An 85-YO in rural Mississippi: months of tender, erythematous plaques & edema on bilateral hands extending to the elbows & on feet extending below the knees with significant pain
🔬skin granulomatous inflammation & numerous AFB
Mycobacterial🧫:➖
1/19
#IDtwitter #dermatology

🔬skin granulomatous inflammation & numerous AFB
Mycobacterial🧫:➖
1/19
#IDtwitter #dermatology


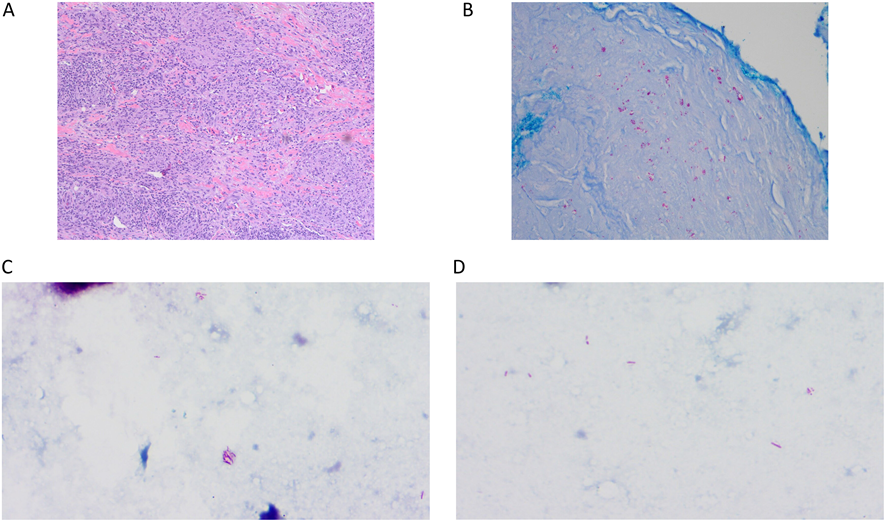
A repeat skin extensive granulomatous inflammation (A), with Ziehl-Neelsen stain clusters of acid-fast bacilli throughout the dermis (B).
Kinyoun stain >9 AFB/high-power field (C & D).
2/19
DOI: doi.org/10.1128/jcm.00…
#dermpath #microbiology
Kinyoun stain >9 AFB/high-power field (C & D).
2/19
DOI: doi.org/10.1128/jcm.00…
#dermpath #microbiology
Molecular identification: 100% identity to multiple Mycobacterium leprae
BORDERLINE LEPROMATOUS LEPROSY WITH REVERSAL REACTION
3/19
#MedTwitter #MolBiol
BORDERLINE LEPROMATOUS LEPROSY WITH REVERSAL REACTION
3/19
#MedTwitter #MolBiol
Prednisone & methotrexate for treatment of reversal reaction, & 10 days later, rifampin, minocycline, & moxifloxacin were added for treatment of leprosy
3 months into therapy: a significant improvement, & he gradually returned to his baseline functional status
4/19
#Doctor
3 months into therapy: a significant improvement, & he gradually returned to his baseline functional status
4/19
#Doctor

New cases of Leprosy, or Hansen’s disease, caused by Mycobacterium leprae or Mycobacterium lepromatosis in 2020:
✔️127,558 globally, with the highest numbers of cases reported in India, Brazil, and Indonesia
✔️159 in the US
5/19
#MedStudentTwitter #resident
✔️127,558 globally, with the highest numbers of cases reported in India, Brazil, and Indonesia
✔️159 in the US
5/19
#MedStudentTwitter #resident
M. leprae:
✔️a acid-fast, intracellular pathogen that most frequently invades Schwann cells in peripheral nerves & macrophages in the skin
✔️M. leprae DNA was detected from skeletal remains from over 4,000 years ago (the first bacterium found to cause disease in humans)
6/19
✔️a acid-fast, intracellular pathogen that most frequently invades Schwann cells in peripheral nerves & macrophages in the skin
✔️M. leprae DNA was detected from skeletal remains from over 4,000 years ago (the first bacterium found to cause disease in humans)
6/19
Nine-banded armadillos (Dasypus novemcinctus) serve as a zoonotic reservoir for human infection and are considered responsible for some transmission of indigenous cases of leprosy in the United States
7/19
#medicine #MedicalStudents
7/19
#medicine #MedicalStudents
A classification system divides leprosy, based on a spectrum of cell-mediated responses to the disease, into 5 subtypes:
✔️tuberculoid,
✔️borderline tuberculoid,
✔️mid-borderline,
✔️borderline lepromatous, &
✔️lepromatous
8/19
#MedEd #MIR
✔️tuberculoid,
✔️borderline tuberculoid,
✔️mid-borderline,
✔️borderline lepromatous, &
✔️lepromatous
8/19
#MedEd #MIR
A simpler WHO classification system exists that divides leprosy, based on number of lesions, into
✔️paucibacillary (5 lesions or less) and
✔️multibacillary (more than 5 lesions) leprosy and can be helpful for determining treatment duration
9/19
DOI: doi.org/10.1128/jcm.00…
✔️paucibacillary (5 lesions or less) and
✔️multibacillary (more than 5 lesions) leprosy and can be helpful for determining treatment duration
9/19
DOI: doi.org/10.1128/jcm.00…
🔬of tuberculoid infections: well-formed granulomas with epithelioid cells, nerve infiltration, & few bacilli
🔬On lepromatous: disorganized granulomas & foamy macrophages with many bacilli, which appear as circular aggregates of bacilli on AFB stains.
10/19
#EducaciónMédica
🔬On lepromatous: disorganized granulomas & foamy macrophages with many bacilli, which appear as circular aggregates of bacilli on AFB stains.
10/19
#EducaciónMédica
The borderline forms may have features of both tuberculoid and lepromatous leprosy.
Histopathology in the patient’s case showed poorly defined, granulomatous inflammation with evidence of high bacillary load, suggestive of disease on the lepromatous side of the spectrum.
11/19
Histopathology in the patient’s case showed poorly defined, granulomatous inflammation with evidence of high bacillary load, suggestive of disease on the lepromatous side of the spectrum.
11/19
Immunologic reactions in leprosy can occur during treatment or spontaneously during the disease course and are associated with increased morbidity.
There are two types of immune reactions.
12/19
#Medicina
There are two types of immune reactions.
12/19
#Medicina
The type 1 reaction, or reversal reaction, is a delayed-type hypersensitivity reaction associated with increased erythema of lesions, edema of the hands & feet, neuritis, and nerve impairment, & most often occurs in borderline forms of leprosy.
13/19
#AtencionPrimaria
13/19
#AtencionPrimaria
The type 2 reaction, or erythema nodosum leprosum, is an immune complex-mediated reaction causing systemic symptoms, including fevers with eruption of multiple, painful subcutaneous nodules, & tends to occur in borderline or lepromatous leprosy.
14/19
#healthcare
14/19
#healthcare
Arthritis secondary to immunologic reactions is symmetrical, affecting small joints of the hands and feet, leading to misdiagnosis as various rheumatologic disorders.
15/19
#internalmedicine
15/19
#internalmedicine
The patient’s overall clinical presentation, including increased pain and edema in his extremities, was felt to be consistent with immunologic reaction-associated arthritis and neuritis.
16/19
#primarycare
16/19
#primarycare
Management was aimed at controlling the inflammatory component of the disease using immunomodulation first followed by antimycobacterial therapy. (Fig, noted 3 months into treatment).
17/19
#dermtwitter
17/19
#dermtwitter

A diagnosis of leprosy should be suspected in a patient presenting with rash and biopsy findings positive for AFB with no growth on culture.
Molecular testing using a multilocus approach to mycobacteria can be used to confirm diagnosis.
18/19
#dermatología
Molecular testing using a multilocus approach to mycobacteria can be used to confirm diagnosis.
18/19
#dermatología
Symptoms of worsening pain, edema, paralysis, and neuropathy in the extremities should additionally prompt concern for possible immunologic reaction to guide initiation of immunosuppressive regimen.
19/19
19/19
• • •
Missing some Tweet in this thread? You can try to
force a refresh












