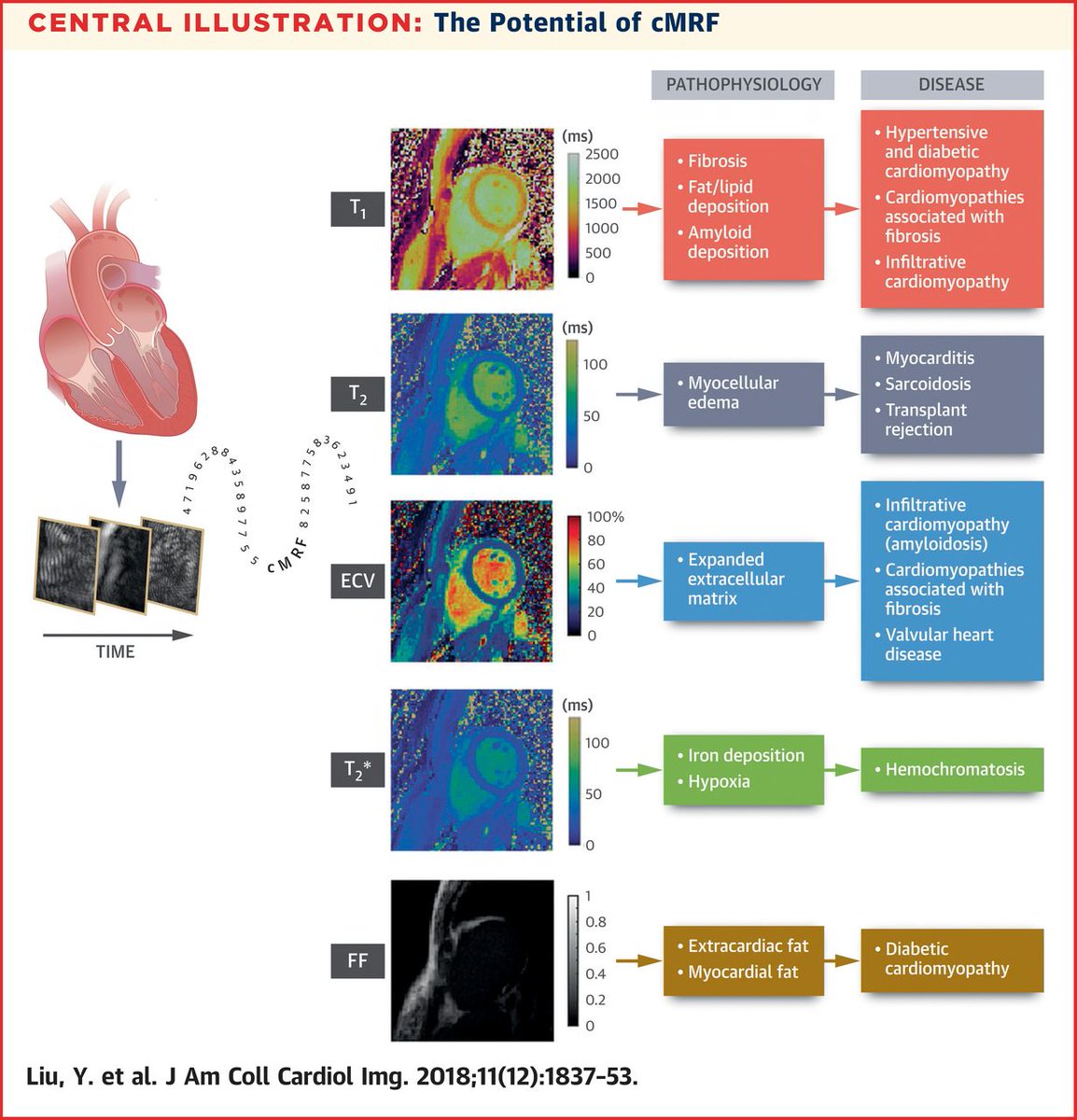
✔️Cardiac MRI for HF evaluation VERY useful
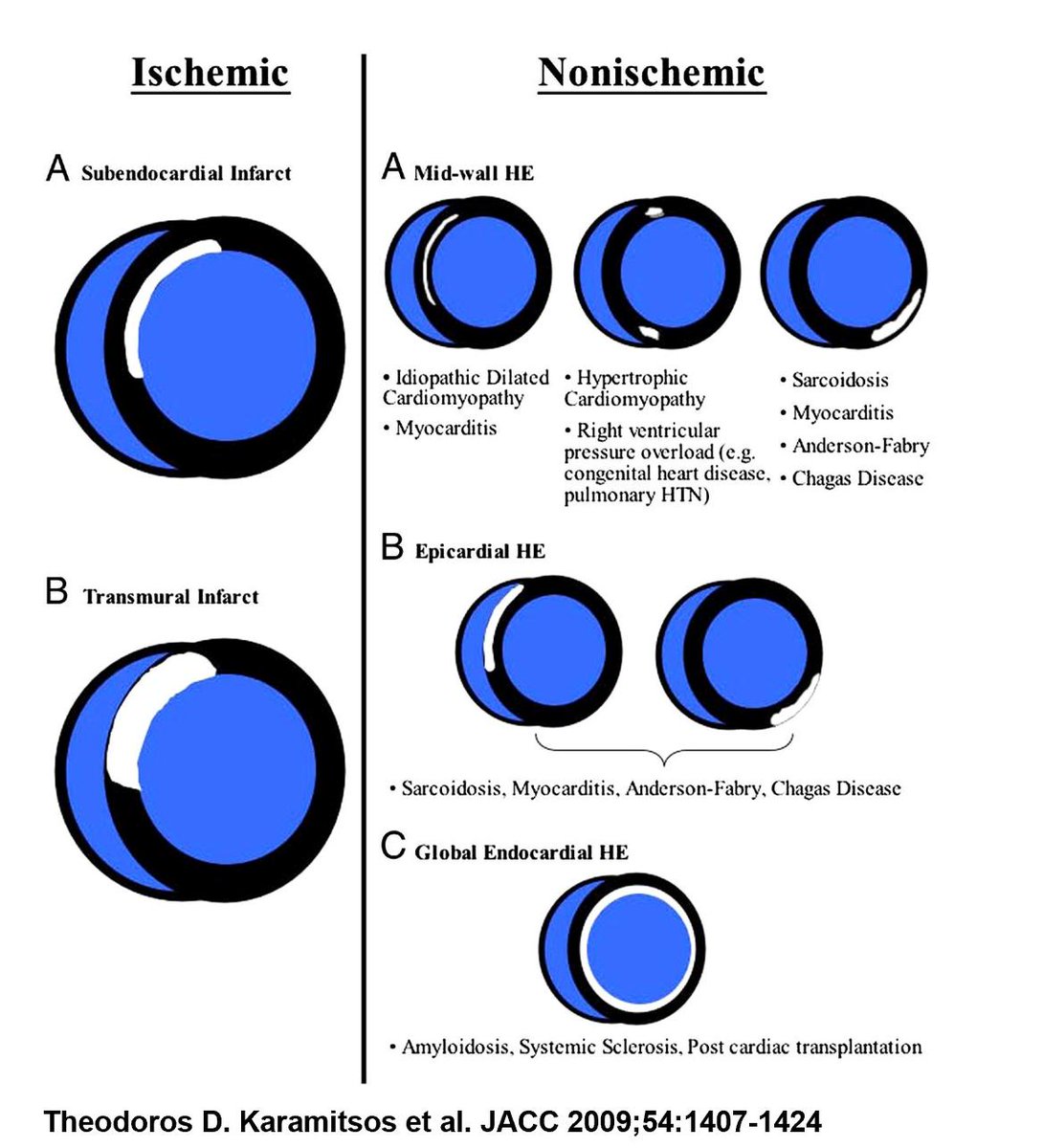
✔️LGE patterns suggestive for specific diagnoses
✔️T2 images find the "water" --> identify active inflammation/edema (acute injury, myocarditis)
Primary MR:
✔️Still a surgical disease...when the risk level is not prohibitive and appropriate center/surgeon outcomes.
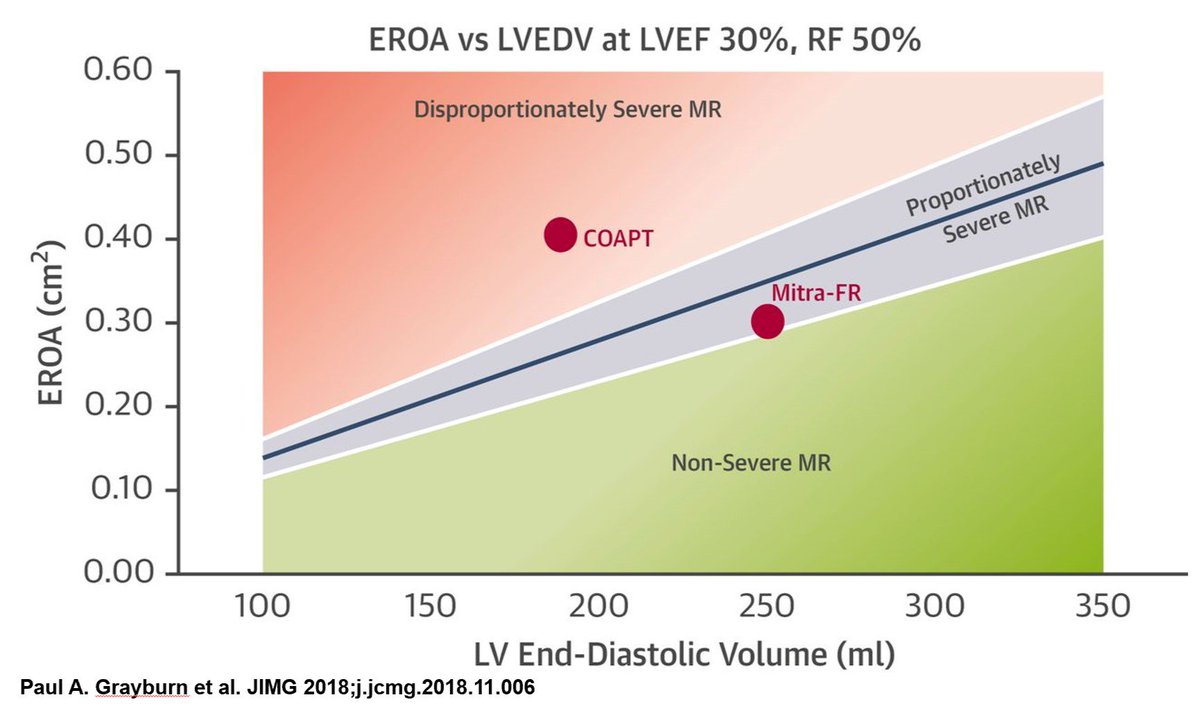
Secondary MR:
✔️MitraClip story is evolving. Image below gives a new way to look at patient selection.
Consider DOACs in APPROPRIATELY selected patients with:
✔️Need for extended VTE treatment
✔️CAD/PAD (though increased bleeding and not common practice)
*Not all DOACs are equal, so please refer to the individual studies
The question(some artistic license): Patient with stable CAD (>12mo from a stent, on ASA only). Develops new AF (C2V of 3). Low bleeding risk. What regimen would you recommend?
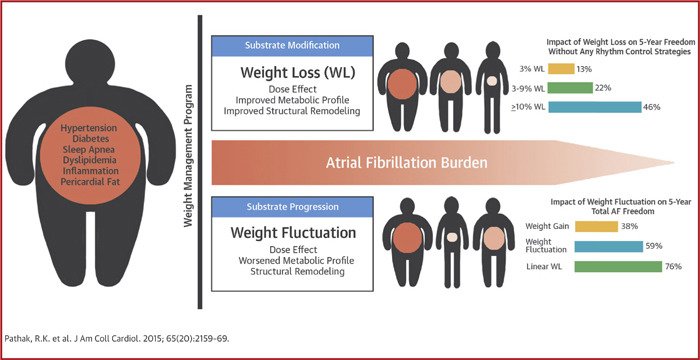
Atrial fibrillation + obesity:
✔️Weight loss is key
✔️Ideally >10% + sustained loss
✔️Detect and treat OSA
Ischemic stroke tips for the cardiologist:
✔️Permissive hypertension
✔️Immediate ASA
✔️Defer AF anticoag for days ➡️ risk of hemorrhage >> recurrent stroke
✔️Stroke during an PCI? ➡️ STAT CT head + check ACT for bleeding risk
DOAC safety points:
✔️Don't bridge with heparin ➡️ just stop and restart if needed
✔️HASBLED score made for warfarin ➡️ not completely applicable for DOACs
✔️Apixaban used in ESRD and obesity ➡️ levels less predictable ➡️ watch for AEs
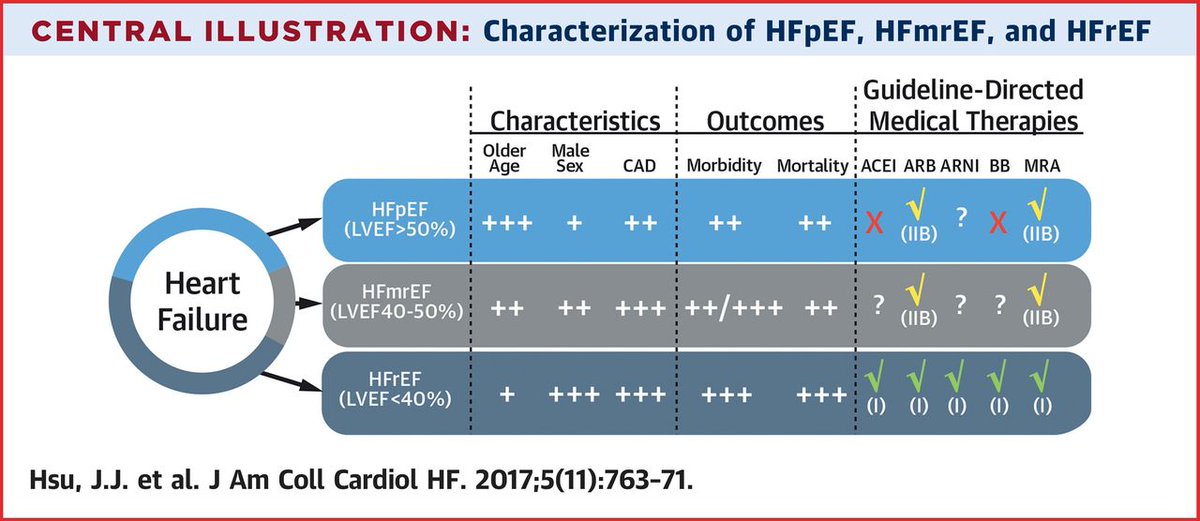
HFmrEF: mid range EF (40-49%)
✔️Not quite HFrEF or HFpEF - we need to better understand
✔️Ex) post MI
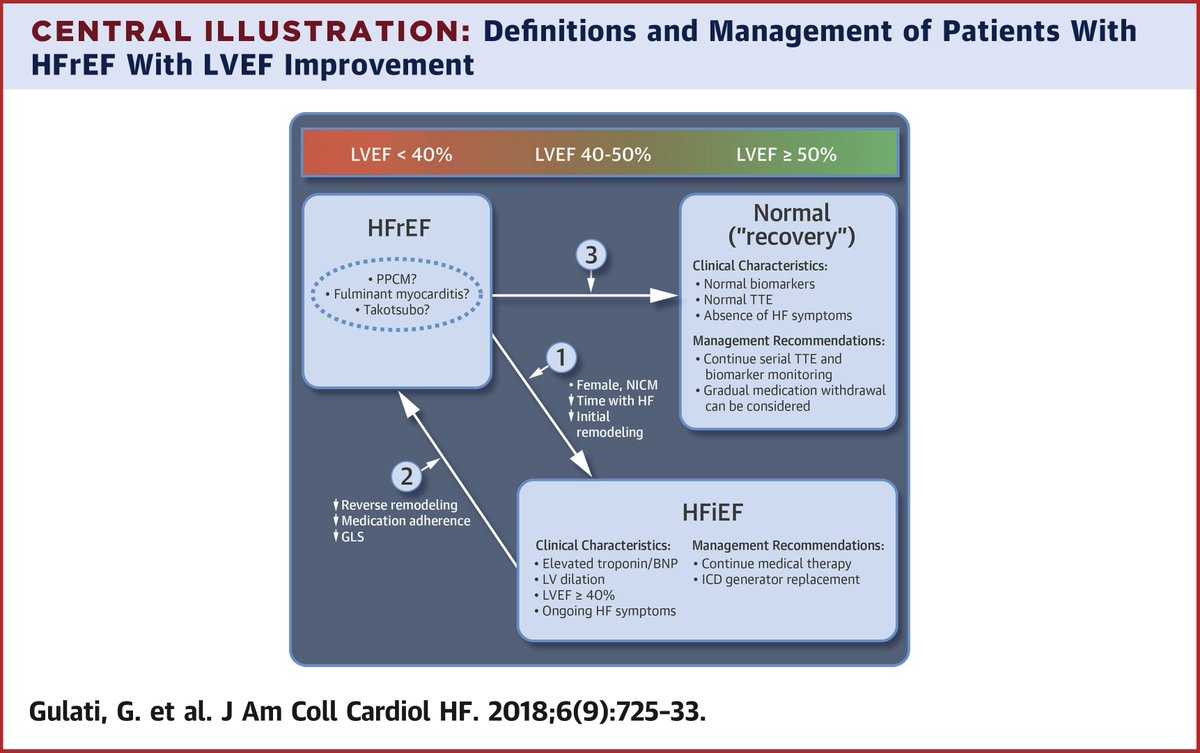
HFiEF
✔️HFrEF with improved EF (>40%)
✔️Do not stop GDMT ➡️ high likelihood to relapse
✔️LV strain and genetic profiles predict outcomes
Cardiac amyloidosis:
✔️Under-diagnosed ➡️ consider in HFpEF and LF/LG AS
✔️Tafamidis for mutant/wild-type TTR ➡️ reduces mortality + improves function/QOL
Cardiac sarcoidosis:
✔️Steroid/immune therapy commonly used but evidence lacking
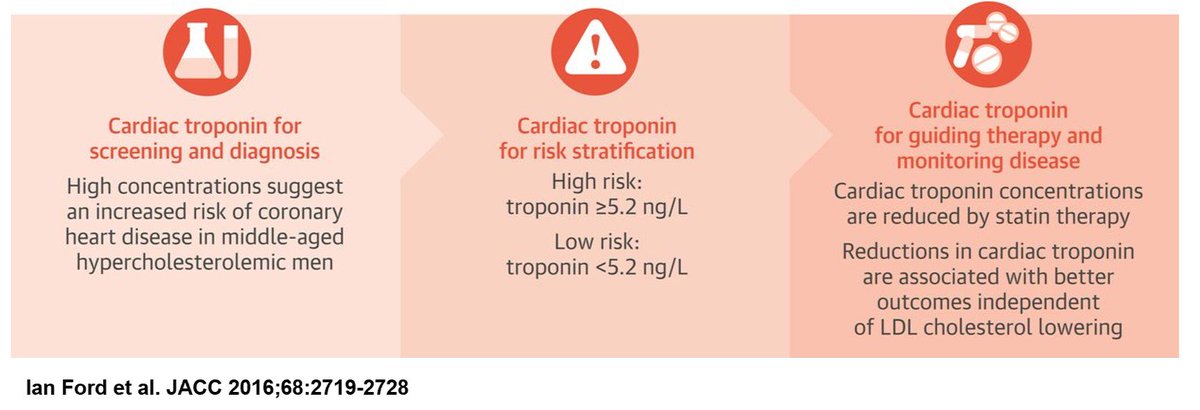
Outpatient uses of hs-troponin
✔️No standardization in assays btw centers ➡️ interpret with CAUTION
✔️Chronic elevation is bad ➡️ increased MACE ➡️ consider CV RF mod
✔️May provide prognostic info on AF stroke/bleeding risk (ESC class IIb)
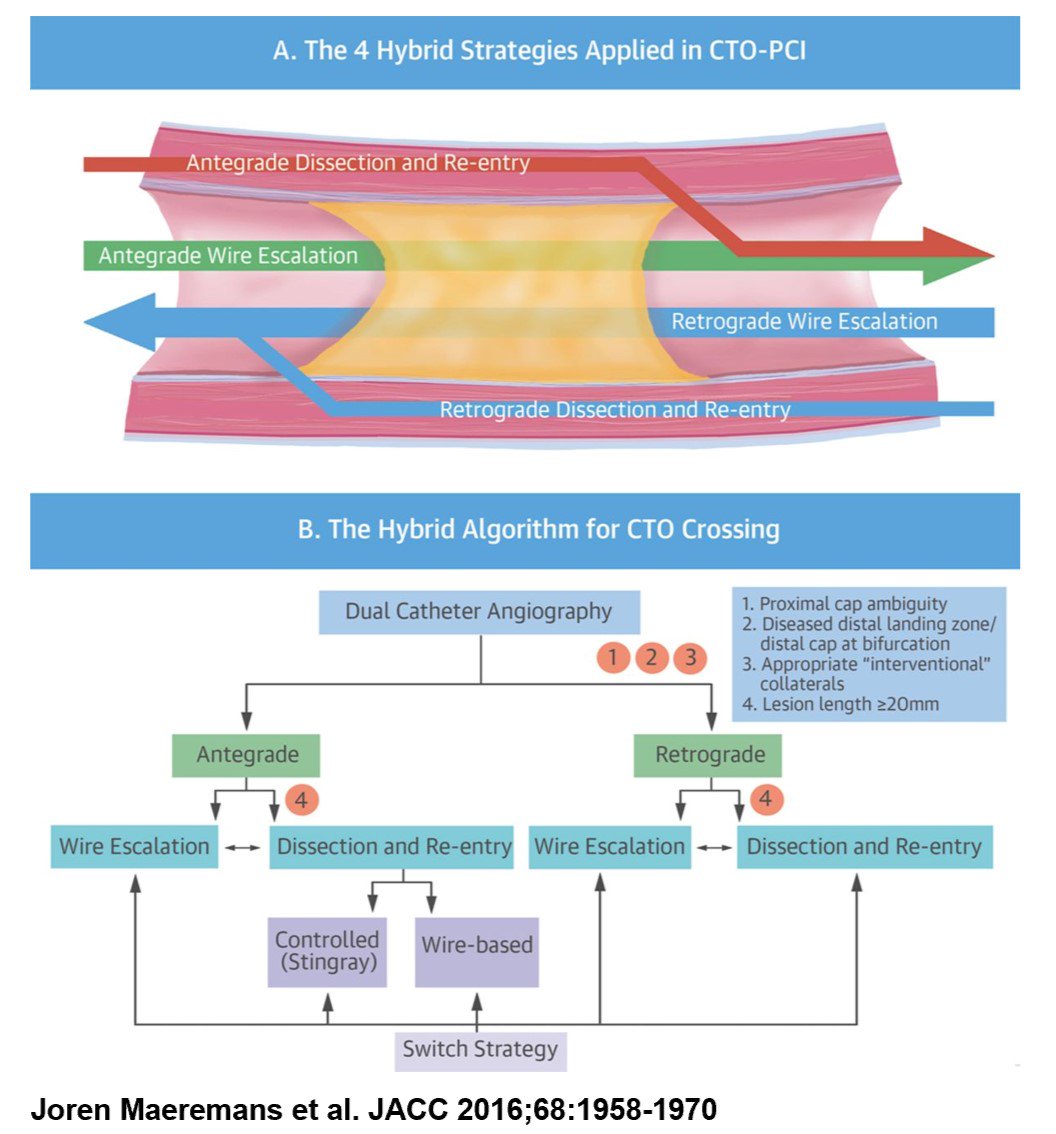
Flow and CTO:
✔️iFR compared to FFR ➡️ non-inferior ➡️ faster, cheaper, less AEs (no adenosine needed)
✔️CTO ➡️ new techniques/technology/strategy + safer ➡️ consider to improve QOL/ischemia in SELECTED patients
✔️CTO on MACE still TBD
AMI with cardiogenic shock:
✔️Culprit vessel >> multi vessel PCI (CULPRIT SHOCK)
✔️Timing, type, and benefit of temp MCS still unclear
Risk stratification for non-cardiac surgery:
✔️Most important test still H&P ➡️ find ACTIVE CV disease
✔️No active CV disease ➡️ most can go to surgery w/o further testing
✔️Testing for few patients ➡️ high risk surgery + high risk patient + poor function
Here are the combined #ActionableKnowledgeItems from this years #ACCBigSky19 cardiology conference! #CardioMedEd
@ACCinTouch @keaglemd @NMHheartdoc @MeneesMD
threadreaderapp.com/thread/1097547…