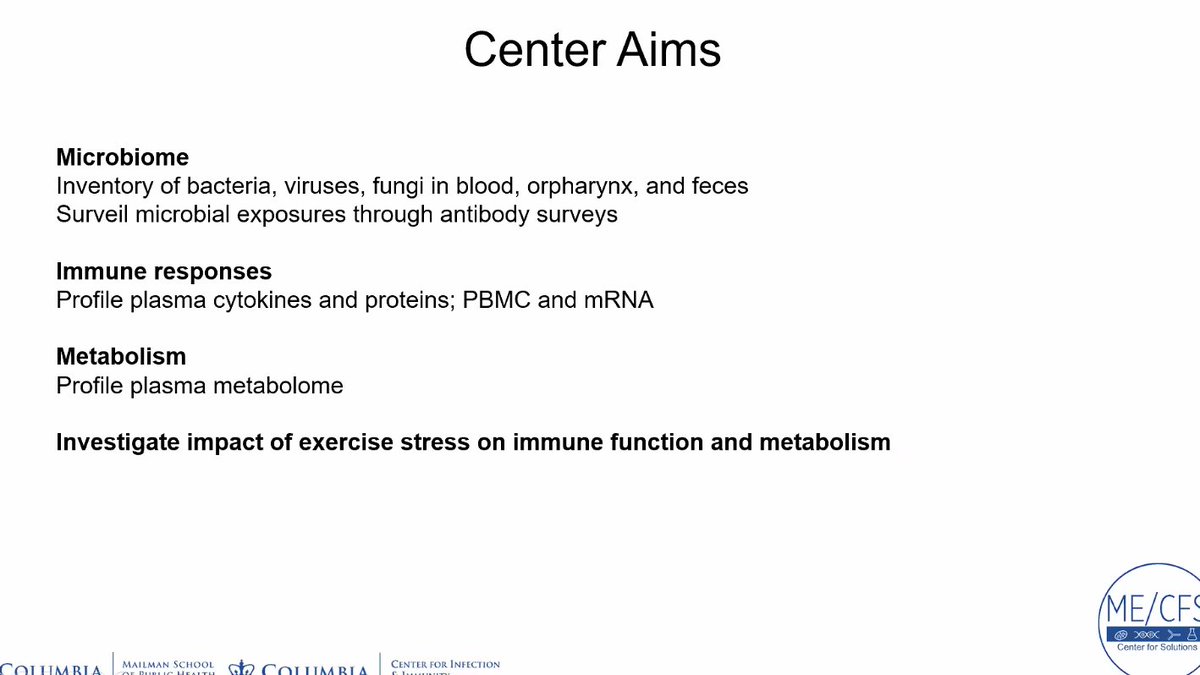
Sleep deprivation & its effects on the gut (ROS) #fatigue #microbiome #ROS
https://twitter.com/exceedhergrasp1/status/1442597046062510086
Ragulja says, too, that you can overdo it with antioxidants: it "really depends on the context".
I STRONGLY agree with Klerman's conclusion that you must collect samples at similar times and collect data re: sleep, based on your hypothesis/what you hope to find. "We keep having different results in circadian-dependent stuff in ME/CFS!"
On to general convo:
General agreement that you can't just block one cytokine & expect it to help: "the systems are too complex"
Miller: IFN-a for depression... patients became insomniacs. MSLTs during the day meant they didn't sleep & were MASSIVELY fatigued.
General agreement that you can't just block one cytokine & expect it to help: "the systems are too complex"
Miller: IFN-a for depression... patients became insomniacs. MSLTs during the day meant they didn't sleep & were MASSIVELY fatigued.
TNF antagonists seemed to help with this, Miller goes on.
Nath: The brain has really its own milieu...
Miller: Most of these drugs don't cross the BBB. A couple of the JAK inhibitors seem to maybe affect fatigue...
Nath: The brain has really its own milieu...
Miller: Most of these drugs don't cross the BBB. A couple of the JAK inhibitors seem to maybe affect fatigue...
M. Davis: It's only in my imagination, but there could be some autoreactive T- or B-cell activity that is messing w/some neurological system or energy metabolism system... perhaps we could use this to ID the antigen, find some targets (for drugs)
M. Davis: People get infections their whole life but then later in life, they get #MECFS or #MS... so what is different, now? Maybe multiple hits over time accumulates specific cells that have 'escaped' from normal regulation.
Klimas: I think we have this unique opportunity with #LongCOVID to better understand the sequence of events that's driving ppl into chronic illness
M. Davis: Epitope shedding & autoimmunity might be pertient...
[Me: Googles... nature.com/articles/nri72….]
M. Davis: Epitope shedding & autoimmunity might be pertient...
[Me: Googles... nature.com/articles/nri72….]
Klimas: Is metabolic change pathological or adaptive?
[ME: ADAPTIVE!!!!]
M. Davis: I was impressed by the description of how fever would interrupt energy metabolism... An anecdote: if a beehive is infected, adult bees beat their wings faster to raise the temp of the hive...
[ME: ADAPTIVE!!!!]
M. Davis: I was impressed by the description of how fever would interrupt energy metabolism... An anecdote: if a beehive is infected, adult bees beat their wings faster to raise the temp of the hive...
Klimas: How do you put this together and as a clinician come up with an intervention to start helping ppl heal? Where would you start?
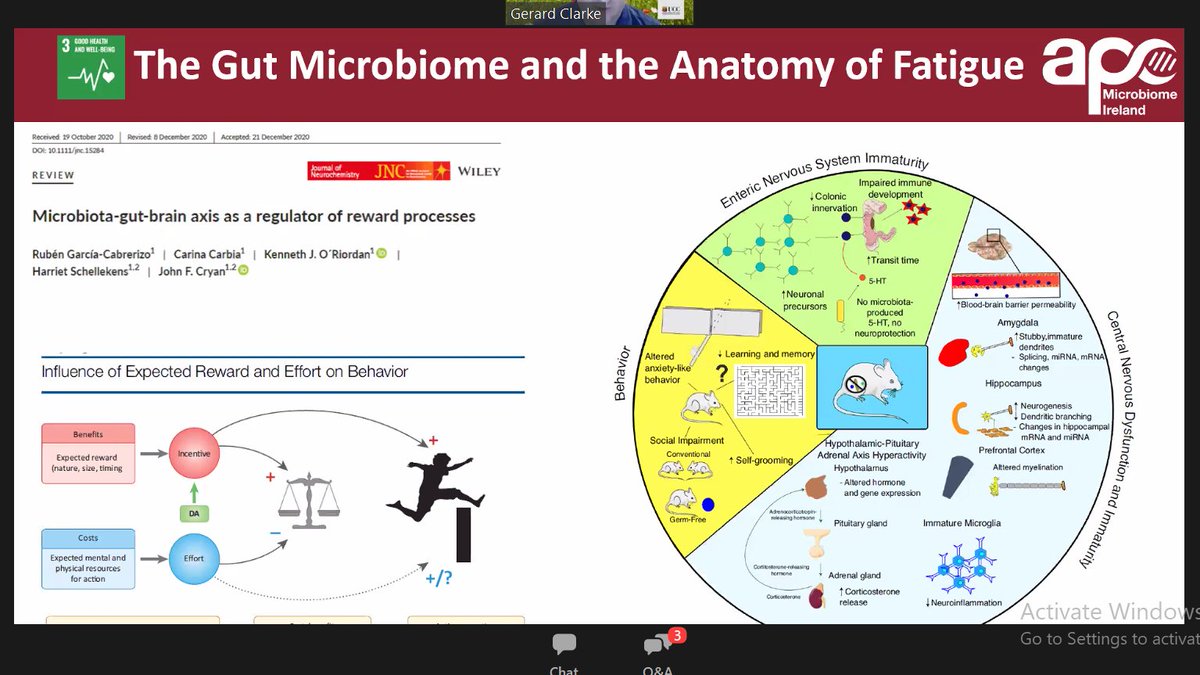
[ME: THE GUT!!!!]
Klimas: Do you start w/sleep?
Miller: One of the things that has struck me today is the differences... (1/5) #fatigue #MECFS
[ME: THE GUT!!!!]
Klimas: Do you start w/sleep?
Miller: One of the things that has struck me today is the differences... (1/5) #fatigue #MECFS
Miller, cnt'd
...in terms of the immunology & some of the stuff that goes on in CNS in MECFS & other fatigue states like in cancer or depression, where there is a much tighter relationship with inflammation than there is in #CFS... (2/5) #fatigue #MECFS
...in terms of the immunology & some of the stuff that goes on in CNS in MECFS & other fatigue states like in cancer or depression, where there is a much tighter relationship with inflammation than there is in #CFS... (2/5) #fatigue #MECFS
Miller, cnt'd:
Is there some sense that these are really different animals & we're glomming er... clumping them together. Is anyone else struggling w/this as well? We think there is this switch to glycolysis & we're going to block glycolysis... (3/5) #fatigue #MECFS
Is there some sense that these are really different animals & we're glomming er... clumping them together. Is anyone else struggling w/this as well? We think there is this switch to glycolysis & we're going to block glycolysis... (3/5) #fatigue #MECFS
Miller, cnt'd:
People are looking to 'turn the cells down'. In ME/CFS, I don't think I'd go down that path! When you want to talk about fatigue generically, you have to look at the 'different fatigues' out there. (4/5) #fatigue #MECFS
People are looking to 'turn the cells down'. In ME/CFS, I don't think I'd go down that path! When you want to talk about fatigue generically, you have to look at the 'different fatigues' out there. (4/5) #fatigue #MECFS
Klimas: Lumping and splitting is an endless debate in our field... And we're at the end of our time. Join us tomorrow, etc. (5/5) #fatigue #MECFS
Day 2 Thread here:
https://twitter.com/exceedhergrasp1/status/1442882013770371074
Hey, all: if you value this work, please consider donating to #MEAction at meaction.net/donate
• • •
Missing some Tweet in this thread? You can try to
force a refresh