1) Welcome to a 🆕#accredited #tweetorial from @cardiomet_CE! Earn 0.5hr 🆓 CE/#CME by following this 🧵. Our expert faculty is Sanjiv J Shah MD @HFpEF, Cardiologist & Director, Northwestern HFpEF Program (hfpef.org). Director of Research, @NMCardioVasc
#FOAMed
#FOAMed

1b) .@HFpEF will be sharing the algorithm he uses to treat #HFpEF based on evidence we have thus far and his anecdotal experience treating patients over the past 16 years in the @NMCardioVasc HFpEF Clinic.
#CardioTwitter #MedEd @MedTweetorials #HeartFailure
#CardioTwitter #MedEd @MedTweetorials #HeartFailure
2) CE/#CMEcredit for #physicians #physicianassociates #nurses #nursepractitioners #pharmacists 🇺🇸🇨🇦🇬🇧🇪🇺.
Statement of accreditation and faculty disclosures at cardiometabolic-ce.com/disclosures/.
FOLLOW US for accredited programs in #cardiometabolic space delivered wholly on Twitter!
Statement of accreditation and faculty disclosures at cardiometabolic-ce.com/disclosures/.
FOLLOW US for accredited programs in #cardiometabolic space delivered wholly on Twitter!
3) This treatment algorithm was recently published in @JACCJournals with my friends and co-authors Barry Borlaug, @KSharmaMD, and @JenHoCardiology (who provided great feedback!). See pubmed.ncbi.nlm.nih.gov/37137592/. 

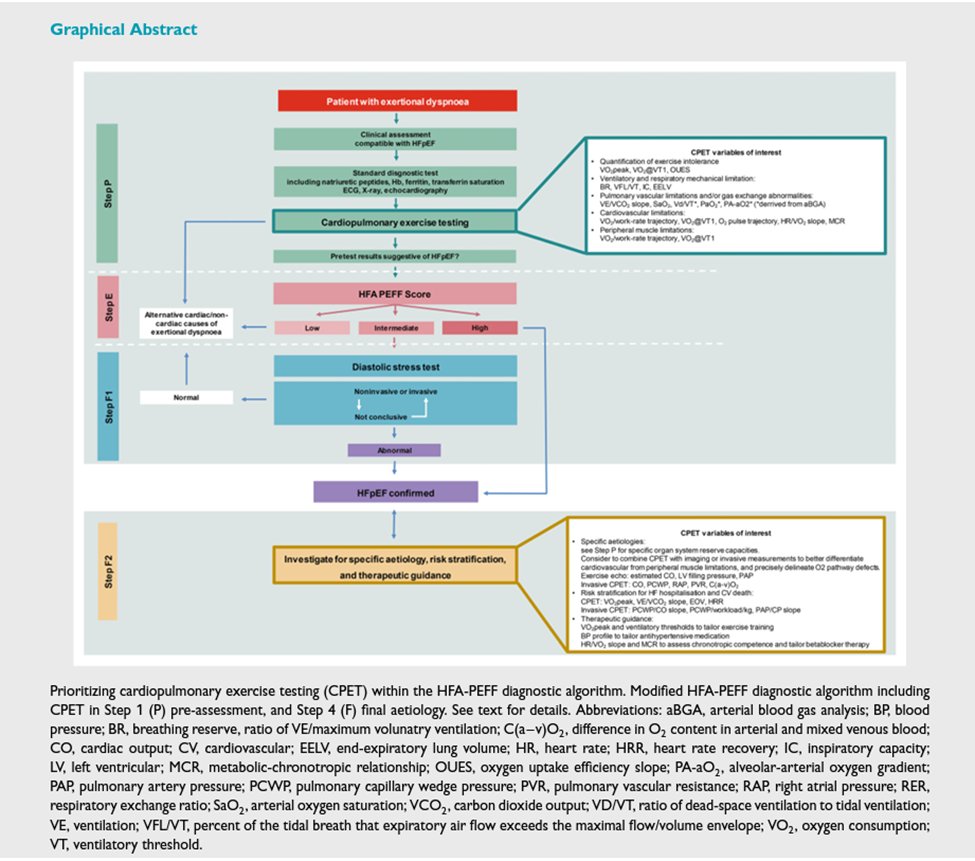
4) Step 1: Start by confirming the #HFpEF diagnosis. In equivocal cases, remember to use provocative testing, preferably exercise testing!
See 🔓ncbi.nlm.nih.gov/pmc/articles/P…
See 🔓ncbi.nlm.nih.gov/pmc/articles/P…
5) Step 2: Once the diagnosis of #HFpEF is made based on elevated LV filling pressures at rest or with exercise in the setting of an #LVEF ≥50%, first evaluate for masqueraders… 

7) Step 3: Start with an #SGLT2i in all pts but use with caution in pts with exercise-induced LA hypertension (#EILAH) because they have normal filling pressures at rest. See our recent paper on EILAH in @JACCJournals: pubmed.ncbi.nlm.nih.gov/36939661/
8) Step 4: Assess: is volume overload present? If so, start #diuretics, with preferential up-front use of an #MRA(e.g., #spironolactone, #finerenone) and loop diuretics as needed (but minimize loop diuretic dose once euvolemic)
10) Step 6: Start #ARNI (sacubitril/valsartan) if not yet started for high #BP if the patient is (1) still symptomatic, (2) #LVEF <55-60% or frequent #HF hospitalizations or +residual congestion, & (3) systolic BP >110 mmHg. Then up-titrate as tolerated.
11) Step 7: Ask 6 key questions in all patients:
(1) Is the pt on an #SGLT2i? If not, why not?
(2) Is the pt on an #MRA? If not, why not?
(3) Is the pt on an #ARNI? If not, why not?
(4) Is the patient on K+? If yes, replace with (or up-titrate) MRA if possible
(1) Is the pt on an #SGLT2i? If not, why not?
(2) Is the pt on an #MRA? If not, why not?
(3) Is the pt on an #ARNI? If not, why not?
(4) Is the patient on K+? If yes, replace with (or up-titrate) MRA if possible
12) Step 7 (continued):
(5) Is the patient on a #nitrate or pulmonary vasodilator? Discontinue if possible
(6) Is the patient on a #betablocker? Wean off unless using for #AFib, #angina, or #MI, or other non-#HFpEF indication
(5) Is the patient on a #nitrate or pulmonary vasodilator? Discontinue if possible
(6) Is the patient on a #betablocker? Wean off unless using for #AFib, #angina, or #MI, or other non-#HFpEF indication
13) Step 8a: Implement #HF education in all patients (daily weights, BP, and HR; establish “dry weight” for volume overloaded pts to guide #diuretic dosing [esp loop diuretics])
14) Step 8b: Educate pts on an exercise training regimen that combines aerobic training + resistance training (maintaining muscle mass and reducing risk for worsening frailty is critical!). Phase 3 #cardiac_rehab or Rx #pulmonary_rehab in pts with concomitant pulmonary disease
15) Step 9: For persistent symptoms and/or #HF hospitalizations ➡️ HF clinic referral, reevaluate for #HFpEF masqueraders, check for worsening comorbidities, if persistent fluid overload Rx HCTZ, use implantable PA monitoring, and evaluate for chronotropic incompetence
17) Additional tip #1: In patients with persistent fluid overload on #SGLT2i, #MRA, and loop #diuretic, avoid #metolazone! Low-dose #HCTZ typically works because of the benefit of sequential nephron blockade...
18) ...The distal convoluted tubule is amped up if already on SGLT2i, MRA, & loop diuretic, so just a little bit of HCTZ (e.g., 12.5 mg qd) can result in significant diuresis. What if #eGFR is very low? No problem, if still making urine, HCTZ will still usually work in #HF pts.
19) Additional tip #2: Which exercise training regimen do you prescribe? I try to mimic what’s been done in trials of exercise in HFpEF patients…
🔓 ahajournals.org/doi/10.1161/CI…
🔓 ahajournals.org/doi/10.1161/CI…
20) Additional tip #3: Pathophys often changes in HFpEF pts as they have events (eg, hospitalization; changes in lifestyle, diet, environment; new meds started for other conditions; new-onset comorbidities or cardiac conditions). Don’t get complacent when caring for #HFpEF pts!
21) Additional tip #4: When caring for #HFpEF pts, we often become the coordinator of care ➡️ need to treat the WHOLE patient in order to make them feel better. Provide a #multidisciplinary Rx plan.
22) Additional tip #5: Avoid #polypharmacy, use combo meds when possible (many are generic), and watch out for adverse effects of non-cardiac medications that may exacerbate #HFpEF.
23) Finally… there are many patients with HFpEF that need our help. Please consider starting a dedicated HFpEF program at your institution if you don’t have one already. This paper explains how to do it 😊… link.springer.com/article/10.100…
24) Caveats (the fine print): #SGLT2i should be considered in all patients except those with type 1 diabetes #T1D, orthostatic hypotension, #eGFR <20-25, or very frequent yeast infections (or history of severe GU infections).
25) Caveats (cont’d): Yeast infections are readily treatable, usually not a reason to permanently stop #SGLT2i. Instruct pts to hold SGLT2i therapy for a few days on “sick days” (GI illness, dehydration, active infections). High #HgbA1c is not a contraindication to SGLT2i.
26) Caveats (cont’d): #MRA should be considered in all pts except those with K+ >5.0 or #eGFR <30. Replace K+ supplementation with MRA whenever possible. Re-check K+ and renal function 1 week and 1 month after initiation, and q3-6 months thereafter.
27) Caveats (cont’d): #ARNI most effective if EF <55-60% or frequent HF hosp (congested phenotype); avoid in pts with history of #angioedema, low BP, orthostatic hypotension, restrictive #cardiomyopathy, #PAH, constrictive pericarditis, cardiac #amyloidosis
28) Caveats (cont’d): #AFib patients often have low stroke volume and inability to augment stroke volume during exertion due to LA dysfunction. Avoid excessive rate control in these patients.
29a) So, let's review a couple "take-home" points. All BUT which of the following should be considered "foundational" therapy for #HFpEF?
a. #SGLT2i
b. #MRA
c. #anticoagulant
d. loop #diuretics (until euvolemic)
a. #SGLT2i
b. #MRA
c. #anticoagulant
d. loop #diuretics (until euvolemic)
29b) It's c, #anticogaulant, which isn't indicated in #HFpEF unless the pt has concomitant #AFib. And for "foundational" therapy, consider #ARNI for high #BP (see tweet 10 ⤴️).
30a) Which of the following drugs is best avoided in patients with #HFpEF?
a. #betablockers
b. #metolazone
c. #nitrates
d. all of the above
a. #betablockers
b. #metolazone
c. #nitrates
d. all of the above
30b) It's all of the above. Leave off #BBs unless needed for #AFib, #angina, or #MI; use #HCTZ instead of #metolazone; avoid #nitrates or pulmonary vasodilators if possible.
31) And just like that—you’ve earned 0.5hr 🆓 CE/#CME! Claim your credit NOW at cardiometabolic-ce.com/cardiorenal44. And then FOLLOW US for more #MedEd by expert authors, delivered wholly on Twitter. .@HFpEF & @cardiomet_CE thank you for joining us!
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter
















